Albenza
General Information about Albenza
Albenza may interact with sure medications, so it may be very important inform your healthcare supplier of any other medicines you're taking earlier than beginning therapy. This consists of prescription medications, over-the-counter medication, and natural dietary supplements.
The energetic ingredient in Albenza, albendazole, works by stopping these worms from absorbing sugar, or glucose, from the human physique. This deprives the worms of the power they should survive and reproduce, finally resulting of their dying. This mechanism of action makes Albenza an effective therapy for a selection of worm infections.
In conclusion, Albenza is a extremely efficient medication for treating infections caused by worms. With its capability to prevent worms from absorbing sugar and depriving them of the power they want to survive, Albenza can successfully remove these infections and enhance the health and well-being of these affected. As with any medication, it is essential to use Albenza as directed, and to seek the guidance of with a healthcare supplier if any side effects or issues come up. With correct remedy, these infections can be efficiently handled and managed.
As with any treatment, Albenza might have some unwanted effects. The most commonly reported unwanted effects include stomach ache, nausea, and vomiting. Less common however extra serious unwanted effects could include allergic reactions, adjustments in vision, and liver problems. It is necessary to hunt medical attention if any of those side effects happen.
Albenza, also recognized by its generic name of albendazole, is a medicine that is generally prescribed to deal with infections caused by worms. These infections, also known as helminths, are brought on by parasitic worms that can infest the human body and trigger a range of signs.
Albenza isn't recommended to be used in pregnant girls, as it might harm the growing fetus. Women of childbearing age should use efficient birth control while taking Albenza and for at least one month after treatment has ended. It is also not really helpful for use in children underneath the age of two, except directed by a healthcare supplier.
Albenza is on the market in tablet form, and is usually taken a few times a day, depending on the precise sort of an infection being treated. It is important to observe the dosage directions as prescribed by a healthcare provider, and to finish the total course of remedy, even when symptoms improve. This will ensure that the an infection is absolutely eradicated and doesn't return.
Albenza is mostly used to treat infections brought on by three types of worms: roundworms, tapeworms, and whipworms. These infections can occur within the intestines, liver, and different tissues of the body. They are most prevalent in rural and underdeveloped areas of the world, where sanitation and hygiene practices are poor.
Symptoms of those worm infections can range depending on the kind of worm involved, however can embody stomach pain, diarrhea, and weight reduction. In severe cases, the worms can even trigger critical complications, similar to anemia and malnutrition. This is why it may be very important treat these infections promptly and effectively with drugs like Albenza.
In the postsynaptic neuron treatment sinus infection 400 mg albenza buy fast delivery, it usually does not alter the membrane potential greatly but instead changes intracellular metabolic functions that modify neuronal excitability for seconds, minutes, or perhaps even longer. Neuropeptides Neuropeptides are synthesized differently and have actions that are usually slow and in other ways different from those of the small-molecule transmitters. The neuropeptides are not synthesized in the cytosol of the presynaptic terminals. Instead, they are synthesized as integral parts of large-protein molecules by ribosomes in the neuronal cell body. The protein molecules then enter the spaces inside the endoplasmic reticulum of the cell body and subsequently inside the Golgi apparatus, where two changes occur. First, the neuropeptide-forming protein is enzymatically split into smaller fragments, some of which are either the neuropeptide itself or a precursor of it. Second, the Golgi apparatus packages the neuropeptide into minute transmitter vesicles that are released into the cytoplasm. Then, the transmitter vesicles are transported all the way to the tips of the nerve fibers by axonal streaming of the axon cytoplasm, traveling at the slow rate of only a few centimeters per day. Finally, these vesicles release their transmitter at the neuronal terminals in response to action potentials in the same manner as for small-molecule transmitters. Because of this laborious method of forming the neuropeptides, much smaller quantities of neuropeptides than the small-molecule transmitters are usually released. This difference is partly compensated for by the fact that the neuropeptides are generally a thousand or more times as potent as the small-molecule transmitters. Another important characteristic of the neuropeptides is that they often cause much more prolonged actions. Some of these actions include prolonged closure of calcium channels, prolonged changes in the metabolic machinery of cells, prolonged changes in activation or deactivation of specific genes in the cell nucleus, and/or prolonged alterations in numbers of excitatory or inhibitory receptors. Slowly acting neuro- peptide transmitters and rapidly acting, small-molecule Chapter 46 Organization of the Nervous System, Basic Functions of Synapses, and Neurotransmitters A Co-release Action potential Ca2+ Ca2+ B Co-transmission; differential Ca2+ sensitivity Single action potential Multiple action potentials Ca2+ Ca2+ synaptic vesicles of the same neuron and contribute to cotransmission of signals to a postsynaptic neuron. The co-release of transmitters and co-transmission of signals obviously has important functional implications. Each different transmitter released from the same presynaptic neuron has its own specific receptors and may have inhibitory or excitatory influences on the postsynaptic target. Different neurons may release different combinations of fast-acting transmitters that directly activate postsynaptic receptors, as well as slow-acting transmitters that require activation of second messenger cascades and postsynaptic changes in gene expression. An example of co-release of two small molecule transmitters is found in the raphe nucleus, located in the brain stem. These neurons provide innervation to several brain regions, they can co-release serotonin and glutamate, and they play an important role in the cycle of sleeping and wakefulness (see Chapters 59 and 60). Therefore, the events described in the next few sections pertain essentially to these neurons. Except for quantitative differences, they also apply to most other neurons of the nervous system. A, With co-release, both transmitters (green and purple) are stored in the same set of synaptic vesicles and released together when an action potential reaches the presynaptic terminal. B, With co-transmission, the transmitters are stored in different populations of synaptic vesicles with differential release mediated by different calcium ion (Ca2+) sensitivities; a single action potential might release one set of vesicles (green), whereas multiple action potentials might be required to release both sets of vesicles (green and purple). C, Co-transmission can also rely on the spatial segregation of vesicle populations to different boutons, allowing uniform information to be transmitted to different postsynaptic targets. This resting membrane potential is somewhat less negative than that found in large peripheral nerve fibers and in skeletal muscle fibers; the lower voltage is important because it allows both positive and negative control of the degree of excitability of the neuron. That is, decreasing the voltage to a less negative value makes the membrane of the neuron more excitable, whereas increasing this voltage to a more negative value makes the neuron less excitable. This mechanism is the basis for the two modes of function of the neuron-either excitation or inhibition-as explained in the next sections. In other cases, these transmitters may be localized in different populations of the concentration differences across the neuronal somal membrane of the three ions that are most important for neuronal function-sodium ions, potassium ions, and chloride ions. At the top of this figure, the sodium ion concentration is shown to be high in the extracellular fluid (142 mEq/L) but low inside the neuron (14 mEq/L). Distribution of sodium, potassium, and chloride ions across the neuronal somal membrane; origin of the intrasomal membrane potential. Furthermore, it shows that there is a potassium pump (the other half of the Na+-K+ pump) that pumps potassium to the interior. The membrane may be somewhat permeable to chloride ions, and there may be a weak chloride pump. Yet, most of the reason for the low concentration of chloride ions inside the neuron is the -65 mV in the neuron. That is, this negative voltage repels the negatively charged chloride ions, forcing them outward through channels until the concentration is much less inside the membrane than outside. Let us recall from Chapters 4 and 5 that an electrical potential across the cell membrane can oppose movement of ions through a membrane if the potential is of proper polarity and magnitude. Therefore, the sodium ions that leak to the interior are immediately pumped back to the exterior by the sodium pump, thus maintaining the -65-mV negative potential inside the neuron. For potassium ions, the concentration gradient is 120 mEq/L inside the neuron and 4. This concentration gradient calculates to be a Nernst potential of -86 mV inside the neuron, which is more negative than the -65 that actually exists.
As salt accumulates in the body medicine qvar inhaler order 400 mg albenza otc, it also indirectly increases the extracellular fluid volume for two basic reasons: 1. Although some additional sodium may be stored in the tissues when salt accumulates in the body, excess salt in the extracellular fluid increases the fluid osmolality. The increased osmolarity stimulates the thirst center in the brain, making the person drink extra amounts of water to return the extracellular salt concentration to normal and increasing the extracellular fluid volume. The increase in osmolality caused by the excess salt in the extracellular fluid also stimulates the hypothalamicposterior pituitary gland secretory mechanism to secrete increased quantities of antidiuretic hormone (discussed in Chapter 29). The antidiuretic hormone then causes the kidneys to reabsorb greatly increased quantities of water from the renal tubular fluid, thereby diminishing the excreted volume of urine but increasing the extracellular fluid volume. Thus, the amount of salt that accumulates in the body is an important determinant of the extracellular fluid volume. Relatively small increases in extracellular fluid and blood volume can often increase the arterial pressure substantially. This is true, however, only if the excess salt accumulation leads to an increase in blood volume and if vascular capacity is not simultaneously increased. As discussed previously, increasing salt intake in the absence of impaired kidney function or excessive formation of antinatriuretic hormones usually does not increase arterial pressure much because the kidneys rapidly eliminate the excess salt, and blood volume is hardly altered. Sequential steps whereby increased extracellular fluid volume increases the arterial pressure. Note especially that increased cardiac output has both a direct effect to increase arterial pressure and an indirect effect by first increasing the total peripheral resistance. The increased arterial pressure, in turn, increases the renal excretion of salt and water and may return extracellular fluid volume to nearly normal if kidney function is normal and vascular capacity is unaltered. Note especially in this case the two ways in which an increase in cardiac output can increase the arterial pressure. One of these is the direct effect of increased cardiac output to increase the pressure, and the other is an indirect effect to raise total peripheral vascular resistance through autoregulation of blood flow. Referring to Chapter 17, let us recall that whenever an excess amount of blood flows through a tissue, the local tissue vasculature constricts and decreases the blood flow back toward normal. This phenomenon is called autoregulation, which simply means regulation of blood flow by the tissue itself. When increased blood volume raises the cardiac output, blood flow tends to increase in all tissues of the body; if the increased blood flow exceeds the metabolic needs of the tissues, the autoregulation mechanisms constricts blood vessels all over the body, which in turn increases the total peripheral resistance. A mean arterial pressure greater than 110 mm Hg (normal is 90 mm Hg) is considered to be hypertensive. At severely high pressures- that is, mean arterial pressures 50% or more above normal-a person can expect to live no more than a few more years unless appropriately treated. Excess workload on the heart leads to early heart failure and coronary heart disease, often causing death as a result of a heart attack. The high pressure frequently damages a major blood vessel in the brain, followed by death of major portions of the brain; this occurrence is a cerebral infarct. Depending on which part of the brain is involved, a stroke can be fatal or cause paralysis, dementia, blindness, or multiple other serious brain disorders. High pressure almost always causes injury in the kidneys, producing many areas of renal destruction and, eventually, kidney failure, uremia, and death. Lessons learned from the type of hypertension called volume-loading hypertension have been crucial in understanding the role of the renalbody fluid volume mechanism for arterial pressure regulation. Volumeloading hypertension means hypertension caused by excess accumulation of extracellular fluid in the body, some examples of which follow. Experimental Volume-Loading Hypertension Caused by Reduced Kidney Mass and Increased Salt Intake. At the first circled point on the curve, the two poles of one of the kidneys were removed, and at the second circled point, the entire opposite kidney was removed, leaving the animals with only 30% of their normal renal mass. Note that removal of this amount of kidney mass increased the arterial pressure by an average of only 6 mm Hg. Because salt solution fails to quench the thirst, the dogs drank two to four times the normal amounts of volume, and within a few days, their average arterial pressure rose to about 40 mm Hg above normal. After 2 weeks, the dogs were given tap water again instead of salt solution; the pressure returned to normal within 2 days. Finally, at the end of the experiment, the dogs were given salt solution again, and this time the pressure rose much more rapidly to a high level, again demonstrating volume-loading hypertension. First, reduction of the kidney mass to 30% of normal greatly reduced the ability of the kidneys to excrete salt and water. Therefore, salt and water accumulated in the body and, in a few days, raised the arterial pressure high enough to excrete the excess salt and water intake. A week or so before the point labeled "0" days, the kidney mass had already been decreased to only 30% of normal. Then, at this point, the intake of salt and water was increased to about six times normal and kept at this high intake thereafter. The acute effect was to increase extracellular fluid volume, blood volume, and cardiac output to 20% to 40% above normal. Simultaneously, the arterial pressure began to rise but not nearly so much at first as the fluid volumes and cardiac output. The reason for this slower rise in pressure can be discerned by studying the total peripheral resistance curve, which shows an initial decrease in total peripheral resistance. This decrease was caused by the baroreceptor mechanism discussed in Chapter 18, which transiently attenuated the rise in pressure. However, after 2 to 4 days, the baroreceptors adapted (reset) and were no longer able to prevent the rise in pressure. At this time, the arterial pressure had risen almost to its full height because of the increase in cardiac output, even though the total peripheral resistance was still almost at the normal level.
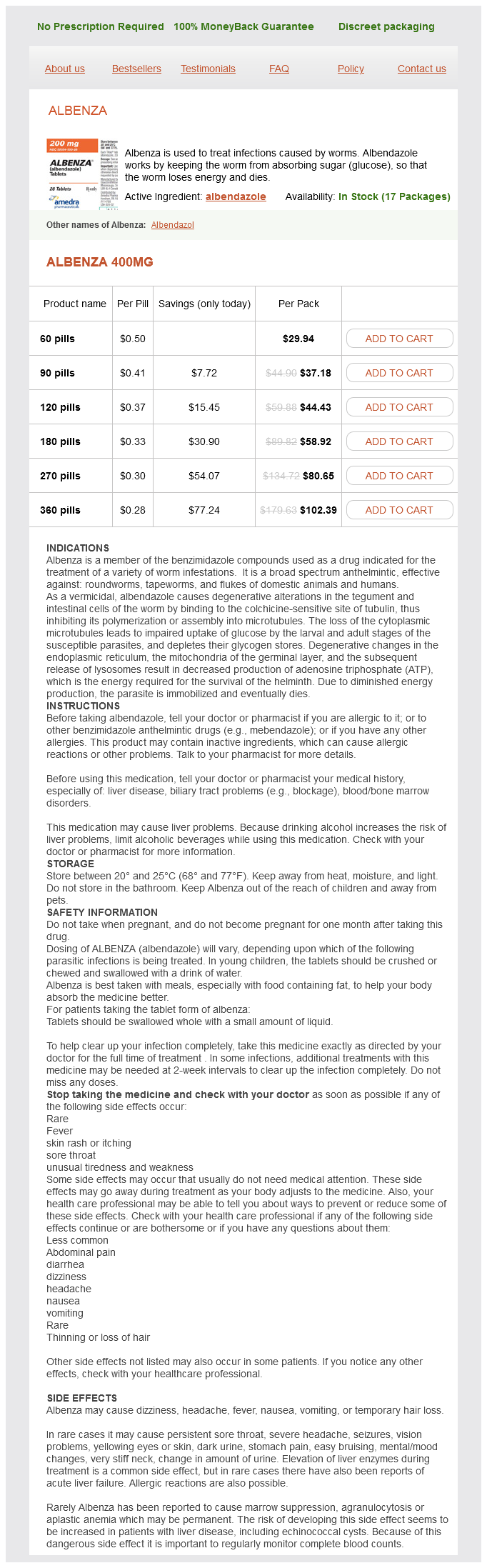
Albenza Dosage and Price
Albenza 400mg
- 60 pills - $29.94
- 90 pills - $37.18
- 120 pills - $44.43
- 180 pills - $58.92
- 270 pills - $80.65
- 360 pills - $102.39
In heavy exercise symptoms 24 hour flu cheap generic albenza canada, the arterial pressure rises by about 30% to 40%, which further increases blood flow by almost 2-fold. The increase in arterial pressure during exercise results mainly from effects of the nervous system. At the same time that the motor areas of the brain become activated to cause exercise, most of the reticular activating system of the brain stem is also activated, which includes greatly increased stimulation of the vasoconstrictor and cardioacceleratory areas of the vasomotor center. These effects rapidly increase the arterial pressure to keep pace with the increase in muscle activity. In many other types of stress besides muscle exercise, a similar rise in pressure can also occur. For example, during extreme fright, the arterial pressure sometimes rises by as much as 75 to 100 mm Hg within a few seconds. This response is called the alarm reaction, and it provides an elevated arterial pressure that can immediately supply blood to the muscles of the body that might be needed to respond instantly to enable flight from danger. Almost all these are negative feedback reflex mechanisms, described in the following sections. Baroreceptor Arterial Pressure Control System-Baroreceptor Reflexes the best known of the nervous mechanisms for arterial pressure control is the baroreceptor reflex. Basically, this reflex is initiated by stretch receptors, called baroreceptors or pressoreceptors, located at specific points in the walls of several large systemic arteries. Feedback signals are then sent back through the autonomic nervous system to the circulation to reduce arterial pressure down toward the normal level. I, Change in carotid sinus nerve impulses per second; P, change in arterial blood pressure (in mm Hg). Typical carotid sinus reflex effect on aortic arterial pressure caused by clamping both common carotids (after the two vagus nerves have been cut). Signals from the aortic baroreceptors in the arch of the aorta are transmitted through the vagus nerves to the same nucleus tractus solitarius of the medulla. Note that the carotid sinus baroreceptors are not stimulated at all by pressures between 0 and 50 to 60 mm Hg but, above these levels, they respond progressively more rapidly and reach a maximum at about 180 mm Hg. The responses of the aortic baroreceptors are similar to those of the carotid receptors except that they operate, in general, at arterial pressure levels about 30 mm Hg higher. Note especially that in the normal operating range of arterial pressure, around 100 mm Hg, even a slight change in pressure causes a strong change in the baroreflex signal to readjust arterial pressure back toward normal. Thus, the baroreceptor feedback mechanism functions most effectively in the pressure range where it is most needed. The baroreceptors respond rapidly to changes in arterial pressure; the rate of impulse firing increases in the fraction of a second during each systole and decreases again during diastole. Furthermore, the baroreceptors respond much more to a rapidly changing pressure than to a stationary pressure. That is, if the mean arterial pressure is 150 mm Hg but at that moment is rising rapidly, the rate of impulse transmission may be as much as twice that when the pressure is stationary at 150 mm Hg. The net effects are as follows: (1) vasodilation of the veins and arterioles throughout the peripheral circulatory system; and (2) decreased heart rate and strength of heart contraction. Therefore, excitation of the baroreceptors by high pressure in the arteries reflexly causes the arterial pressure to decrease because of a decrease in peripheral resistance and a decrease in cardiac output. Conversely, low pressure has the opposite effects, reflexly causing the pressure to rise back toward normal. This reduces the carotid sinus pressure; as a result, signals from the baroreceptors decrease and cause less inhibitory effect on the vasomotor center. The vasomotor center then becomes much more active than usual, causing the aortic arterial pressure to rise and remain elevated during the 10 minutes that the carotids are occluded. Removal of the occlusion allows the pressure in the carotid sinuses to rise, and the carotid sinus reflex now causes the aortic pressure to fall almost immediately to slightly below normal as a momentary overcompensation and then return to normal in another minute. The ability of the ba- After the baroreceptor signals have entered the nucleus tractus solitarius of the medulla, secondary signals inhibit 222 roreceptors to maintain relatively constant arterial pressure in the upper body is important when a person stands up after lying down. Immediately on standing, the arterial pressure in the head and upper part of the body tends to fall, and marked reduction of this pressure could cause loss of consciousness. However, the falling pressure at the baroreceptors elicits an immediate reflex, resulting in strong sympathetic discharge throughout the body that minimizes the decrease in pressure in the head and upper body. Frequency distribution curves of the arterial pressure for a 24-hour period in a normal dog and in the same dog several weeks after the baroreceptors had been denervated. Two-hour records of arterial pressure in a normal dog (top) and in the same dog (bottom) several weeks after the baroreceptors had been denervated. Because the baroreceptor system opposes in- creases or decreases in arterial pressure, it is called a pressure buffer system, and the nerves from the baroreceptors are called buffer nerves. The upper panel in this figure shows an arterial pressure recording for 2 hours from a normal dog, and the lower panel shows an arterial pressure recording from a dog whose baroreceptor nerves from the carotid sinuses and the aorta had been removed. Note the extreme variability of pressure in the denervated dog caused by simple events of the day, such as lying down, standing, excitement, eating, defecation, and noises. Note that when the baroreceptors were functioning normally, the mean arterial pressure remained within a narrow range of between 85 and 115 mm Hg throughout the day and, for most of the day, it remained at about 100 mm Hg. After denervation of the baroreceptors, however, the frequency distribution curve flattened, showing that the pressure range increased 2. Thus, one can see the extreme variability of pressure in the absence of the arterial baroreceptor system. One reason that the baroreceptors have been considered by some physiologists to be relatively unimportant in chronic regulation of arterial pressure is that they tend to reset in 1 to 2 days to the pressure level to which they are exposed. That is, if the arterial pressure rises from the normal value of 100 to 160 mm Hg, a very high rate of baroreceptor impulses is at first transmitted. Then, it diminishes much more slowly during the next 1 to 2 days, at the end of which time the rate of firing will have returned to nearly normal, despite the fact that the mean arterial pressure still remains at 160 mm Hg.