Aleve
General Information about Aleve
It is a broadly known proven truth that managing ache is crucial in promoting overall well-being and Aleve plays a major position on this. Whether it's for acute or chronic ache, Aleve has been proven to be an effective and safe option when taken as directed. In truth, a examine printed in the British Journal of Clinical Pharmacology found that Aleve was equally effective as different commonly used pain relievers, but with a decrease danger of side effects. This gives customers peace of mind knowing they can find aid without having to worry about potential adverse reactions.
Pain is a universal experience that we've all handled sooner or later in our lives. From complications to muscle cramps, pain can be a debilitating condition that impacts our day by day activities and quality of life. As a result, many individuals turn to over-the-counter medicines to search out reduction. One such treatment is Aleve, a preferred ache reliever that has been trusted by tens of millions of individuals worldwide.
Aleve, also recognized by its generic name naproxen, is a non-steroidal anti-inflammatory drug (NSAID) commonly used to treat a selection of situations together with arthritis, ankylosing spondylitis, tendinitis, bursitis, gout, and menstrual cramps. It is available in both prescription and over-the-counter varieties, making it simply accessible to these in need of fast-acting pain relief.
While Aleve is generally protected and well-tolerated, it is essential to focus on potential unwanted effects. These could include abdomen upset, heartburn, headache, nausea, and dizziness. In uncommon instances, it could also cause serious unwanted facet effects, together with liver or kidney problems, allergic reactions, and elevated risk of heart attack or stroke. It is crucial to follow the recommended dosage and speak to a healthcare professional if any regarding unwanted aspect effects occur.
In conclusion, Aleve is a trusted and efficient pain reliever that has been providing reduction to tens of millions of people for many years. Its long-lasting results and varied strengths make it a handy option for these on the lookout for focused reduction. However, as with every treatment, it is essential to use it responsibly and seek the guidance of with a healthcare skilled when wanted. With correct use, Aleve might help us handle ache and enhance our quality of life. So the following time you experience ache, contemplate Aleve as a safe and effective choice for aid.
The lively ingredient in Aleve, naproxen, works by blocking the production of certain chemical substances within the physique that trigger inflammation and ache. This helps to reduce back swelling and ease discomfort related to numerous situations. Aleve is available in several types such as tablets, liquid gels, and caplets, making it handy for individuals to choose the form that works greatest for them.
One of the principle advantages of Aleve is its long-lasting aid. While different ache relievers might only last for a couple of hours, Aleve can provide aid for up to 12 hours, making it a well-liked choice for those with continual pain. This signifies that individuals can take it less frequently, which can help cut back the risk of potential side effects related to overuse of pain medication.
Another benefit of Aleve is that it is obtainable in different strengths, which permits for personalised dosing based mostly on a person's needs. This implies that for minor aches and pains, a lower strength could also be adequate, whereas the next energy may be needed for more extreme circumstances. However, it could be very important seek the advice of with a healthcare skilled when figuring out the suitable dose as taking an excessive quantity of of any medicine can have adverse results.
In this case pain treatment guidelines 2014 order aleve discount, the right femoral vein provides reliable direct access to the inferior vena cava and avoids the problem of navigating the venous cannula across the inferior vena caval bifurcation from the left side. If severe aortic regurgitation is present and the sternum cannot be opened safely, then a small left anterolateral thoracotomy can be performed to provide access to the apex of the left ventricle for venting. Systemic core cooling progresses at a rate of around 1°C/min and may take as long as 30 minutes to reach 16°C. The heart may fibrillate at around 25°C at which point it is important to avoid left ventricular distension. In the presence of aneurysmal aortic sinuses, it may be possible to clamp the previous ascending aortic graft or native ascending aorta in order to correct the root pathology during systemic cooling. In this case, the ascending aorta and root are opened and myocardial protection is obtained with antegrade cardioplegia. Myocardial temperature is kept below 10°C by reinfusion of cardioplegia every thirty minutes. The jet from the femoral cannula displaced emboli from the aneurysmal abdominal aorta. These occluded the cerebral circulation before the brain was cooled and before retrograde cerebral perfusion could wash them out. During circulatory arrest, the patient is placed in the Trendelenburg position and the venous blood drained into the pump oxygenator. The aneurysm is then opened widely and, if not undertaken previously, cardioplegia is delivered antegrade into the coronary ostia. Venous pressure in the innominate vein should be kept below 20 mmHg to reduce the risk of cerebral edema. Superior vena caval flow is kept at about 250 ml/min (or less if the venous pressure reaches 20 mmHg). The aortic arch resection is undertaken with careful definition of the arch anatomy and the relationship between the true and false aortic lumens and the origins of the brachiocephalic vessels. Usually, this begins with a longitudinal incision in the mid-ascending aorta, followed by transection of the whole aorta just proximal to the innominate artery. During this process, every attempt is made to preserve the phrenic and recurrent laryngeal nerves. If the dissection extends into the innominate or left carotid artery, it is unwise to direct the blood flow exclusively into the true lumen since the false lumen may be responsible for some of the distal blood flow. In either case, the septum within each dissected branch is incised for a distance of approximately 10 mm, then resected to avoid leaving a mobile and potentially obstructive flap. When the circle of Willis is intact, this method provides satisfactory cerebral perfusion during arch repair. Distal aortic resection is then carried out to either completely excise the aneurysm or prepare the distal aorta for an elephant trunk. The septum between the true and false lumens is incised longitudinally along its borders as far distally as can be visualized. This avoids redirecting distal aortic flow preferentially into either lumen, since the false channel may give rise to important visceral or spinal branches downstream. Excision of the flap must extend over a greater length than the elephant trunk to avoid kinking of the Dacron tube. The graft size is selected according to the dimensions of the descending thoracic aorta. This should not exceed 12 cm in length in order to avoid occlusion of distal aortic branches. The invaginated graft is inserted into the descending aorta so that the distal aortic anastomosis is made between the double-fold of the Dacron graft and the dissected descending aorta. The suturing is accomplished precisely under direct vision in a full-thickness manner. If the wall of the false lumen is fragile, an external Teflon strip may be used for reinforcement. Teflon is also advisable when the aortic diameter is much larger than that of the graft. When this anastomosis is completed, the stay-suture on the invaginated part of the graft is pulled out to withdraw the aortic arch limb. The elephant trunk in the descending aorta is then inspected for kinks and access into both true and false lumens distally. Reconnection of the brachiocephalic vessels There are a variety of methods with which to reconnect the head vessels. This involves a single circumferential anastomosis around the button into a window of approximately 3. In straightforward cases, the elephant trunk anastomosis, and reimplantation of the brachiocephalic vessels can be performed within the 30 minutes of safe circulatory arrest time. With a clamp on the proximal end of the graft, perfusion is restored to the arch and distal aorta before completing the proximal anastomosis to the ascending aorta. In this case, the origins of the brachiocephalic vessels are resected back to undissected margins and then anastomosed in serial fashion to the branched graft. Circulatory arrest of more than 30 minutes is associated with cognitive impairment. More than 40 minutes provides increased stroke rate, and ischemia extending to 60 minutes results in decreased survival. Time is therefore an important determinant as to how the cerebral vessels are reconnected.
The use of tissue expanders in immediate breast reconstruction following mastectomy for cancer low back pain treatment guidelines generic aleve 500 mg buy line. Incidence of autoimmune disease in patients after breast reconstruction with silicone gel implants versus autogenous tissue: a preliminary report. Lack of cyclin E immunoreactivity in non-malignant breast and association with proliferation in breast cancer. Microscopic localization of calcifications in and around breast carcinoma: a cautionary note for needle core biopsies. Immunohistochemical localization of gross cystic disease fluid protein-15, -24 and -44 in ductal 2350. Androgen receptor expression in ductal carcinoma in situ of the breast: relation to oestrogen and progesterone receptors. Phase 2 randomized trial of primary endocrine therapy versus chemotherapy in postmenopausal patients with estrogen receptor-positive breast cancer. Cutaneous angiosarcoma of the breast after segmental mastectomy and radiation therapy. Too close for comfort: accidental burn following subcutaneous mastectomy and immediate implant reconstruction. Case report and dosimetric analysis of an axillary recurrence after partial breast irradiation with mammosite catheter. Immunohistochemistry increases the accuracy of diagnosis of benign papillary lesions in breast core needle biopsy specimens. Failure of high risk women to produce nipple aspirate fluid does not exclude detection of cytologic atypia in random periareolar fine needle aspiration specimens. Genome-wide search for loss of heterozygosity using laser capture microdissected tissue of breast carcinoma: an implication for mutator phenotype and breast cancer pathogenesis. Genetic polymorphisms in the cyclooxygenase-2 gene, use of nonsteroidal anti-inflammatory drugs, and breast cancer risk. Intratumoral concentration of sex steroids and expression of sex steroid-producing enzymes in ductal carcinoma in situ of human breast. Cyclooxygenase-2 expression is related to nuclear grade in ductal carcinoma in situ and is increased in its normal adjacent epithelium. Screeningdetected and symptomatic ductal carcinoma in situ: differences in the sonographic and pathologic features. Ultrasonographic detection of occult cancer in patients after surgical therapy for breast cancer. Excisional biopsy should be performed if lobular carcinoma in situ is seen on needle core biopsy. Carcinoma arising from preexisting pregnancy-like and cystic hypersecretory hyperplasia lesions of the breast: a clinicopathologic study of 9 patients. Interobserver variability in the classification of proliferative breast lesions by fine-needle aspiration: results of the Papanicolaou Society of Cytopathology Study. Breast cancer diagnosis and prognosis in women augmented with silicone gel-filled implants. Upright stereotactic vacuumassisted needle biopsy of suspicious breast microcalcifications. Fibroadenomas with atypia: causes of under- and overdiagnosis by aspiration biopsy. Calcium oxalate crystals (Weddellite) within the secretions of ductal carcinoma in situ-a rare phenomenon. Novel translational model for breast cancer chemoprevention study: accrual to a presurgical intervention with tamoxifen and N-[4hydroxyphenyl] retinamide. AlphaB-crystallin: a novel marker of invasive basallike and metaplastic breast carcinomas. Sclerosing polycystic adenosis of parotid gland with dysplasia and ductal carcinoma in situ. Aldosterone acts upon the distal convoluted tubule and cortical collecting duct of the kidney to increase sodium reabsorption in exchange for potassium and hydrogen ion, which are excreted in the urine. Plasma renin levels generally are decreased as the body attempts to suppress the renin-angiotensin system. A pheochromocytoma (a catecholaminesecreting tumor, usually in the adrenal medulla) can cause high levels of circulating catecholamines (both epinephrine and norepinephrine). This condition leads to adrenoceptormediated systemic vasoconstriction and 1-adrenoceptor-mediated cardiac stimulation that can cause substantial elevations in arterial pressure. Although arterial pressure rises to very high levels, tachycardia still occurs because of the direct effects of the catecholamines on the heart and vasculature. Excessive 1-adrenoceptor stimulation in the heart often leads to arrhythmias in addition to the hypertension. Aortic coarctation is a narrowing of the aortic arch usually just distal to the left subclavian artery. It is a congenital defect that obstructs aortic outflow, leading to elevated pressures proximal to the coarctation. Distal pressures, however, are not necessarily reduced as would be expected from the hemodynamics associated with a stenosis. The reason for this is that reduced systemic blood flow, and in particular reduced renal blood flow, leads to an increase in the release of renin and an activation of the renin-angiotensinaldosterone system. Although the aortic arch and carotid sinus baroreceptors are exposed to higher-than-normal pressures, the baroreceptor reflex is blunted owing to structural changes in the walls of vessels where the baroreceptors are located. Furthermore, baroreceptors become desensitized to chronic elevation in pressure and become "reset" to the higher pressure.
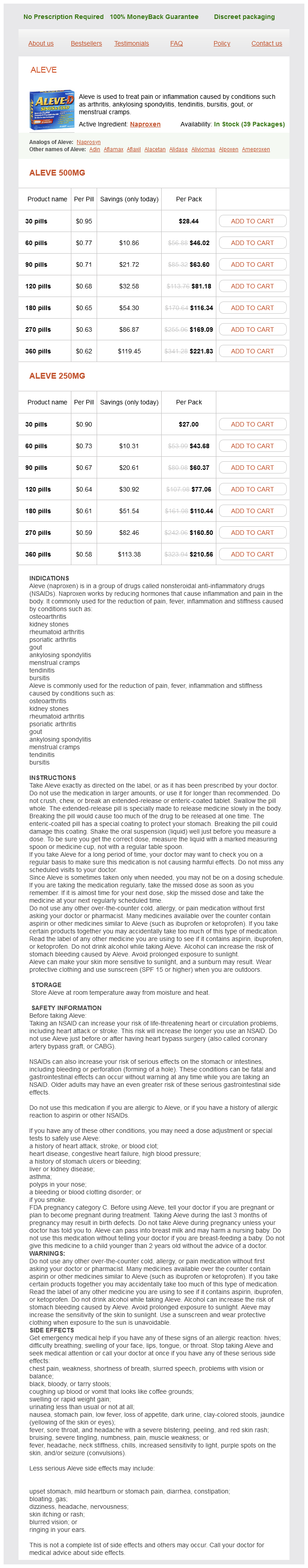
Aleve Dosage and Price
Aleve 500mg
- 30 pills - $28.44
- 60 pills - $46.02
- 90 pills - $63.60
- 120 pills - $81.18
- 180 pills - $116.34
- 270 pills - $169.09
- 360 pills - $221.83
Aleve 250mg
- 30 pills - $27.00
- 60 pills - $43.68
- 90 pills - $60.37
- 120 pills - $77.06
- 180 pills - $110.44
- 270 pills - $160.50
- 360 pills - $210.56
The overabundance of glucose drives the anaerobic glycolysis cycle and leads to faster accumulation of lactate and intracellular acidosis during the arrest interval unifour pain treatment center nc purchase cheap aleve on line. We use intravenous insulin drip to maintain normoglycemia intra- and post-operatively. Detailed analysis of the plethora of agents that have experimental or clinical relevance is beyond the scope of this discussion. Although there are several agents found to be experimentally effective in blocking some of the known specific pathways that lead to neuronal injury, such as glutamate antagonists or receptor blockers, sodium channel blockers (lamotrigine), nitric oxide synthase inhibitors, free radical scavengers (superoxide dismutase), and non-specific cytoprotective agents (Poloxamer 188), none have found any useful clinical application because of either unacceptable side effects and/or clinical toxicity. Cerebral ischemia causes a rapid shift of calcium from the extracellular space into the cells. Some authors have favored the use of nicardipine that directly reduces this influx [95]. Others have incorporated the use of lidocaine as an adjunct in reducing cerebral metabolism. Steroids are used in all patients as membrane stabilizers and also to reduce cerebral edema [94]. In all patients with anticipated arrest times of greater than 30 minutes, 1 g of methylprednisolone is given prior to arrest. It is continued in the first 48 hours post-arrest (125 mg every 6 h for 24 h; then 125 mg every 12 h for the next 24 h). In patients with actual arrest times of less than 30 minutes, the post operative doses are omitted. Mannitol, besides reducing cerebral edema and intracranial pressure, has an important effect as a free radical scavenger [97] and is given in standard doses both during the cooling and rewarming periods. We had used barbiturates as an adjunct for cerebral protection in our early experience, but have abandoned their use mainly because of their myocardial depressant effect in the high doses required. Others continue to incorporate highdose thiopental in their protective regimen [46]. Use of antifibrinolytic agents, such as lysine analogs (-aminocaproic acid or tranexamic acid) or the serine protease inhibitor, aprotinin, is effective in reducing blood loss following cardiopulmonary bypass. We further fine-tune the heparin levels by their direct measurement 148 with a heparin-protamine titration device. The discussion of clinical use of aprotinin cannot be complete without consideration of the recent comparative analysis of the use of aprotinin, tranexamic acid, and -aminocaproic acid in a large cohort of patients who underwent myocardial revascularization [104]. This study showed a significant association with aprotinin use and the risk of end-organ damage. Also, strikingly, aprotinin was not any more effective in reducing blood loss than the other studied antifibrinolytic agents. We believe that in spite of its limitations, the study findings are convincing enough to prompt a change in our practice. Our implementation of several strategies, in addition to routine use of antifibrinolytics, has eliminated the need for transfusion of blood and blood products in the majority of these cases. For example, autologous blood is removed (in quantities determined by the desired level of hemodiluton) prior to initiating cardio-pulmonary bypass and reinfused following administration of protamine. Also, the targeted use of blood products is guided by routine perioperative thromboelastography. The transfusion rate (blood or blood products) is far lower in elective cases (15%). Conclusion Hypothermic circulatory arrest remains an important element of all contemporary methods of cerebral protection used in the surgery of the aortic arch. Increasing understanding of the physiology of hypothermia and nervous system ischemia has helped in the development of improved methods of brain protection. Determination of optimal perfusion flow rate for deep hypothermic cardiopulmonary bypass in the adult based on distributions of blood flow and oxygen consumption. Relationship of brain blood flow and oxygen consumption to perfusion flow rate during profoundly hypothermic cardiopulmonary bypass. Neurologic outcome after ascending aorta-aortic arch operations: effect of brain protection technique in high-risk patients. Hyperglycemia increases cerebral intracellular acidosis during circulatory arrest [published erratum appears in Ann Thorac Surg 1993; 55: 1054]. Involvement of apoptosis in neurological injury after hypothermic circulatory arrest: a new target for therapeutic intervention Leukocyte filtration improves brain protection after a prolonged period of hypothermic circulatory arrest: a study in a chronic porcine model. Neuronal nitric oxide synthase inhibition reduces neuronal apoptosis after hypothermic circulatory arrest. Deep hypothermic circulatory arrest and global reperfusion injury: avoidance by making a pump prime reperfusatea new concept. Conditioned blood reperfusion markedly enhances neurologic recovery after prolonged cerebral ischemia. Postoperative hypoxemia exacerbates potential brain injury after deep hypothermic circulatory arrest. Regional glucose utilization and blood flow following graded forebrain ischemia in the rat: correlation with neuropathology. Neuronal damage after hypothermic circulatory arrest and retrograde cerebral perfusion in the pig. The relationship among canine brain temperature, metabolism, and function during hypothermia. Assessment of cerebral blood flow with transcranial Doppler in right brachial artery perfusion patients. Biochemical serum markers for brain damage: a short review with emphasis on clinical utility in mild head injury. Serum S100 protein: a potential marker for cerebral events during cardiopulmonary bypass. S100beta correlates with neurologic complications after aortic operation using circulatory arrest.