Alphagan
General Information about Alphagan
One of the numerous advantages of Alphagan is that it's effective in patients with extensive or hypertension in the eye. This situation, often identified as ocular hypertension, is a precursor to glaucoma and requires treatment to prevent the event of the disease. The medicine can be generally utilized in sufferers who usually are not responding well to different glaucoma medications.
In addition to Alphagan, there are numerous other glaucoma medications out there, such as beta-blockers, prostaglandin analogs, and carbonic anhydrase inhibitors. The selection of medicine depends on the kind and severity of the glaucoma, in addition to the patient's medical history. Alphagan can also be prescribed together with different glaucoma medicines for maximum efficacy.
In conclusion, Alphagan is a extensively used and efficient treatment for the therapy of glaucoma. It helps to reduce intraocular strain, protecting the optic nerve and stopping imaginative and prescient loss. As with any medicine, it is important to comply with the prescribed dosage and inform your physician of any side effects. Regular eye exams and correct adherence to remedy may help manage glaucoma and protect your vision for years to return.
Alphagan is a generally prescribed medicine that is used to minimize back intraocular strain in patients with glaucoma. Glaucoma is a watch disease that impacts the optic nerve and can result in permanent vision loss if left untreated. Intraocular strain, also referred to as IOP, is the stress throughout the eye and is a serious threat factor for creating glaucoma. Alphagan helps to lower the IOP, thereby slowing down the progression of glaucoma and protecting the affected person's imaginative and prescient.
Alphagan belongs to a category of drugs referred to as alpha-adrenergic agonists. It works by decreasing the production of aqueous humor, the fluid that circulates inside the eye, thereby reducing intraocular strain. It also will increase the drainage of this fluid from the attention, further reducing the strain. This twin mechanism of action makes Alphagan a potent weapon towards glaucoma.
Patients with glaucoma usually have excessive IOP as a outcome of a blockage within the drainage system of the attention, which prevents the fluid from flowing out properly. As a end result, the fluid builds up, causing the pressure to rise. If this pressure stays high for an prolonged period, it could damage the optic nerve and result in blindness. Alphagan helps to lower the IOP, lowering the danger of nerve injury.
Glaucoma is a condition that impacts tens of millions of individuals worldwide, and the numbers are only expected to increase because the population ages. It is sometimes called the 'silent thief of sight' as a result of it develops progressively and without any noticeable symptoms until significant damage has already occurred. This is why early detection and remedy of glaucoma are crucial in preventing vision loss. Alphagan is probably considered one of the many medicines used to treat glaucoma, and it has been proven to be effective in controlling the disease.
Alphagan is out there within the form of eye drops and is usually utilized two to 3 instances a day, depending on the severity of the condition. It is essential to comply with the prescribed dosage and frequency to make sure efficient remedy. The drops are applied immediately into the eye, and sufferers might experience a slight stinging sensation or redness, which is regular and may subside quickly.
As with any treatment, Alphagan may cause side effects in some individuals, together with complications, dry mouth, blurred vision, and drowsiness. Most of these side effects are mild and often resolve on their own. However, patients should inform their physician if they expertise any persistent or extreme discomfort.
Lesions can be of three types: erythematous lesions medicine 665 discount alphagan, discoid lesions and ulcers; and may coexist [180,184]. The morphological spectrum varies, for example in acute mucosal lesions, erythematous macules, palatal erythema, ulcers, blisters or erosions may predominate [107]. Discoid lesions begin as erythematous papules, which enlarge into chronic plaques [185], usually appearing as erythematous central areas surrounded by welldemarcated, irregular, white borders and telangiectasia [184,186]. Chelitis also occurs in approximately 6%, the lips having a silvery appearance, with erythema, scaling and blurring of the vermilion border [188]. Given the potential risk of transformation to squamous cell carcinoma in these patients, mucosal biopsy should be considered in any non healing or irregularly ulcerated lesion. Involvement of the joints occurs at some time in approximately 90% of patients, arthralgia being more common than arthritis. A rheumatoidlike deformity is present in approximately 25% of patients, with marked softtissue swelling, especially of the dorsa of the fingers, hands and wrists, although joint erosions on Xray are not a feature. The deformity is usually less, but the soft tissue swelling is more marked than in rheumatoid arthritis. Rarely, erosive symmetrical polyarthritis with rheumatoid arthritislike deformities, termed rhupus, can occur [201]. These patients may be distinguished from those with lupus arthropathy due to the presence of anticyclic citrullinated peptide antibodies [202]. Many patients suspected of having a connective tissue disease may, even after thorough investigation, present problems of categorization. The progressive rheumatoid arthritislike deformities in this syndrome are due to tenosynovitis rather than the synovial inflammation seen in rheumatoid arthritis. The elbows, shoulders, knees and feet may also be involved and softtissue nodules may occur, usually indicating calcinosis. Muscle pain occurs in approximately 50% of patients, and this may be confused with the pain of arthritis. Muscle weakness is a less common feature, and can by related to steroid myopathy or other drug effects. Inflammatory myopathy occurs in 510% of patients and is indistinguishable from idiopathic inflammatory myopathy [206]. An interruption of blood flow to the bony epiphysis results in bone necrosis and subchondral fractures. Risk factors include the presence of the Raynaud phenomenon, vasculitis, antiphospholipid syndrome and glucocorticoid use. Glucocorticoids are thought to promote adipogenesis and fatty infiltration of osteocytes, enhancing apoptosis. Glucocorticoid dose and length of use correlate with the risk of avascular necrosis. The femoral head or condyle is most frequently involved [209], but the condition also may involve the knees, ankles, humerus, metatarsals and carpal bones. The diagnosis should be considered in patients with persistent pain over one or several joints, when there is little activity in other systems. Surgical management options include core decompression, bone grafting and joint replacement. The condition is thought to be associated with increased pressure in the bone marrow because of altered venous drainage, and core decompression may be successful [211]. Factors contributing to bone loss include chronic inflammation, glucocorticoid use, renal dysfunction, vitamin D deficiency, ovarian failure and concomitant thyroid disease. The identification of risk factors, regular bone mineral density measurement and appropriate therapy are critical. Pleurisy and pericarditis have a prevalence of 17% at disease onset and a cumulative incidence of 36% [214]. Patients with pericarditis typically present with tachycardia, substernal chest discomfort and positional pain [213]. Clinically significant valvular dysfunction secondary to LibmanSacks endocarditis occurs in just 12% of patients [215]. Both systolic and diastolic murmurs may be found depending upon the site of the lesion, and bacterial endocarditis can occur on the damaged heart valves. Treatment with corticosteroids increases the risk of developing coronary artery disease by contributing to hyperlipidaemia, hypertension and weight gain, such that patients on 30 mg of prednisolone have a 60% greater 2year risk of cardiovascular events compared with disease activitymatched patients no taking corticosteroids [218]. The myocardium may also be affected, resulting in cardiac failure, but this is rare [219]. Transient pleurisy is the most common feature, and in approximately twothirds of these cases some fluid develops, occasionally haemorrhagic. Diffuse pulmonary haemorrhage [223] and pulmonary infections must be considered within the differential diagnosis [220]. Pulmonary hypertension occurs rarely compared with systemic sclerosis and is likely multifactorial, with factors including vasospasm, vasculitis and thrombotic occlusion. The need for regular screening by urinalysis, blood pressure monitoring, assessment of renal function and early renal biopsy is critical [227]. The course is variable, and albuminuria and casts may persist for years without marked deterioration in renal function. Kidney damage, if this is going to develop, usually appears early (within the first 3 years) and is more frequent and severe in younger patients [227]. Thus, a renal biopsy in every patient with haematuria, proteinuria or elevation of serum creatinine is advised [226]. Gastrointestinal symptoms occur in about 50% of patients but are usually mild with anorexia, nausea and vomiting being the most frequent.
Electron microscopy of the skin often shows cytoplasmic vacuoles treatment tracker buy alphagan us, particularly in endothelial cells, fibroblasts, Schwann cells and the myoepithelial cells of sweat glands [6,7]. Angiokeratomas appear in mid to late childhood and are present in 85% of patients aged over 20 years [8]. Patients have developmental delay in childhood and regress after puberty, eventually becoming severely retarded. There is gradual coarsening of the facial features, with sagging skin, thick lips, a broad low nasal bridge and coarse hair. Facial angiofibromas are common in adults, as are gingival overgrowths and oedema of the buccal mucosa [9]. It has been reported in infants with neurodegeneration (Schindler disease) and in adults with angiokeratomas and mild learning difficulties (Kanzaki disease). The angiokeratomas may have a similar distribution to Fabry disease, or they may be more widespread, including across the breasts, extremities, face, lips, mouth and gastric mucosa [6]. They also have gum hypertrophy, severe neurological involvement, dysostosis multiplex and cardiomyopathy. Enzyme replacement therapy is being developed for mannosidosis and bone marrow transplantation may improve the neurological outcome in fucosidosis. Investigations the diagnosis is established by demonstrating raised levels of the mistargeted lysosomal enzymes in plasma. Skin histology reveals membranebound vacuoles and cytoplasmic bodies in fibroblasts and other mesenchymal cells. Sphingolipidoses Introduction and general description Sphingolipids are amphiphilic molecules found in cell membranes. They are degraded by lysosomal hydrolases and deficiencies of these enzymes (or their protector proteins) cause the sphingolipidoses. TaySachs disease), problems are confined to the nervous system: these are not considered further here. The clinical and biochemical features of sphingolipidoses with dermatological features are included in Table 81. It is classified clinically into three types, of which type I (nonneuronopathic) is much the commonest [12]. This presents in children or adults with hepatosplenomegaly, thrombocytopenia (due to hypersplenism) or bone problems (ischaemic crises, bone pain or pathological fractures). Cutaneous features are common in type I but not troublesome and include diffuse yellowbrown pigmentation, easy tanning, brown macules and telangiectasia [13]. The baby is encased in thick, tight, shiny skin that cracks and desquamates to leave erythroderma [14]. Type A usually presents in early infancy with diarrhoea and vomiting, poor weight gain, hepatosplenomegaly and neurological problems; these patients die by 3 years of age. Less severely affected type A patients have juvenile or adultonset neurological disease. Type B patients present as children or adults with splenomegaly or hepatosplenomegaly; complications include interstitial lung disease, poor growth, hyperlipidaemia and thrombocytopenia. The skin may be involved in types A or B, with patches of waxy induration and brownish yellow pigmentation. Severe cases present as neonates with hydrops fetalis or hypotonia, hepatosplenomegaly and facial dysmorphism (including macroglossia, gum hypertrophy and a depressed nasal bridge). The mildest cases present in late childhood with dysarthria, dystonia and skeletal dysplasia (affecting the spine and hip). Telangiectasia and extensive Mongolian blue spots have also been reported in infantile cases. Patients usually present in early infancy with a hoarse cry, painful swollen joints and subcutaneous nodules. The most commonly affected joints are those of the hand and wrist, elbows, knees and ankles. The subcutaneous nodules may be associated with erythematous papules and are generally close to affected joints and over pressure points, such as the occiput and lower spine. Histology reveals granulomas containing large, foamy histiocytes; electron microscopy shows that these have cytoplasmic vacuoles containing curvilinear inclusions (Farber bodies) [17]. Most patients have psychomotor retardation, poor weight gain and die in early childhood from respiratory infections. Introduction and general description this is a rare Xlinked lysosomal storage disorder, characterized by angiokeratomas and multisystem complications [19]. Affected males usually present in childhood with episodes of pain in the extremities, followed by the appearance of angiokeratomas. Many heterozygous females also develop symptoms, although the onset is usually later. Pathophysiology A deficiency of galactosidase A prevents the degradation of glycosphingolipids with terminal galactose residues, predominantly globotriaosylceramide (Gb3). Gb3 accumulation in vascular endothelial, perithelial and smooth muscle cells leads to aneurysmal dilatation of blood vessels, ischaemia and infarction. Glycosphingolipids also accumulate in the renal glomeruli and tubules, cardiac muscle, autonomic ganglion cells and corneal epithelium. Investigations the diagnosis is established by enzyme assays on leukocytes (or cultured cells). NiemannPick cells are typical examples large, usually mononucleate histiocytes, whose cytoplasm is filled with lipid droplets; they stain readily with Sudan stains and contain doubly refractile material. Ultrastructurally, the cytoplasm of Niemann Pick cells contains granular lipid inclusions that may appear lamellar [15]. Ultrastructurally, Gaucher cells have vesicles that contain twisted tubular structures [18].
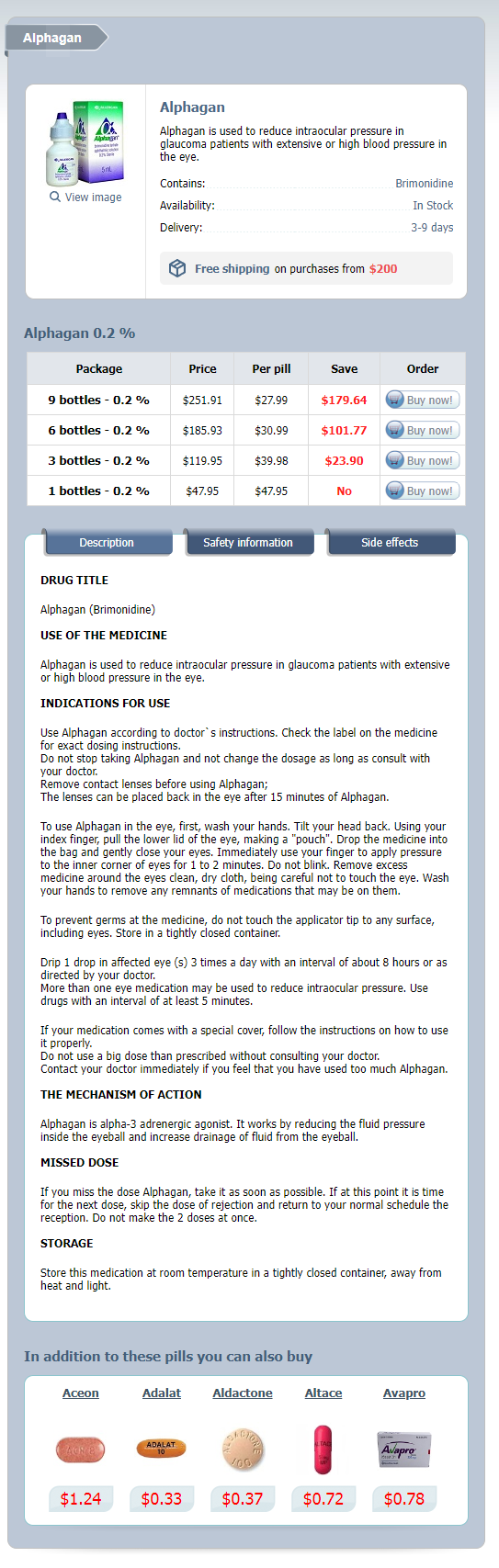
Alphagan Dosage and Price
Alphagan 0.2 %
- 9 bottles - $251.91
- 6 bottles - $185.93
- 3 bottles - $119.95
- 1 bottles - $47.95
Palmoplantar keratoderma and neurological manifestations this category largely overlaps with the neuroichthyotic syndromes medicine symbol purchase alphagan 0.2% overnight delivery, These include striate keratoderma with spastic paraplegia, pes cavus and mental retardation in four brothers [1]; autosomal dominant punctate keratoderma and spastic paralysis [2]; autosomal dominant focal keratoderma with nail dystrophy and motor and sensory neuropathy [3]; and CharcotMarieTooth disease [4]. Atypical erythrokeratoderma with deafness has also been associated with peripheral neuropathy [5]. Clinical features Differential diagnosis As an example, acroosteolysis with keratoderma (BureauBarrière syndrome) [6,7] may show diffuse keratoderma with osteolysis in the forefoot area, polyneuropathy of the lower legs and painless ulcers of the feet. The disease is nonfamilial and often subsumed under the concept of neurotrophic ulcers [8]. Given the success of of etretinate, acitretine may be the treatment of choice [1]. The lesions of reactive arthritis are compact, heaped up and resemble the heads of nails (keratoderma blenorrhagica). Extensive hyperkeratotic eczema may be difficult to distinguish on clinical and histological grounds but marked itching may indicate eczema. The even orange hyperkeratosis of pityriasis rubra pilaris is associated with an acute follicular eruption in adults and by lesions on the knees and elbows in children. Keratoderma is also reported in association with acrocyanosis and livedo reticularis [12]. In lichen planus, warty lesions may be mistaken for viral warts; lichen planus and other lichenoid eruptions such as lichen nitidus may mimic punctate keratoderma [14]. Trichophytosis, especially resulting from Trichophyton rubrum, may be unilateral and lacking inflammatory signs. The tendency of secondary syphilis lesions to involve the palms is well known, and hyperkeratotic late syphilides may be warty or focal [15]. In immunocompromised patients, viral warts may be confluent on the palms or soles. Palmoplantar hyperkeratosis with myxoedema, improving with treatment, has been reported on several occasions [16,17]. In chronic lymphoedema, the skin overlying the lymphoedematous area first becomes diffusely thickened, and then develops into a velvety papillomatous surface, which is ultimately covered by large irregular warty projections (lymphostatic verrucosis; mossy foot) [1921]. Lymphoedematous keratoderma occurs most characteristically in filariasis, but may develop in the context of chronic lymphoedema of any origin. The dermis is oedematous with dilated lymphatics, conspicuous newvessel formation, some sclerosis and a variable infiltrate of inflammatory cells. Both the hyperkeratotic component and the lymphoedema improved in three cases given etretinate 0. Carcinogens, of which the best documented example is arsenic, may produce both keratoderma and internal malignancy [28,29]. One survey showed that palmar keratoses occur four to five times more frequently in patients with cancer than in controls [30]. An increased incidence of keratoses in patients with lung or bladder cancer has been debated [3133]. Keratoses associated with cancer are histologically distinct from arsenical keratoses [34]. Keratoderma may result from tegafur, glucan, lithium and halogenated weedkillers, and dioxin figure 65. Arsenicalinduced irregular warty keratoses, or more even glassy lesions, are still occasionally seen [40]. Agents used in cancer treatment commonly cause palmoplantar erythema (the handfoot syndrome) and may cause keratoderma [4143]. Cases have since been identified in several other countries, and a familial link to the Oudtshoorn cluster is evident in most. Pathophysiology It is an autosomal dominant disorder with variable penetrance and linkage to chromosome 8p22p23 has been reported in five South African and one German kindred [3]. The genetic alteration may have originated in a French immigrant in the late 1700s. A Norwegian family with four affected members did not show linkage to chromosome 8p22p23, suggesting genetic heterogeneity [6]. A frequent precipitant is cold dry weather and, although in South Africa it is most active in winter months, it may be perennial in temperate climates. Other triggers include febrile illness, surgery, stress and menstruation, and it improves in pregnancy and with age. The father of an affected toddler was unaffected but paternal aunts and other family members had similar palmoplantar eruptions and her paternal great great grandmother originated from Oudtshoorn [7], suggestive of partial penetrance. Episodes may be preceded by itch and hyperhidrosis and associated with pustulation. Palmoplantar erythema develops, and is followed by the evolution of painless superficial opaque dry blebs, which peel or can be pulled away, leaving a red base with intact markings. A second wave may begin at the centre of a lesion, resulting in gyrate and polycyclic annular erythema, which eventually resolves. Cycles repeat every few weeks and the palms and soles appear normal between attacks. Truncal lesions were reported in one patient [2], and facial involvement in another [8]. A similar phenotype affecting the palms, more active in summertime, was reported in Porokeratoses 65. Investigations Biopsy of the advancing edge of a lesion shows hyperplasia, spongiosis and, in the upper stratum spinosum, keratinocytes with pale cytoplasm, perinuclear vacuolization and pycnotic nuclei.