Anafranil
General Information about Anafranil
In addition to its use in psychological health conditions, Anafranil can additionally be prescribed for ongoing pain administration. This could embody continual pain circumstances corresponding to fibromyalgia, neuropathic ache, and rigidity headaches. By focusing on particular neurotransmitters in the mind, Anafranil can scale back pain signals and provide relief to people affected by persistent pain.
Like any treatment, Anafranil could cause side effects such as dry mouth, drowsiness, constipation, and blurred imaginative and prescient. However, these unwanted effects are usually delicate and tend to fade with continued use. It is crucial to follow the prescribed dosage and seek the guidance of a well being care provider if any unwanted facet effects happen or worsen.
Moreover, it is crucial to notice that Anafranil is a prescription treatment and will solely be taken under the steering of a healthcare skilled. They will assess the severity of your condition and determine the appropriate dosage for you. It is crucial to observe the prescribed routine and not cease taking the medication abruptly, as it may lead to unwanted withdrawal signs.
Panic assaults, however, are characterised by sudden and intense emotions of fear, typically accompanied by bodily signs corresponding to coronary heart palpitations, shortness of breath, and dizziness. These attacks may be extraordinarily distressing and may occur unexpectedly, causing a significant influence on an individual's quality of life. Anafranil has been discovered to be beneficial in decreasing the frequency and severity of panic assaults.
OCD is a psychological disorder that causes obsessive thoughts and compulsive behaviors. Individuals with OCD could experience problem controlling their ideas and actions, resulting in significant distress and interference in their day by day lives. According to the National Institute of Mental Health, roughly 2.2 million adults within the United States have OCD. Anafranil is one of the really helpful treatments for this dysfunction and has proven to be highly efficient in managing OCD symptoms.
Depression is a temper dysfunction that impacts hundreds of thousands of people worldwide. It is characterized by persistent feelings of unhappiness, hopelessness, and lack of curiosity in actions that used to deliver pleasure. Anafranil works by balancing the levels of certain neurotransmitters in the mind, including serotonin and norepinephrine. These neurotransmitters play an important function in regulating temper, and an imbalance can lead to signs of despair. Anafranil helps to alleviate these symptoms and enhance general well-being.
Furthermore, Anafranil may interact with other drugs, together with blood thinners, antihistamines, and sure antibiotics. It is essential to inform your physician of any other medications you are taking to avoid potential drug interactions.
Anafranil, also referred to as clomipramine, is a medicine that falls underneath the class of tricyclic antidepressants (TCAs). It is primarily used to deal with psychological health issues, corresponding to obsessive compulsive disorder (OCD), panic assaults, melancholy, and ongoing pain. Anafranil works on the central nervous system, providing aid to people affected by these debilitating situations.
In conclusion, Anafranil is a widely used treatment for the treatment of OCD, panic assaults, despair, and ongoing ache. It works by concentrating on specific neurotransmitters within the mind, offering aid to people struggling with these conditions. If you or a liked one is affected by any of these issues, it is important to seek professional assist and talk about the use of Anafranil as a potential remedy option. With proper use and monitoring, this treatment can considerably enhance a person's high quality of life.
Because of the growing interest in prevention of hyperphosphatemia to improve outcome depression medication for teens buy anafranil online now, some dialyzer manufacturers have begun to optimize the phosphate clearance of their dialyzers. The main barrier to phosphate removal is the rather quick fall in serum phosphorus level that occurs early during dialysis. Because of this, only modest improvements in phosphorus removal with optimized membranes are to be expected, but the improvement is not negligible. In vitro measures of 2-microglobulin clearance are problematic and are not reported. One problem with making dialyzers very permeable in order to increase 2-microglobulin removal has been increased loss of albumin. It turns out that much of this problem is due to the nonuniformity of pore size in such membranes. New "nanotechnology" approaches to manufacturing high-flux membranes have resulted in relatively high 2-microglobulin removal rates with very acceptable (low) levels of albumin loss. The membrane surface area of most dialyzers suitable for the treatment of adult patients ranges between 0. Smaller-size dialyzers are available from many manufacturers for the use of pediatric patients. Large surface area dialyzers normally have high urea clearances, although dialyzer design and thickness of the membrane are also important properties. Historically, the surface area played a role in respect of biocompatibility, particularly with dialyzers using membranes made of unsubstituted cellulose. This aspect of dialyzer function is less important in current dialyzers that predominantly use synthetic membranes. It should be remembered that the priming volume of the blood lines is about 100150 mL. The value of the extracorporeal volume of the blood tubing sets and dialyzer is an important consideration when treating pediatric or very small adult patients. Both parameters influence flow through the fiber bundle, which, in turn, impacts on dialyzer efficiency. The four primary methods of sterilization are electron-beam, -irradiation, steam autoclaving, or ethylene oxide gas. The use of ethylene oxide has lost popularity because of (a) the rare but serious occurrence of anaphylactic reactions during dialysis in occasional patients who are allergic to ethylene oxide and (b) environmental concerns. A high blood level in the venous chamber and a wet-stored dialyzer help to reduce exposure for microemboli during hemodialysis. Theory and validation of access flow measurement by dilution technique during hemodialysis. Patients are exposed to 120-200 L of dialysis solution during each dialysis treatment. Any small molecular weight contaminants in the dialysis solution can enter the blood unimpeded and accumulate in the body in the absence of renal excretion. Therefore, the chemical and microbiologic purity of dialysis solution is important if patient injury is to be avoided. Dialysis solution is prepared from purified water (product water) and concentrates, the latter containing the electrolytes necessary to provide dialysis solution of the prescribed composition. Most concentrates are obtained from commercial sources and their purity is subject to regulatory oversight. The purity of the water used to prepare dialysis solution or to reconstitute concentrates from powder at a dialysis facility, is the responsibility of the dialysis facility. Some substances added to municipal water supplies for public health reasons pose no threat to healthy individuals at the concentrations used, but can cause injury to renal failure patients if these substances are allowed to remain in the water used for dialysis. Therefore, all municipal water supplies should be assumed to contain substances harmful to dialysis patients, and all dialysis facilities require a system for purifying municipal water before it is used to prepare dialysis solution. Please refer to Suggested Readings for a more complete discussion of these and other contaminants. This is added to water as a flocculating agent by many municipal water suppliers (aluminum sulfate is used to remove nonfilterable suspended particles). Aluminum causes bone disease, a progressive and often fatal neurologic deterioration known as the dialysis encephalopathy syndrome, and anemia. The International Organization for an exhausted deionizer and cause severe pruritus, nausea, and fatal ventricular fibrillation. The water used to prepare dialysis solution and the final dialysis solution are both susceptible to microbiologic contamination by bacteria and their endotoxins. Contamination of municipal water supplies by other microbial products, such as microcystins derived from blue-green algae, can also prove toxic to hemodialysis patients (Carmichael, 2001). Dialysis centers should be aware of the potential presence of such toxins, particularly in areas subject to seasonal algae blooms. These standards have been adopted by the Association for the Advancement of Medical Instrumentation as national standards for the United States and are also followed by regulatory organizations in many other countries. The standards set maximum levels for chemicals known to be toxic to hemodialysis patients, for chemicals known to be toxic to the general population, and for bacteria and their endotoxins. Pyrogenic reactions do not occur when levels of bacteria and endotoxins in the dialysis solution are maintained below these limits. Low levels of endotoxins and endotoxin fragments in dialysis solution, while not causing pyrogenic reactions, may contribute to a chronic inflammatory response that may be associated with long-term morbidity in dialysis patients. In observational studies, the use of so-called "ultrapure" dialysis solution, which is characterized by a bacteria level below 0. Ultrapure dialysis solution has also been associated with reduced plasma levels of 2-microglobulin and pentosidine (a surrogate marker of carbonyl stress), a slower loss of residual renal function, and lower cardiovascular morbidity (Susantitaphong, 2013).
This allows for a sudden increase in intracellular calcium mood disorder mania quality 25 mg anafranil, which causes preformed insulin to be released from intracellular secretory granules. First generation sulfonylureas (acetohexamide, chlorpropamide, tolazamide, and tolbutamide) are almost never used anymore. The second generation drugs (glipizide, glyburide, and glimepiride) are still fairly widely employed. All the second generation sulfonylureas undergo hepatic metabolism with a variable percentage of renal excretion (Spiller, 2006). The metabolite of glipizide has little or no hypoglycemic activity and a short half-life of 24 hours. Therefore, even though its renal excretion is high (80%85%), glipizide is the sulfonylurea of choice in dialysis patients. However, sulfonylureas as a class show a relatively high incidence of hypoglycemia, plus many drugs frequently used in dialysis patients can either antagonize (phenytoin, nicotinic acid, diuretics) or enhance (salicylates, warfarin, ethanol) the hypoglycemic action of sulfonylureas. In people with type 2 diabetes, endogenous insulin, assessed by C-peptide measurements, was highest in people with recently diagnosed disease and progressively decreased in people as the duration of diabetes increased. Since most people on dialysis will have had diabetes for a fairly long time, many will be producing little or no endogenous insulin and so will be unable to respond to sulfonylureas. Metformin, a member of the biguanide class, is perhaps the most widely used oral agent to treat type 2 Chapter 32 / Diabetes 565 32. Metformin use is associated with a very low incidence of hypoglycemia, weight loss instead of weight gain, and a favorable effect on serum lipids. Its mechanism of action is to acutely decrease hepatic glucose production by transiently inhibiting the respiratory enzyme chain in mitochondria. However, metformin has been associated with the rare complication of life-threatening lactic acidosis. The causation of this association is not completely clear, and acidosis is most commonly seen in patients with substantial comorbidity, but patients with markedly reduced renal function are at increased risk. Metformin is not metabolized, and 90% is excreted as the active drug by the kidneys (Spiller, 2006). Plasma metformin levels are thus substantially higher in patients with reduced creatinine clearance (Lipska, 2011). There are two -glucosidase inhibitors available in the United States: acarbose and miglitol. They work by competitively and reversibly inhibiting gut enzymes that mediate the intestinal breakdown of oligosaccharides into simple sugars, thereby limiting their absorption. Postprandial glucose surges are reduced without stimulation of endogenous insulin, and, thus, the risk of hypoglycemia is relatively low. Little acarbose is absorbed, but it is extensively metabolized in the gut, and about one-third of the metabolites, some active, are absorbed (Spiller, 2006; Reilly, 2010). In patients with reduced renal function, the plasma levels of acarbose and its metabolites can increase. Miglitol is not metabolized and is excreted unchanged in the urine (Spiller, 2006; Reilly, 2010). These drugs sensitize target tissues to insulin, increase glucose uptake in muscle and adipose tissue, and decrease hepatic glucose production. They may also have beneficial anti-inflammatory, vascular, and metabolic (hypolipidemic) effects. In the United States, it carries a warning to avoid use in patients with active bladder cancer and to consider risks versus benefits prior to initiating therapy in patients with a history of bladder cancer. One group found an increase in interdialysis weight on rosiglitazone, but this study lacked a true control group (Chiang, 2007). In 2007, a review of a variety of sources of available data linked rosiglitazone with an increased risk of myocardial infarction and cardiovascular death, and its use has been restricted in the United States (Nissen, 2007). Both pioglitazone and rosiglitazone have been associated with weight gain, edema, and congestive heart failure in nonuremic patients; the mechanism is thought to be increased renal retention of sodium and water. Acute myopathy has been reported when glitazones were given in conjunction with fibrates. Repaglinide is a member of the meglitinide family of compounds and acts as an insulin secretagogue. It binds to the sulfonylurea receptor and functions in a manner similar to the sulfonylureas, but it has an additional cell binding site and thus a different binding profile (Hatorp, 2002). Second, it is eliminated almost entirely by hepatic metabolism with biliary or fecal excretion of mainly inactive metabolites. Several studies have examined the impact of renal disease on repaglinide pharmacokinetics (Marbury, 2000; Schumacher, 2001; Hatorp, 2002). Despite these findings, there was little difference in hypoglycemia, and repaglinide is not contraindicated in people with renal disease but should be used with caution, starting at a low dose (0. In contrast to repaglinide, which has primarily fecal excretion, nateglinide, another meglitinide, is 90% excreted by the kidney, primarily as active metabolites (Spiller, 2006; Reilly, 2010). Use of nateglinide in patients on dialysis should thus be avoided or done with the greatest caution. It has multiple actions, including stimulation of endogenous insulin secretion, Chapter 32 / Diabetes 569 inhibition of endogenous glucagon secretion, delay of gastric emptying, and inhibition of appetite. The effects on insulin and glucagon are glucose-dependent, that is, they occur only in the presence of hyperglycemia.
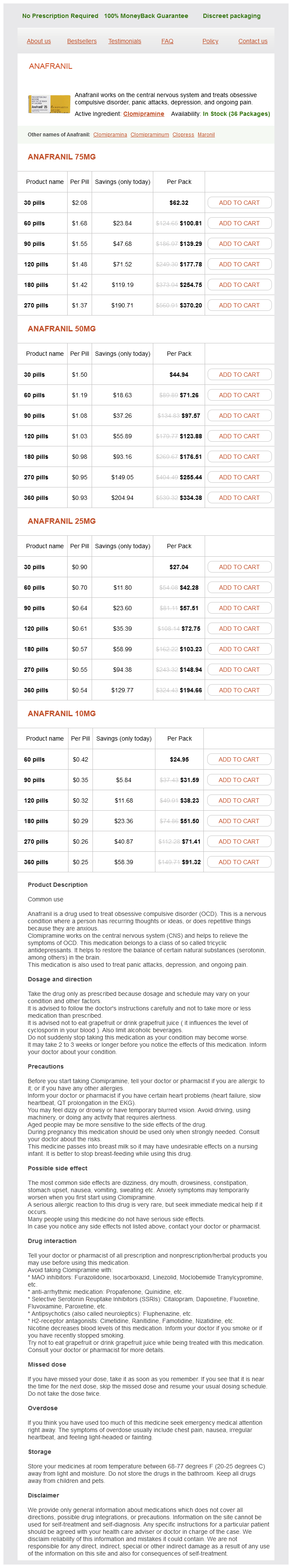
Anafranil Dosage and Price
Anafranil 75mg
- 30 pills - $62.32
- 60 pills - $100.81
- 90 pills - $139.29
- 120 pills - $177.78
- 180 pills - $254.75
- 270 pills - $370.20
Anafranil 50mg
- 30 pills - $44.94
- 60 pills - $71.26
- 90 pills - $97.57
- 120 pills - $123.88
- 180 pills - $176.51
- 270 pills - $255.44
- 360 pills - $334.38
Anafranil 25mg
- 30 pills - $27.04
- 60 pills - $42.28
- 90 pills - $57.51
- 120 pills - $72.75
- 180 pills - $103.23
- 270 pills - $148.94
- 360 pills - $194.66
Anafranil 10mg
- 60 pills - $24.95
- 90 pills - $31.59
- 120 pills - $38.23
- 180 pills - $51.50
- 270 pills - $71.41
- 360 pills - $91.32
Catheter malposition with the tip against the abdominal wall or tube restriction by attached tissues can produce both inflow and outflow pain teenage depression symptoms uk anafranil 25 mg buy low price. Slower infusion rates and incomplete drainage may diminish these symptoms; however, transluminal catheter manipulation or laparoscopic exploration should be considered for flow pain that is persistent or accompanied with hydraulic dysfunction with or without associated catheter malposition. Pain during outflow is common, especially toward the end of the drain, and is especially frequent in the early days after initiation of dialysis. As the intraperitoneal structures siphon up to the catheter tip during the drain, it causes the catheter to bump up against the exquisitely sensitive parietal peritoneum. Drain pain is more frequently a problem with automated peritoneal dialysis due to hydraulic suction on the peritoneal lining. Chapter 23 / Peritoneal Dialysis Catheters, Placement, and Care 441 Catheters implanted too low on the abdominal wall can wedge tubing into the deep pelvis, resulting in drain pain from early closure of pelvic viscera around the catheter tip. Similarly, constipation with crowding of the bowel around the catheter in the pelvis can cause or contribute to the severity of the symptoms. The drain pain sometimes resolves with time or with treatment of associated constipation. If persistent, it can be managed by avoiding complete drainage of the peritoneal effluent. In cycler patients, this can be achieved by performing some degree of tidal peritoneal dialysis. In resistant cases of drain pain, repositioning of the catheter may be attempted, but even this does not always resolve the problem. Catheter flow dysfunction is usually manifested as outflow failure; therefore, the volume of drained dialysate is substantially less than the inflow volume, and there is no evidence of pericatheter leakage. Outflow failure usually occurs soon after catheter placement, but it may also commence during or after an episode of peritonitis, or at any time during the life of the catheter. Evaluation and treatment for the common causes of flow dysfunction are as follows: a. Distended rectosigmoid colon may block the catheter side holes or displace the catheter tip into a position of poor drainage function. Extrinsic bladder compression on the catheter due to urinary retention occurs less frequently. Abdominal radiography is helpful to look for a fecal-filled colon and catheter displacement. Constipation is treated with oral administration of an emollient, such as 70% sorbitol solution, 30 mL every 2 hours until the desired effect is achieved. Polyethylene glycol solution, 2 L, ingested over a period of 46 hours is usually effective in persistent cases. Stimulant laxatives such as bisacodyl and saline enemas are reserved for refractory cases since chemical and mechanical irritation of the colonic mucosa have been associated with transmural migration of bacteria and development of peritonitis. Mechanical kinking of the catheter tubing is usually accompanied by two-way obstruction. A flatplate radiograph of the abdomen is often helpful in identifying a kink in the catheter tubing. Heparin should be added to the dialysate whenever fibrin strands or plugs are visible in the effluent. Heparin is more useful prophylactically than therapeutically, preventing the formation of fibrin clots and extension of existing clots. Once outflow obstruction has occurred, irrigation of the catheter with heparin is usually unsuccessful in recovering function. If treatment of constipation and fibrinolytic therapy are not successful in restoring drainage function, and if urinary retention and tubing kinks have been excluded, the catheter is presumed to be obstructed by omentum or other adherent intraperitoneal structures. Interventions to resolve catheter obstruction are now most commonly performed using radiologic and laparoscopic techniques. Fluoroscopic guidewire manipulation has been used to redirect displaced and obstructed catheters. Chapter 23 / Peritoneal Dialysis Catheters, Placement, and Care 443 Forceful straightening of the subcutaneous tunnel can produce tunnel track trauma and infection. Transluminal manipulation is not practical for extended catheters because of the long tubing length. A preprocedure dose of prophylactic antibiotics to provide antistaphylococcal coverage is advisable. Particular attention must be given to antiseptic preparation of the catheter tubing in addition to creating a sterile surgical field for the procedure. After catheter manipulation is performed, restoration of flow function is checked by syringe irrigation. Frequently, multiple, separate manipulation procedures are required, with long-term flow function restored in only 45%73% of cases. Failure rates for fluoroscopic manipulation as high as 90% were observed when patients had an antecedent history of abdominopelvic surgery or peritonitis, suggesting that adhesions play a major factor in technical failures. Laparoscopy has become an invaluable method of evaluating and resolving catheter flow obstruction. Because laparoscopy can reliably identify the source of flow dysfunction and provide a means for definitive treatment, it is often considered as the next step in the management sequence after other causes for obstruction have been excluded. The dialysis catheter frequently can be used to perform the initial gas insufflation of the abdomen since most catheter obstructions represent outflow problems. Alternatively, a Veress needle is used for insufflation, or the initial laparoscopic port is placed by direct cutdown on the peritoneum.