Antabuse
General Information about Antabuse
Antabuse, also known as disulfiram, is a medicine used for the treatment of alcoholism. This drug works by inflicting unpleasant results when alcohol is consumed, which acts as a deterrent for people struggling with alcohol dependancy. Antabuse does not treatment alcoholism, however it can be a useful software in the recovery course of.
In conclusion, Antabuse is an effective medication for individuals fighting alcoholism. It works by inflicting unpleasant results when alcohol is consumed, which serves as a deterrent for those in recovery. However, it is essential to keep in thoughts that this treatment is solely one part of a comprehensive treatment program for alcohol dependancy. It requires dedication and a robust dedication to sobriety for people to achieve long-term restoration. If you or someone you know is struggling with alcoholism, seek assist from a medical skilled to debate if Antabuse could additionally be a beneficial treatment possibility.
The fear of experiencing these unpleasant results can be a powerful deterrent for individuals battling alcohol addiction. Knowing that they will feel sick if they consume alcohol might help them resist the urge to drink. However, it is important to notice that Antabuse does not deal with the habit itself. It merely helps individuals stay sober by making alcohol consumption less desirable.
Antabuse is prescribed for use as part of a comprehensive treatment program for alcoholism. It is usually mixed with counseling, support teams, and other therapies to handle the underlying causes of addiction. This treatment is often used within the first few months of therapy when a person's motivation to remain sober may be at its weakest. It helps construct a foundation for sobriety and teaches individuals how to deal with their habit triggers.
Antabuse has been used as a therapy for alcoholism for the reason that Nineteen Forties. It was initially used to treat parasitic infections, but its results on alcoholism were found accidentally. Researchers noticed that patients experienced adverse reactions once they consumed alcohol while taking the medication. This led to the event of Antabuse as a therapy for alcohol habit.
If a person taking Antabuse consumes alcohol, they'll experience a range of signs that can last for a quantity of hours. These signs may be dangerous and, in some cases, life-threatening, such as heart palpitations, low blood strain, and issue respiration. Therefore, it is essential to follow the doctor's instructions and avoid any alcohol-containing products while taking Antabuse.
The way Antabuse works is by inhibiting an enzyme called aldehyde dehydrogenase, which is answerable for breaking down alcohol in the physique. As a end result, when a person takes Antabuse and consumes alcohol, their body is unable to metabolize it properly. This ends in a build-up of a poisonous substance called acetaldehyde, which causes a variety of disagreeable signs corresponding to flushing, sweating, nausea, vomiting, and headache.
Alcoholism is a severe and persistent illness that impacts tens of millions of individuals worldwide. It is characterized by a powerful longing for alcohol, an incapability to manage alcohol intake, and a bodily dependence on the substance. Alcoholism can have extreme penalties on a person's well being, relationships, and total high quality of life. Therefore, looking for therapy for alcohol dependancy is crucial for those affected.
It is crucial for sufferers to know that Antabuse isn't a magic tablet that can cure their alcohol habit. It requires a powerful dedication to sobriety and life-style adjustments to realize long-term restoration. Some individuals might experience side effects from Antabuse, similar to drowsiness, complications, or skin rash. It is essential to inform one's physician if these unwanted facet effects turn out to be bothersome or extreme.
Improving outcomes in coronary surgery: the impact of echo-directed aortic cannulation and perioperative hemodynamic management in 500 patients medications that cause weight gain buy antabuse canada. Aortic no-touch technique makes the difference in off-pump coronary artery bypass grafting. Ascending aortic atheroma assessed intraoperatively by epiaortic and transesophageal echocardiography. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Noninvasive cerebral oxygenation may predict outcome in patients undergoing aortic arch surgery. The effects of cardiopulmonary bypass on the number of cerebral microemboli and the incidence of cognitive dysfunction after coronary artery bypass graft surgery. Considerations in prevention of surgical site infections following cardiac surgery: when your patient is diabetic. Low T4 syndrome: a strong prognostic predictor of death in patients with heart disease. The low triiodothyronine syndrome: a strong predictor of low cardiac output and death in patients undergoing coronary artery bypass grafting. Gender specific practice guidelines for coronary artery bypass surgery: perioperative management. Differential effects of direct thrombin inhibitors and antithrombin-dependent anticoagulants on the dynamics of clot formation. Guide to anticoagulant therapy: Heparin: a statement for healthcare professionals from the American Heart Association. The Society of Thoracic Surgeons, the Society of Cardiovascular Anesthesiologists, and the American Society of ExtraCorporeal Technology: Clinical Practice Guidelines-Anticoagulation During Cardiopulmonary Bypass. Adequate anticoagulation during cardiopulmonary bypass determined by activated clotting time and the appearance of fibrin monomer. Evidence based coagulation monitors: heparin monitoring, thromboelastography, and platelet function. Correlations between activated clotting time values and heparin concentration measurements in young infants undergoing cardiopulmonary bypass. Anticoagulation for cardiac surgery in patients receiving preoperative heparin: use of the high-dose thrombin time. Protamine dosage based on two titrations reduces blood loss after valve replacement surgery: a prospective, double-blinded, randomized study. Heparin resistance and antithrombin: should it still be called heparin resistance Decreased concentration of antithrombin after preoperative therapeutic heparin does not cause heparin resistance during cardiopulmonary bypass. Postoperative activity, but not preoperative activity, of antithrombin is associated with major adverse cardiac events after coronary artery bypass graft surgery. Low preoperative antithrombin activity causes reduced response to heparin in adult but not in infant cardiac-surgical patients. Heparin dose response is independent of preoperative antithrombin activity in patients undergoing coronary artery bypass graft surgery using low heparin concentrations. Can extra protamine eliminate heparin rebound following cardiopulmonary bypass surgery Treatment and prevention of heparin-induced thrombocytopenia: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Prevalence of heparin/platelet factor 4 antibodies before and after cardiac surgery. Positive heparin-platelet factor 4 antibody complex and cardiac surgical outcomes. Argatroban anticoagulant therapy in patients with heparin-induced thrombocytopenia. Impact of heparin-induced thrombocytopenia on outcome in patients with ventricular assist device support: single-institution experience in 358 consecutive patients. Hemodynamic changes after protamine administration: association with mortality after coronary artery bypass surgery. Mortality and adverse events after protamine administration in patients undergoing cardiopulmonary bypass. Risk factors for clinically important adverse events after protamine administration following cardiopulmonary bypass. Effect of site of venous protamine administration, previously alleged risk factors, and preoperative use of aspirin on acute protamine-induced pulmonary vasoconstriction. The safety of aprotinin and lysine-derived antifibrinolytic drugs in cardiac surgery: a metaanalysis. The response to activated protein C after cardiopulmonary bypass: impact of factor V leiden. Factor V Leiden protects against blood loss and transfusion after cardiac surgery. Thrombosis after deep hypothermic circulatory arrest with antifibrinolytic therapy: is factor V leiden the smoking gun. Impact of clopidogrel in patients with acute coronary syndromes requiring coronary artery bypass surgery: a multicenter analysis. Does preoperative platelet function predict bleeding in patients undergoing off pump coronary artery bypass surgery Effect of clopidogrel on bleeding and transfusions after off-pump coronary artery bypass graft surgery: impact of discontinuation prior to surgery. Effect of abciximab on the outcome of emergency coronary artery bypass grafting after failed percutaneous coronary intervention.
They can decrease the pacing rate in a stepwise fashion to search for intrinsic electrical activity medicine ball purchase antabuse 500 mg with visa. If no intrinsic rate is present around 40 to 45 beats/min or the patient develops symptoms, the patient may be considered pacemaker-dependent. If the patient is deemed to be pacemaker-dependent, a secondary method for pacing the patient should be considered in the event of a pacemaker failure. Alternative methods of pacing patients intraoperatively include transesophageal pacing, transcutaneous pacing, or transvenous pacing through a pacing pulmonary artery catheter or through a temporary transvenous pacing wire. Transcutaneous pacing depends on correct pad position and high pacing outputs, which can be very uncomfortable in a nonsedated patient. Transvenous pacing and pacing pulmonary artery catheters can be time consuming, and they are not ideal choices for emergent pacing. Whatever method is chosen, it is important to have the necessary equipment and support organized and available prior to beginning the procedure. A summary of important information for the anesthesia team to identify is summarized in Table 38. Monopolar electrocautery is the most frequently used type of electrocautery because it has both cutting as well as coagulation capabilities. Monopolar electrocautery creates a current that passes from the probe to the tissue and returns through the patient to the return pad to create an electrical circuit. Bipolar electrocautery is usually not a concern25; the electrical current field is small and limited to the two poles at the end of the electrode. Unfortunately, bipolar is less frequently used compared with monopolar electrocautery and is usually reserved for neurosurgery, ophthalmology, and head and neck procedures. The vast majority of electrocautery encountered in the operating suite is monopolar due to its versatility. Such failure to initiate a paced rhythm (inhibition of the pacemaker) can compromise hemodynamics in a pacemaker-dependent patient. This assumes that the monopolar electrocautery grounding pad or return pad is also placed below the level of the umbilicus. When magnets are applied to the pacemaker, the effect on the device depends on the manufacturer, in addition to the battery life. If the Medtronic device is a single-chamber pacemaker, it will pace that single chamber asynchronously. If the Medtronic device is a dual-chamber pacemaker, it will pace both chambers asynchronously. If the Medtronic pacemaker has adequate battery life, the device will pace at 85 beats/min. However, if the battery life is at the elective replacement interval, the device will pace at 65 beats/min. The change in rate is binary, meaning that the rate goes from 85 to 65 beats/min when the battery enters its elective replacement interval. Jude pacemakers will pace asynchronously during magnet application if the magnet response is turned on. It is important to note that magnet application is programmable- that is, with some devices, magnet application will have no effect. Jude pacemaker with magnet response programmed on, magnet application will program the device to pace asynchronously at a rate of 100 beats/min if the battery life is normal or a rate of 85 beats/min if the device is at its battery elective replacement interval. Unlike Medtronic devices, the rate change from 100 to 85 beats/min is not binary; it is a gradual reduction from 100 to 85 beats/min. This is a relatively easy way to render the pacemaker asynchronous, with the added benefit of the device reverting back to its programmed settings once the magnet is removed. Importantly, the asynchronous rate provided by magnet placement may not be appropriate for the patient for a particular procedure. At times, patients require a higher heart rate in order to increase tissue oxygen delivery. To the contrary, most magnet rates are typically around 90 beats/min, which may not be appropriate for a large subset of patients-that is, those with aortic stenosis or coronary artery disease. One advantage of reprogramming are that if the patient is not in the supine position, it may be difficult to maintain the magnet in a location over the device to render it asynchronous. This can lead to significant arrhythmias caused by depolarization of the ventricle by the pacemaker during a refractory period, due to intrinsic electrical activity. The principal disadvantage of reprogramming versus magnet application is that the changes made with the programmer are not as easily reversed. It is important to understand the risks and benefits of magnet application versus reprogramming, and create a perioperative plan that suits the patient. This can trigger arrhythmias or loss of pacing capture due to increases in pacing thresholds. In the perioperative setting, this very rarely occurs when an energy surge directly contacts the pulse generator, resulting in a major hardware/software failure. The reset mode is unique to each manufacturer and serves as a safety backup in the case of catastrophic failure. Unfortunately, magnet application and device reprogramming will not prevent electrical reset. This could lead to underpacing and hemodynamic collapse in pacemakerdependent patients.
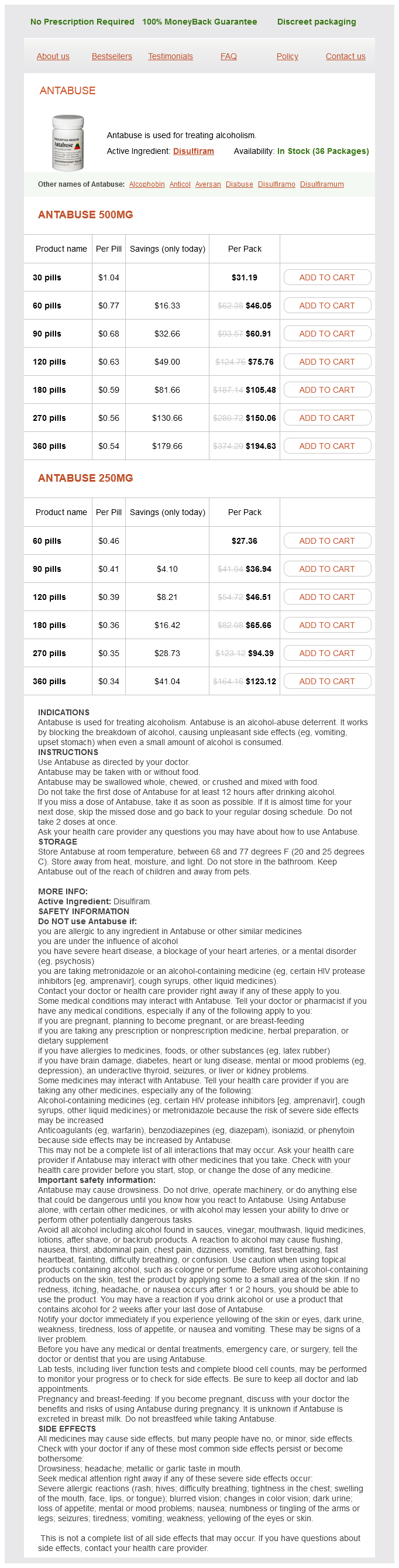
Antabuse Dosage and Price
Antabuse 500mg
- 30 pills - $31.19
- 60 pills - $46.05
- 90 pills - $60.91
- 120 pills - $75.76
- 180 pills - $105.48
- 270 pills - $150.06
- 360 pills - $194.63
Antabuse 250mg
- 60 pills - $27.36
- 90 pills - $36.94
- 120 pills - $46.51
- 180 pills - $65.66
- 270 pills - $94.39
- 360 pills - $123.12
Such transducers exhibit a high common-mode rejection ratio symptoms enlarged spleen generic 500 mg antabuse otc, defined as the tendency of the transducer to produce zero output if both of its inputs are exposed to identical pressures. In clinical settings, pressure is most commonly measured using relatively inexpensive, piezoresistive transducers. Shown are tracheal pressure and flow waveforms during controlled mechanical ventilation. Measurement of air trapping, intrinsic positive end-expiratory pressure, and dynamic hyperinflation in mechanically ventilated patients. This change in electrical resistance can be sensed with a standard Wheatstone bridge circuit, which produces an output-voltage signal appropriate for amplification and filtering. In general, piezoresistive transducers have adequate frequency responses sufficient for most respiratory applications. However, for practical reasons, most ventilators and anesthesia machines measure flow close to the machine console. This flow can be considerably different from that close to the patient because of the effects of gas compression, wall distention of the breathing circuit, and changes in gas humidity. An important clinical use of flow monitoring is the detection of nonzero end-expiratory flows. The most common method involves the measurement of a differential pressure decrease (P) across a fluid resistive element. Such a principle forms the basis for one of the oldest and most widely used flowmeters, the pneumotachograph. Although the instruments provide accurate measurement of flow, pneumotachographs are very sensitive to changes in temperature, humidity, and gas composition,268 and require frequent calibration using various electronic or software-based techniques to ensure accurate measurements. Orifice flowmeters also have the advantage of having relatively large internal diameters that limit the formation of condensation and minimize obstruction with secretions. Given that these devices can be manufactured using inexpensive plastic injection molding techniques, many orifice flowmeters are designed to be disposable, thus making their use increasingly popular for respiratory applications in clinical environments. When gas flows past the wire, the corresponding temperature drop changes the conductivity of the filament, which can be sensed with appropriate electronic circuits. Alternatively, two wires in series must be used for sensing bidirectional flow through a single conduit,274 with the flow direction determined according to which wire is cooled first. This may be accomplished by appropriately zeroing the transducer periodically, such as at the end of a breath. Although electronic or digital high-pass filters may be used to remove drifts and offsets in real-time, these tend to have long transient responses. Each of these bands produces an independent signal representative of the thoracic and abdominal cross-sectional area, and the sum of these two signals calibrated against a known gas volume yields lung volume change. These can be used to optimize lung recruitment, maintain an open lung, and limit overdistension (see the section on "Static Respiratory Mechanics"). Also, the calibration characteristics of the device are affected by changes in the pattern of breathing. A low electrical current at high frequency is applied in two chest electrodes, corresponding changes in voltage of the chest are measured, and the impedance is continuously calculated from these. The technique is implemented in several commercial systems using routine electrocardiographic leads and is also used in home monitoring of neonatal apnea. Electromyographic signal of respiratory muscles is not frequently used because of the low signal-to-noise ratio. An important drawback of techniques based on chest expansion is their inaccuracy in the presence of movement. This approach uses the Poiseuille principle (P = k × V) and differential pressure transducers to detect flow. Capnography allows for early detection of respiratory depression before O2 desaturation, particularly when supplemental O2 is administered. Respiratory rate measurements using these techniques were more accurate than those obtained with thoracic impedance tomography in extubated patients in postanesthesia care units, even with supplemental O2 at high flows. In such cases, a nasal cannula with an oral guide may improve measurement accuracy. However, pulse oximetry adds an additional level of safety combined with primary monitors of ventilation. For example, in a study using pulse oximetry and noninvasive capnography for continuous monitoring of 178 patients receiving patientcontrolled analgesia, respiratory depression measured by O2 desaturation occurred in 12% of the patients, in line Respiratory Rate Monitoring: Apnea Monitoring Apnea and bradypnea are life-threatening events frequently observed in the intraoperative and postoperative periods of anesthesia. Prematurity, morbid obesity, age, obstructive sleep apnea, and central nervous system depressant medications have been associated with risk of apnea or bradypnea. Central apnea is defined as apnea resulting from a failure of the central nervous system to drive respiration. Current monitors assess at least one of three processes occurring during breathing to detect apnea288: chest wall expansion, gas flow, and gas exchange. Changes in thoracic electrical impedance (impedance pneumography) of the chest wall. The method is based on the changes in electrical conductivity of the chest to an electrical current as air moves in and out of the lungs during breathing and blood volume changes in the same period. This is because air is a poor electrical conductor 41 · Respiratory Monitoring 1327 with previous studies. Combinations of transthoracic impedance and pulse oximetry may maximize the detection of true episodes of apnea in home monitors for neonatal apnea. The value of combining monitors of ventilation such as capnography with pulse oximetry to maximize the detection of alveolar hypoventilation has been confirmed. The most dangerous conditions occur when artifacts are detected as breathing and alarms are not activated.