Aricept
General Information about Aricept
Dementia is a debilitating condition that impacts tens of millions of people worldwide, with Alzheimer’s illness being the most typical trigger. It is a progressive brain dysfunction that leads to a decline in cognitive function, including memory, considering, and behavior. This finally impacts a person’s ability to operate independently and perform daily tasks. Fortunately, there are medicines available to help handle the symptoms of Alzheimer’s illness, considered one of which is Aricept.
The early phases of Alzheimer’s disease are sometimes characterised by memory loss, problem with language and decision-making, and adjustments in temper or habits. As the disease progresses, these symptoms worsen, making it more durable for patients to carry out even simple tasks. This is the place Aricept comes in. It can help improve cognitive perform and delay the worsening of symptoms, permitting patients to maintain their independence and quality of life for an extended interval.
While Aricept doesn't remedy Alzheimer’s illness, it can significantly improve patients’ day by day functioning and quality of life. Studies have shown that Aricept can help sufferers with Alzheimer’s illness maintain higher memory and cognition, and delay the need for long-term care. It can also assist with behavioral signs corresponding to agitation and aggression.
Like any medication, Aricept could cause unwanted effects in some individuals. Common unwanted effects include nausea, vomiting, diarrhea, lack of urge for food, and muscle cramps. These unwanted side effects are usually mild and short-term, and should improve with continued use. However, it is essential to seek the assistance of a well being care provider if these unwanted effects persist or turn out to be bothersome.
Aricept, additionally identified by its generic name donepezil, is an FDA-approved medicine used to treat dementia associated with Alzheimer’s illness. It works by growing the levels of acetylcholine, a neurotransmitter involved in reminiscence and studying, in the brain. This helps to improve communication between nerve cells and slow down the development of dementia.
Aricept is out there in each oral pill and orally disintegrating tablet type, making it easy for patients with swallowing difficulties to take. It is usually taken as quickly as a day at bedtime, however the dosage could vary depending on the individual’s situation and response to therapy. The treatment is often prescribed by a doctor and ought to be taken as directed. It is necessary not to improve or lower the dosage without consulting a healthcare skilled.
In conclusion, Aricept is a helpful medication for managing the symptoms of Alzheimer’s disease. It may help improve reminiscence, cognition, and habits, and delay the development of the disease. However, it is very important remember that Aricept only works to handle the signs and does not remedy Alzheimer’s disease. It is essential to observe your doctor’s instructions and continue with regular check-ups to observe the medication’s effectiveness and make any needed changes. For people dwelling with Alzheimer’s illness, Aricept presents hope and an opportunity to take care of a better high quality of life.
Aricept may also interact with other medicines, so it is essential to inform your physician about all the medicines, vitamins, and supplements you are taking before beginning remedy. People with certain medical circumstances, corresponding to heart illness, seizures, and asthma, must also inform their doctor earlier than taking Aricept.
The concern is that medicine mountain scout ranch buy aricept master card, given enough opportunities, the highly pathogenic H5N1 avian influenza virus will acquire the ability to spread efficiently and be sustained among humans, either by reassortment or by adaptive mutation. Other avian influenza strains have been found in human infections following close bird exposure, including H7N9 H9N2 viruses. Avian Influenza Sequence analyses of influenza A viruses isolated from many hosts in different regions of the world support the theory that all mammalian influenza viruses derive from the avian influenza reservoir. Avian influenza ranges from inapparent infections to highly lethal infections in chickens and turkeys. Influenza viruses of ducks multiply in cells lining the intestinal tract and are shed in high concentrations in fecal material into water, where they remain viable for days or weeks, especially at low temperatures. It is likely that avian influenza is a waterborne infection, moving from wild to domestic birds and pigs. It appears that the 1918 virus was not a reassortant but was derived entirely from an avian source that adapted to humans. Using reverse genetics, an infectious virus containing all the gene segments from the 1918 pandemic virus was constructed. In contrast to ordinary influenza viruses, the 1918 virus was highly pathogenic, including being able to kill mice rapidly. Preparation of Inactivated Viral Vaccines Inactivated influenza A and B virus vaccines are licensed for parenteral use in humans. Federal bodies and the World Health Organization make recommendations each year about which strains should be included in the vaccine. Selected seed strains are grown in embryonated eggs, the substrate used for vaccine production. Sometimes the natural isolates grow too poorly in eggs to permit vaccine production, in which case a reassortant virus is made in the laboratory. The reassortant virus, which carries the genes for the surface antigens of the desired vaccine with the replication genes from an egg-adapted laboratory virus, is then used for vaccine production. A cell-based vaccine using animal cell cultures became available in 2012, which overcomes some limitations of egg-based production. Virus is harvested, purified, concentrated by zonal centrifugation, and inactivated with formalin or -propiolactone. Prevention and Treatment by Drugs Amantadine hydrochloride and an analog, rimantadine, classed as adamantane drugs, are M 2 ion channel inhibitors for systemic use in the treatment and prophylaxis of influenza A. To be maximally effective, the drugs must be administered very early in the disease. Depending on the susceptibility of the predominantly circulating strains, subtyping may be useful to determine optimal therapy. Live-Virus Vaccines Prevention and Control by Vaccines Inactivated viral vaccines are the primary means of prevention of influenza in the United States. However, certain characteristics of influenza viruses make prevention and control of the disease by immunization especially difficult. Existing vaccines are continually being rendered obsolete as the viruses undergo antigenic drift and shift. Surveillance programs by government agencies and the World Health Organization constantly monitor subtypes of influenza circulating around the world to promptly detect the appearance and spread of new strains. A major advance would be the ability to design a vaccine that stimulates production of a broadly neutralizing antibody response effective against many influenza subtypes. Although protection can reach from 70% to 100% in healthy adults, frequency of protection is lower (3060%) among the elderly and among young children. Inactivated viral vaccines usually do not generate good local IgA or cell-mediated immune responses. The immune response is influenced by whether the person is "primed" by having had prior antigenic experience with an influenza A virus of the same subtype. A live-virus vaccine must be attenuated so as not to induce the disease it is designed to prevent. In view of the constantly changing face of influenza viruses in nature and the extensive laboratory efforts required to attenuate a virulent virus, the only feasible strategy is to devise a way to transfer defined attenuating genes from an attenuated master donor virus to each new epidemic or pandemic isolate. A cold-adapted donor virus, able to grow at 25°C but not at 37°C-the temperature of the lower respiratory tract-should replicate in the nasopharynx, which has a cooler temperature (33°C). A live attenuated, cold-adapted, temperature-sensitive, trivalent influenza virus vaccine administered by nasal spray was licensed in the United States in 2003. It was the first livevirus influenza vaccine approved in the United States, as well as the first nasally administered vaccine in the United States. Use of Influenza Vaccines the only contraindication to vaccination is a history of allergy to egg protein, although the cell-based vaccine overcomes this limitation. When the vaccine strains are grown in eggs, some egg protein antigens are present in the vaccine. Annual influenza vaccination is recommended for all children ages 6 months to 18 years and for high-risk groups. The live-virus intranasal vaccine is not currently recommended for individuals in the high-risk groups. Which of the following statements regarding the prevention and treatment of influenza is correct Which of the following statements about the neuraminidase of influenza virus is not correct The type-specific antigen (A, B, or C) of influenza viruses is found on which viral constituent A 70-year-old nursing home patient refused the influenza vaccine and subsequently developed influenza.
Detection methods available include neutralization symptoms joint pain generic aricept 10 mg on line, immunofluorescence, and enzyme-linked immunosorbent assay. Antibodies develop, but the virus is not eliminated from the body; a carrier state is established that lasts throughout life and is punctuated by transient recurrent attacks of herpes. Middle-class individuals in developed countries acquire antibodies later in life than those in lower socioeconomic populations. Presumably, this reflects more crowded living conditions and poorer hygiene among the latter. The virus is spread by direct contact with infected saliva or through utensils contaminated with the saliva of a virus shedder. The source of infection for children is usually an adult with a symptomatic herpetic lesion or with asymptomatic viral shedding in saliva. At any given time, 15% of normal adults are excreting virus, often in the absence of clinical symptoms. It is estimated that there are about 4060 million infected individuals in the United States. Both symptomatic and asymptomatic infections provide a reservoir of virus for transmission to susceptible persons. Studies have estimated that transmission of genital herpes in more than 50% of cases resulted from sexual contact in the absence of lesions or symptoms. Rarely, pregnant women may develop disseminated disease after primary infection, with a high mortality rate. Primary infection before 20 weeks of gestation has been associated with spontaneous abortion. Estimates of the frequency of cervical shedding of virus among pregnant women vary widely. Viral isolates from the vesicles of chickenpox or zoster patients exhibit no significant genetic variation. The drugs may suppress clinical manifestations, shorten time to healing, and reduce recurrences of genital herpes. Newborns and persons with eczema should be protected from exposure to persons with active herpetic lesions. Patients with genital herpes should be counseled that asymptomatic shedding is frequent and that the risk of transmission can be reduced by antiviral therapy and condom usage. One approach is to use purified glycoprotein antigens found in the viral envelope, expressed in a recombinant system. After initial replication in regional lymph nodes, primary viremia spreads virus and leads to replication in the liver and spleen. Secondary viremia involving infected mononuclear cells transports virus to the skin, where the typical rash develops. Varicella-zoster virus replication and spread are limited by host humoral and cellular immune responses. Herpes Zoster the skin lesions of herpes zoster are histopathologically identical to those of varicella. As a rule, the distribution of lesions in the skin corresponds closely to the areas of innervation from an individual dorsal root ganglion. It is believed that waning immunity allows viral replication to occur in a ganglion, causing intense inflammation and pain. Herpes zoster (shingles) is a sporadic, incapacitating disease of elderly or immunocompromised individuals that is characterized by pain and vesicular rash limited in distribution to the skin innervated by a single sensory ganglion. Whereas varicella is the acute disease that follows primary contact with the virus, zoster is the response of the partially immune host to reactivation of varicella virus present in latent form in neurons in sensory ganglia. Malaise and fever are the earliest symptoms, soon followed by the rash, first on the trunk and then on the face, the limbs, and the buccal and pharyngeal mucosa in the mouth. The rash lasts about 5 days, and most children develop several hundred skin lesions. Infectious virus remains strongly cell associated, and serial propagation is more easily accomplished by passage of infected cells than of tissue culture fluids. Immune system eliminates the infection except for some virions that establish latent infections inside nerve cells. If immunity wanes with age or other reason, the virus persisting in the nerve ganglia can infect the skin, causing herpes zoster. Secondary viremia results in the transport of virus to skin and respiratory mucosal sites, where replication in epidermal cells causes the characteristic rash (chickenpox). Varicella-zoster virus-specific immunity is required to terminate viral replication. The virus gains access to cells of the trigeminal and dorsal root ganglia during primary infection and establishes latency. Punch biopsies of varicella-zoster virus vesicles were fixed and stained with hematoxylin and eosin. A: Early infection showing "balloon degeneration" of cells with basophilic nuclei and marginated chromatin (reduced from 480×). B: Later infection showing eosinophilic intranuclear inclusions surrounded by wide clear zones (reduced from 480×). C: Multinucleated giant cell in the roof of a varicella vesicle (reduced from 480×). D: Low-power view of an early vesicle showing separation of the epidermis (acantholysis), dermal edema, and mononuclear cell infiltration (reduced from 40×). Herpes Zoster Herpes zoster usually occurs in persons immunocompromised as a result of disease, therapy, or aging, but it occasionally develops in healthy young adults. It usually starts with severe pain in the area of skin or mucosa supplied by one or more groups of sensory nerves and ganglia and is often unilateral. Within a few days after onset, a crop of vesicles appears over the skin supplied by the affected nerves.
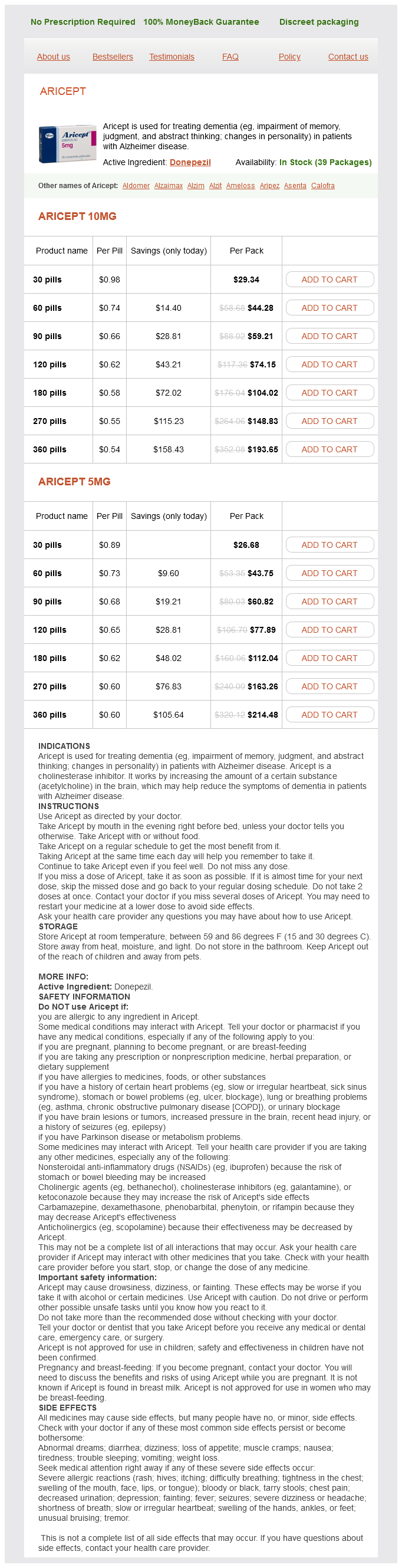
Aricept Dosage and Price
Aricept 10mg
- 30 pills - $29.34
- 60 pills - $44.28
- 90 pills - $59.21
- 120 pills - $74.15
- 180 pills - $104.02
- 270 pills - $148.83
- 360 pills - $193.65
Aricept 5mg
- 30 pills - $26.68
- 60 pills - $43.75
- 90 pills - $60.82
- 120 pills - $77.89
- 180 pills - $112.04
- 270 pills - $163.26
- 360 pills - $214.48
IgG antibodies to penicillin are common and are not associated with allergic reactions other than rare cases of hemolytic anemia symptoms for hiv aricept 5 mg buy cheap. A history of a penicillin reaction in the past is not reliable, but the drug must be administered with caution to such persons, or a substitute drug should be chosen. Allergic reactions may occur as typical anaphylactic shock; typical serum sickness type reactions (urticaria, joint swelling, angioneurotic edema, pruritus, respiratory embarrassment within 712 days of penicillin dosage); and a variety of skin rashes, fever, nephritis, eosinophilia, vasculitis, and so on. The incidence of hypersensitivity to penicillin is negligible in children but may be 15% among adults in the United States. Clinical Uses Penicillins are the most widely used antibiotics, particularly in the following areas. Penicillin G is the drug of choice in most infections caused by streptococci, susceptible pneumococci, meningococci, spirochetes, clostridia, aerobic gram-positive rods, nonpenicillinase-producing staphylococci, and actinomycetes. Penicillin G is inhibitory for enterococci (E faecalis), but for bactericidal effects (eg, in enterococcal endocarditis), an aminoglycoside must be added. Penicillin G in ordinary doses is excreted into the urine in sufficiently high concentrations to inhibit some gram-negative organisms unless they produce a large amount of -lactamases. Benzathine penicillin G is a salt of very low solubility given intramuscularly for low but prolonged drug levels. In patients with renal failure, smaller doses may produce encephalopathy, delirium, and seizures. Carbenicillin too frequently decreases normal platelet aggregation, which can lead to clinically significant bleeding. Natural cephalosporins have low antibacterial activity, but the attachment of various R side groups has resulted in the proliferation of an enormous array of drugs with varying pharmacologic properties and antimicrobial spectra and activity. Certain second- and third-generation cephalosporins can induce special -lactamases in gram-negative bacteria. In general, however, cephalosporins tend to be resistant to the -lactamases produced by staphylococci and common gram-negative bacteria that hydrolyze and inactivate many penicillins. For ease of reference, cephalosporins have been arranged into major groups, or "generations," discussed in the paragraphs that follow (Table 28-4). These are cephamycins and they have enhanced anaerobe activity but otherwise are similar in spectrum to the second-generation cephalosporins. Cephalexin, cefadroxil, and cephradine (no longer available in the United States) are absorbed from the gut to a variable extent and can be used to treat uncomplicated urinary tract infections and streptococcal pharyngitis. The following structures can each be substituted at R1 and R2 to produce the named derivatives. Cefditoren is an oral third-generation cephalosporin with excellent activity against many gram-positive and gram-negative species. This agent has bactericidal activity and stability against many -lactamase enzymes. Cefditoren is the most potent orally administered cephalosporin against S pneumoniae. It is indicated for the treatment of acute bacterial skin and skin structure infections as well as community-acquired pneumonia. Because of the growing numbers of -lactamases, some cephalosporins are being combined with -lactamase inhibitors. The most promising ones to date include ceftazidime and ceftaroline combined with avibactam, a novel -lactamase inhibitor. Cefazolin is a choice for surgical prophylaxis because it gives the highest (90120 g/mL) levels with every 8-hour dosing. Cephalothin, cephapirin, and cephradine (these agents are no longer available in the United States) in the same dose give lower levels. Second-Generation Cephalosporins the second-generation cephalosporins are a heterogeneous group. All are active against organisms covered by first-generation drugs but have extended coverage against gram-negative rods, including Klebsiella and Proteus but not P aeruginosa. Some (not all) oral second-generation cephalosporins can be used to treat sinusitis and otitis media caused by H influenzae, including -lactamaseproducing strains. Cefoxitin and cefotetan used in mixed anaerobic infections, including peritonitis and pelvic inflammatory disease. However, resistance to these agents among the B fragilis group has increased substantially. Third-Generation Cephalosporins the third-generation cephalosporins have decreased activity against gram-positive cocci except for S pneumoniae; enterococci are intrinsically resistant to cephalosporins and often produce superinfections during their use. Most third-generation cephalosporins are active against methicillin susceptible staphylococci, but ceftazidime is only weakly active. A major advantage of third-generation drugs is their enhanced activity against gram-negative rods. When second-generation drugs tend to fail against P aeruginosa, ceftazidime or cefoperazone may succeed. Thus, third-generation drugs are very useful in the management of hospital-acquired gram-negative bacteremia. Ceftazidime may also be lifesaving in severe melioidosis (Burkholderia pseudomallei infection). Cefotaxime, ceftriaxone, or ceftizoxime given intravenously may be used for management of gram-negative bacterial sepsis and meningitis. Adverse Effects of Cephalosporins the cephalosporins are sensitizing and can elicit a variety of hypersensitivity reactions, including anaphylaxis, fever, skin rashes, nephritis, granulocytopenia, and hemolytic anemia.