Atacand
General Information about Atacand
One important point to note is that there are not any instructions on critical or strengthened hypotension (extremely low blood pressure) after taking the first dose of Atacand or experiencing a withdrawal impact after stopping remedy. This highlights the protection and tolerability of the treatment, as it doesn't cause drastic modifications in blood strain that might lead to severe unwanted facet effects.
In conclusion, Atacand is an effective and well-tolerated medicine for the management of arterial hypertension. With its dose-dependent lengthy lowering of arterial stress and lack of reflex improve in coronary heart rate, it supplies a protected and tailor-made strategy to managing high blood pressure. As at all times, it's important to consult along with your physician before beginning any new medication and to comply with their directions for optimum outcomes.
However, as with any treatment, there could also be some potential side effects of Atacand. These can include dizziness, headache, fatigue, and a rise in potassium ranges within the blood. It is necessary to comply with your physician's directions and often monitor your blood stress and potassium ranges whereas taking Atacand.
The anti-hypertensive action of Atacand is achieved by way of the decrease in peripheral resistance within the body. Peripheral resistance refers back to the resistance that blood encounters because it flows by way of the body's blood vessels. By reducing this resistance, Atacand makes it simpler for blood to move, leading to a decrease in blood strain. This is different from different anti-hypertensive drugs, which may also lower blood pressure but can do so by growing heart fee, doubtlessly causing undesirable unwanted aspect effects similar to palpitations.
One important benefit of Atacand is that there is no reflex enhance in coronary heart price. This signifies that, in distinction to other drugs, Atacand does not cause the center to beat faster in response to a lower in blood pressure. This is useful for individuals with pre-existing coronary heart situations, as a rise in coronary heart price because of medicine can put extra pressure on the guts.
One of the principle benefits of Atacand is its dose-dependent lengthy reducing of arterial strain. This signifies that the treatment can be tailor-made to an individual's particular wants, with the dosage being adjusted to achieve the desired results. This is important in managing hypertension, as different individuals might require totally different doses to successfully management their blood stress.
Atacand is a drugs used to deal with arterial hypertension, also called hypertension. It is a kind of medicine called an angiotensin receptor blocker (ARB) that works by stress-free blood vessels, making it easier for blood to move via and thus lowering blood strain.
Such classification has major prognostic implications and influences important therapeutic decisions antiviral nhs generic 16 mg atacand, including the use of tyrosine kinase inhibitors. The survival of patients with the latter disorder is much shorter than that of patients with the former condition. Survival is also influenced by whether appropriate treatment is instituted during the erythrocytotic phase of the illness. Patients who have uncontrolled erythrocytosis are at an extremely high risk for the development of thromboses. The median survival time from the onset of symptoms has been reported in a study that is over four decades old to be as short as 1. Unfortunately, current therapies are not effective for this latter purpose, and controlling blood counts may have less of an effect than anticipated. No particular platelet or leukocyte count could be shown to be protective against thrombosis. At present, the therapeutic goals are to reduce the risk of thrombosis by normalizing the hematocrit levels to 45% (some experts advocate reducing the hematocrit to 42% in females) based on a randomized prospective study that demonstrated a decreased risk of cardiovascular morbidity and mortality with a goal hematocrit of less than 45% compared to 4550%. Whether therapy should be directed at normalization of platelets remains uncertain at present and should not be pursued unless within the context of a clinical trial. Extreme thrombocytosis (>1 × 109/L), if associated with spontaneous hemorrhage, is an indication for normalization of platelet numbers. A series of studies, although completed more than 30 years ago, by the Polycythemia Vera Study Group answered several very important questions regarding the efficacy and associated complications of particular therapeutic modalities. These investigations have aided in the identification of optimal therapy for individual patients, which must be selected on the basis of age and comorbid disease status to minimize treatment-related complications. Long-term survival was inferior for patients treated with chlorambucil compared with those treated with Hypertension, hypercholesterolemia, diabetes, and smoking (see text). Extreme thrombocytosis (platelet count >1500 × 109 L-1) is a risk factor for bleeding. An increasing leukocyte count has been identified as a novel risk factor for thrombosis, but confirmation is required. Median survival was 23 years in the absence of advanced age and leukocytosis, and 9 years with the presence of both of these risk factors. Patients with two or more of these risk factors had a 10-year relative survival of 26%, as opposed to patients with zero or one risk factors, who had a 10-year survival of 84% and 59%, respectively. The choice of therapeutic agents used to treat the erythrocytotic phase of disease clearly influences patient outcomes. This will avoid inappropriate exposure of patients with nonmalignant disorders to the adverse effects of myelosuppresive agents. Elderly patients with compromised cardiovascular or pulmonary systems should be more carefully phlebotomized (twice a week), or smaller volumes of blood should be removed. Selective serotonin uptake inhibitors (paroxetine 20 mg/day or fluoxetine 10 mg/day) or phototherapy can also be of use. Dramatic relief, however, can be achieved in almost all cases with the institution of ruxolitinib. Due to cost, ruxolitinib therapy should be reserved for individuals with pruritis not relieved by less costly strategies. Elective surgery or dental procedures should be delayed until hematocrit levels have been normalized for more than 2 months. If emergency surgery is contemplated, phlebotomy and cytapheresis should be pursued. During pregnancy, therapy is frequently not necessary; if it is, phlebotomy plus low-dose aspirin should be exclusively used. An early finding was the appearance during the first 5 years of a significant excess of deaths from acute leukemia in the chlorambucil arm, which reached 17% after 15 years of followup. As a result, the chlorambucil arm was discontinued, and patients were assigned randomly to one of the other two arms. Even though no statistical difference in overall survival between 32P and phlebotomy alone was apparent through the first 10 years, the morbidity and mortality associated with each type of therapy were attributable to distinctly different causes. Thrombosis as a cause of death was much more frequent in the phlebotomy-only group during the first 57 years of follow-up. Analyses of factors associated with thrombosis revealed that the performance of phlebotomy, the rate of phlebotomy, advancing age, and history of previous thrombosis were statistically significant factors predictive of this outcome. The need for more than four therapeutic phlebotomies a year in the phlebotomyalone arm was associated with an increased thrombotic risk. This led to the belief that frequent phlebotomy requirements were detrimental and necessitated cytoreductive therapy. Iron deficiency is a consequence of repeated therapeutic phlebotomy; but in fact, it should be viewed as a therapeutic goal to further limit erythropoiesis. Although iron deficiency can be associated with a number of clinical signs and symptoms, including glossitis, dysphagia, cheilosis, koilonychia, fatigue, global weakness, cognitive deficits, neuromuscular disturbances, and pica syndrome, these rarely prompt treatment discontinuation. In contrast, the use of 32P led to a lower rate of thrombosis during the first 5 years, but the incidences of leukemias, lymphomas, and nonhematologic malignancies increased during the next 5 years to nearly 10%. After a 15-year period of observation, the incidences of leukemia and lymphoma in the chlorambucil group had risen to 17%. A statistically significant increase in skin and gastrointestinal cancers occurred in the 32P- and chlorambucil-treated cohorts compared with the group treated with phlebotomy alone (see box on Algorithm for Management of Patients With Polycythemia Vera). Based on these studies, therapy with chlorambucil and 32P are no longer recommended.
Novel agents such as ibrutinib medicament antiviral zona atacand 16 mg buy fast delivery, idelasilib, lenalidomide, and bortezomib have shown promising results; their integration in upfront therapies has a potential to further improve outcomes with initial therapy. Although endoscopies of upper and lower gastrointestinal tracts are frequently positive, such evaluation may not change management. Other salvage therapy includes bortezomib, bendamustine, lenalidomide, or temsirolimus frequently combined with rituximab. Caballero D, Campo E, Lopez-Guillermo A, et al: Clinical practice guidelines for diagnosis, treatment, and follow-up of patients with mantle cell lymphoma. Jares P, Colomer D, Campo E: Genetic and molecular pathogenesis of mantle cell lymphoma: perspectives for new targeted therapeutics. Visco C, Finotto S, Zambello R, et al: Combination of rituximab, bendamustine, and cytarabine for patients with mantle-cell non-Hodgkin lymphoma ineligible for intensive regimens or autologous transplantation. Dreger P, Rieger M, Seyfarth B, et al: Rituximab-augmented myeloablation for first-line autologous stem cell transplantation for mantle cell lymphoma: effects on molecular response and clinical outcome. Lamm W, Kaufmann H, Raderer M, et al: Bortezomib combined with rituximab and dexamethasone is an active regimen for patients with relapsed and chemotherapy-refractory mantle cell lymphoma. Wang M, Fayad L, Wagner-Bartak N, et al: Lenalidomide in combination with rituximab for patients with relapsed or refractory mantle-cell lymphoma: a phase 1/2 clinical trial. Zaja F, De Luca S, Vitolo U, et al: Salvage treatment with lenalidomide and dexamethasone in relapsed/refractory mantle cell lymphoma: clinical results and effects on microenvironment and neo-angiogenic biomarkers. Martin P, Chadburn A, Christos P, et al: Outcome of deferred initial therapy in mantle-cell lymphoma. Robak T, Huang H, Jin J, et al: Bortezomib-based therapy for newly diagnosed mantle-cell lymphoma. Although they share many clinical and biologic features, the approach to their management is different; therefore, an accurate histologic diagnosis is of utmost importance. Therefore, it is imperative to promptly evaluate patients with these diseases and expeditiously institute appropriate therapy. Patients may have constitutional manifestations from the production of inflammatory molecules and a variety of other cytokines and chemokines produced by the lymphoma cells or host tissues. Such manifestations include weight loss, malaise, fevers, night sweats, and loss of appetite. Of these, unexplained weight loss of more than 10% of body weight and temperature higher than 38°C as well as drenching night sweats are referred to as "B" symptoms. Recent progress using techniques such as molecular profiling and other high-resolution genetic technologies are further advancing this taxonomy. Although this differentiation may not affect treatment choice initially, it will affect prognosis and natural history, and therefore needs to be recognized at diagnosis. It is important to determine if there is a history of potential causative factors such as prior malignancy, chemotherapy or radiation treatment, or autoimmune or immunodeficiency diseases. Aggressive lymphoma should be diagnosed by an experienced hematopathologist familiar with the nuances and pitfalls of lymphoma diagnosis. Patients with a history of hepatitis B infection should either receive antiviral prophylaxis or have the hepatitis B viral load monitored very closely (ideally on each cycle) with a low threshold to commence antiviral medications. The use of other imaging modalities depends on the clinical presentation and sites of disease. The latter should be included due to the importance of identifying patients with active hepatitis and a history of hepatitis B because they will likely require treatment with antivirals, monitoring, or both (see box on Hepatitis B Prophylaxis and Therapy During Lymphoma Treatment). We administer intrathecal prophylaxis to all patients who fulfill either of the following criteria: 1. We commence prophylaxis on cycle 3 day 1 and administer it on days 1 and 5 of cycles 3 through 6. All cases are subclassified to indicate the absence (A) or presence (B) of the systemic symptoms of significant fever (>38. In routine clinical practice, it has not been feasible to perform gene expression profiling and immunohistochemistry algorithms to predict cell of origin have been used up until now. While these have been somewhat helpful, they have demonstrated varying degrees of concordance with microarray results, limiting their usefulness. For early stage disease, whether or not radiation treatment adds benefit to chemotherapy has been controversial. However, longer patient follow-up showed a convergence of the overall survival curves because of late systemic relapses in the combined modality arm, thus reopening the debate on radiation. After consolidation radiotherapy, however, only 19% of patients had a positive gallium scan, and 80% were event-free at 39 months of median follow-up. If at this time, the result becomes negative, patients go into routine follow-up, and if it remains abnormal, we perform a biopsy and administer radiation if the biopsy confirms residual disease. Radiotherapy has been a mainstay of treatment because it is effective and sidestepped the limitations of chemotherapy, but responses are usually short lived, and virtually all patients relapse. Unfortunately, such combined modality treatment is associated with severe long-term neurotoxicity and recently, a high incidence of late relapses has been identified for this disease entity. For this reason, there has been much interest in developing regimens that obviate or defer the need for radiation until relapse. There are three recognized clinical variants, and they vary in whom they affect and how they present, and they also have morphologic and biologic differences. Although older studies demonstrated that surgical resection of abdominal disease improved outcome, indicating the importance of tumor volume, more effective and risk-adapted treatments have made surgical resection unnecessary except for specific complications such as obstruction, perforation, fistula, or bleeding.
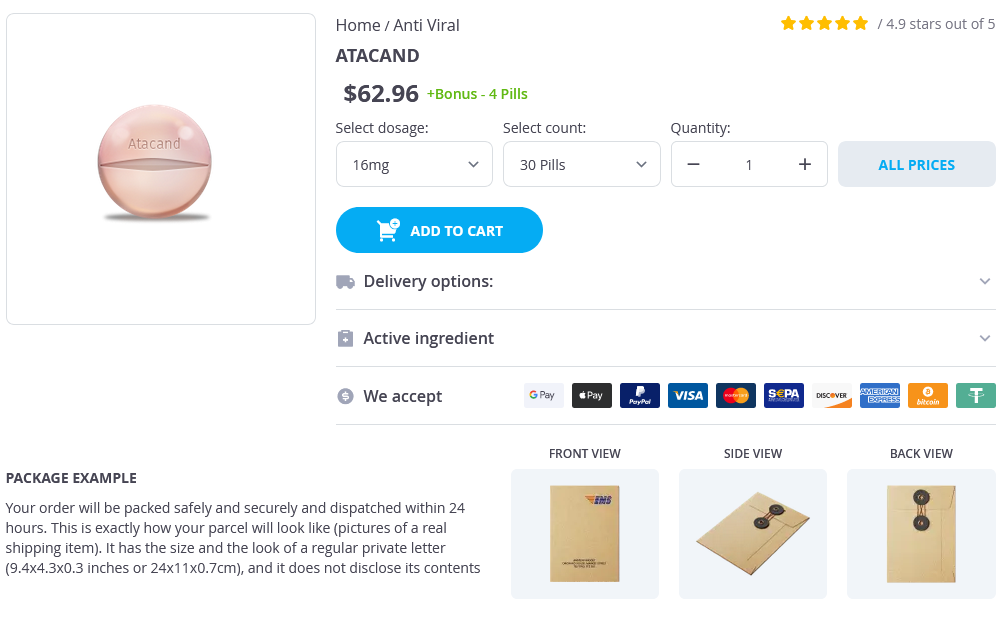
Atacand Dosage and Price
Atacand 16mg
- 30 pills - $69.95
- 60 pills - $134.35
- 90 pills - $178.55
Atacand 8mg
- 30 pills - $75.95
- 60 pills - $97.65
- 90 pills - $132.45
Atacand 4mg
- 30 pills - $50.99
- 60 pills - $81.99
- 90 pills - $96.99
Within a few months after presentation aloe vera anti viral properties cheap 16mg atacand with mastercard, it will become apparent that the lesions seen initially are limited to the skeleton or were the "heralding lesion(s)" of diffuse systemic involvement. When cutaneous involvement is the only obvious presenting sign, several months may be required to determine the ultimate extent of disease. All patients should be evaluated with a complete blood count, chemistries including liver function tests, coagulation workup, and urine osmolality. Chronically draining ears from temporal bone involvement is often diagnosed as chronic otitis media. Liver and spleen involvement must be distinguished from leukemia and storage diseases. In general, the only patient population with significant mortality rates are those with visceral, or so-called "risk organ", involvement. Of the approximately 79% of patients who responded to initial therapy, 94% were alive at 5 years, but only 11% of the nonresponders survived. These important data suggest that alternative therapies should be tested early during the course of therapy for patients with poor early responses. Skin involvement frequently mimics seborrheic dermatitis, albeit with a severe or refractory course. In patients with potentially morbid or life-threatening disease at presentation or in those who develop morbid or lifethreatening disease during the course of treatment, alternative and sometimes more aggressive treatment should be implemented. For the majority of patients with localized or limited systemic disease, the goal of therapy should be minimizing loss of function and preventing cosmetic deformity. Seborrhea-like dermatitis of the scalp may improve with use of a selenium- or phenol-based shampoo. Topical steroids can be effective, but prolonged exposure or use on the face should be avoided. In patients with particularly refractory and extensive skin involvement, psoralen ultraviolet A can be effective. Surgery and Radiotherapy Patients with disease involving a single bone can usually be managed with local therapy. This most often involves surgical curettage for patients whose lesions are in easily accessible, noncritical locations. Complete "cancer operation" resections are not considered necessary and should be avoided to reduce cosmetic and orthopedic deformities, as well as loss of function. Because of concerns about the development of secondary malignancies, systemic therapy is usually favored over radiation. However, local radiotherapy is indicated under certain circumstances; for example, when patients are at risk for visual or hearing loss, skeletal deformity, spinal cord injury, or severe pain when systemic therapy is not rapidly effective. Alternative treatment has not been standardized for patients with recurrent or refractory disease. In addition, the combination of 2-CdA and high-dose cytarabine has been used in refractory, high-risk patients. Finally, a recent report, by Simko et al has demonstrated that upfront use of cytarabine monotherapy is associated with excellent response rates, and may avoid the toxicities of prednisone/vinblastine-based regimens. Patients with neurodegenerative syndrome may have ataxia, dysarthria, dysmetria, and learning and behavior difficulties. A retrospective analysis by Willis et al of 71 patients from a single institution followed for a median of 8. Thus judicious use of radiotherapy, avoidance of potentially carcinogenic chemotherapeutic agents, and good supportive care are recommended. The only successful treatment of sclerosing cholangitis has been liver transplantation. No effective treatment is available, and progression to cor pulmonale and respiratory failure may occur. A reasonable therapeutic approach to systemic therapy is to observe patients with limited, single-system disease who respond to local. If persistent symptomatic lesions or evidence of progressive disease is seen, systemic treatment should be pursued. Patients with disease that is localized to skin, bone, and lymph nodes (defined as "nonrisk" organs) generally have a good prognosis and may require only minimal treatment. Extensive refractory skin disease may warrant systemic therapy with low-dose oral methotrexate, vinblastineprednisone, or low-dose cytarabine, or with topical therapy such as nitrogen mustard. Multisystem disease or multifocal bony disease usually warrants treatment with systemic chemotherapy. Trials are ongoing for the assessment of B-Raf and Mek inhibitors in pediatric solid malignancies. Future clinical trials for such targeted therapies will likely focus on patients with therapy-resistant risk organ involvement because these children have the least satisfactory outcomes. These red-yellowish, benignappearing lesions are sometimes mistaken for molluscum. Lesions may vary significantly in size and number but are often several millimeters to 1 cm in size and solitary. Of note, residual pigmented areas may persist indefinitely even after lesions have regressed. In patients who do not respond to initial treatment with vinblastine and steroids, use of other agents, such as methotrexate, steroids, and 2-CdA, has led to responses, according to anecdotal reports. It usually presents with xanthoma-like skin nodules and bilateral lower limb bone pain. They may also have periorbital involvement with exophthalmos and impingement on the optic nerves. However, a recent report of excellent response to a B-Raf inhibitor may change this standard of care.