Augmentin
General Information about Augmentin
Otitis media is a kind of ear an infection that impacts the middle ear, and it may possibly occur in both children and adults. This type of an infection is often attributable to micro organism, and Augmentin is often the first line of treatment. It works by focusing on the micro organism and stopping its progress, thus enhancing symptoms such as ear pain, fever, and issue listening to.
One of the explanation why Augmentin is such a preferred selection for treating these bacterial infections is its broad spectrum of exercise. This means that it can effectively kill a extensive range of micro organism, making it a reliable therapy possibility for a big selection of infections. The mixture of amoxicillin and clavulanate can be effective at stopping the event of antibiotic resistance, which is a major concern within the medical group.
In conclusion, Augmentin is an efficient antibiotic option for treating bacterial infections of the lower respiratory tract, otitis media, sinusitis, pores and skin infections, and urinary tract infections. It has a broad spectrum of exercise and is often prescribed due to its effectiveness and low danger of creating resistance. As with any medicine, you will want to use Augmentin as directed and full the total course of treatment to ensure a profitable recovery.
Sinusitis is an infection of the sinuses, which are hollow cavities in the cranium that help to filter and humidify air. When these become infected, they can trigger symptoms similar to congestion, facial pain, and headaches. Augmentin is efficient at treating sinusitis because it could attain the infected sinus tissue and eliminate the bacteria inflicting the infection.
Augmentin is a robust antibiotic treatment that is used to treat a variety of bacterial infections. It is a mix of two elements, amoxicillin and clavulanate, which work together to effectively kill bacteria. This medication is often used to treat infections within the decrease respiratory tract, otitis media, sinusitis, pores and skin infections, and urinary tract infections.
Urinary tract infections (UTIs) are one of the widespread bacterial infections, affecting each men and women. They may be attributable to bacteria getting into the urinary tract through the urethra, and can outcome in signs corresponding to ache, burning during urination, and frequent urges to urinate. Augmentin is often prescribed to deal with UTIs because it can attain the bacteria within the urinary tract and kill them, leading to symptom aid.
The decrease respiratory tract consists of the lungs and airways, and bacterial infections on this area can cause a broad range of signs corresponding to cough, chest pain, and problem breathing. Augmentin is usually prescribed for these sort of infections as a end result of it's effective against the commonest micro organism that cause them. By killing the bacteria, Augmentin helps to alleviate signs and speed up recovery.
Skin infections could be caused by a variety of bacteria, including staph and strep. These infections can range from mild to severe, and will require antibiotic therapy to totally clear. Augmentin is commonly prescribed for skin infections as a end result of it's efficient at killing a variety of micro organism and stopping them from spreading.
Augmentin is on the market in each tablet and liquid form, making it easily accessible and convenient to take. However, it is very important note that this medicine should only be taken as directed by a healthcare skilled. It can be essential to finish the complete course of therapy, even if signs enhance, to guarantee that the infection is absolutely eradicated.
Expression of cytokeratin 20 in developing rat liver and in experimental models of ductular and oval cell proliferation virus 7 band buy generic augmentin from india. A classification of ductal plate malformations based on distinct pathogenic mechanisms of biliary dysmorphogenesis. Nomenclature of the finer branches of the biliary tree: canals, ductules, and ductular reactions in human livers. Anatomy of the biliary ducts within the human liver: analysis of the prevailing pattern of branchings and the major variations of the biliary ducts. Embryology, anatomy, and surgical applications of the extrahepatic biliary system. Surgical anatomy of hepatic hilum with special reference of the plate system and extrahepatic duct. A comparative anatomical study of the distribution of the cystic artery in man and other species. Technical innovation for noninvasive and early diagnosis of biliary atresia: the ultrasonographic "triangular cord" sign. Definitive exclusion of biliary atresia in infants with cholestatic jaundice: the role of percutaneous cholecysto-cholangiography. Risk factors for isolated biliary atresia, national birth defects prevention study, 19972002. Cytomegalovirusspecific T-cell reactivity in biliary atresia at the time of diagnosis is associated with deficits in regulatory T cells. Five- and 10-year survival rates after surgery for biliary atresia: a report from the Japanese Biliary Atresia Registry. Medical status of 219 children with biliary atresia surviving long-term with their native livers: results from a North American multicenter consortium. The anatomic pattern of biliary atresia identified at time of Kasai hepatoportoenterostomy and early postoperative clearance of jaundice are significant predictors of transplant-free survival. Total serum bilirubin within 3 months of hepatoportoenterostomy predicts short-term outcomes in biliary atresia. Early prediction of long-term survival and the timing of liver transplantation after the Kasai operation. A multicenter study of the outcome of biliary atresia in the United States, 1997 to 2000. Anatomy of the porta hepatis as a basis for extended hepatoporto-enterostomy for extrahepatic biliary atresia-a new surgical technique. Bacterial cholangitis in patients with biliary atresia: impact on short-term outcome. Prophylactic oral antibiotics in prevention of recurrent cholangitis after the Kasai portoenterostomy. Portoenterostomy for biliary atresia: long-term survival and prognosis after esophageal variceal bleeding. The impact of a previous Kasai procedure on liver transplantation for biliary atresia. Pediatric liver transplantation for biliary atresia: results of primary grafts in 328 recipients. Serial circulating markers of inflammation in biliary atresia-evolution of the postoperative inflammatory process. Extrahepatic anomalies in infants with biliary atresia: results of a large prospective North American multicenter study. Coordinate expression of regulatory genes differentiates embryonic and perinatal forms of biliary atresia. The significance of human jagged 1 mutations detected in severe cases of extrahepatic biliary atresia. Treatment of biliary atresia with special reference to hepatic porto-enterostomy and its modifications. Prolonged neonatal jaundice and the diagnosis of biliary atresia: a single-center analysis of trends in age at diagnosis and outcomes. Patients with biliary atresia have elevated direct/conjugated bilirubin levels shortly after birth. Postoperative corticosteroid therapy for bile drainage in biliary atresia-a nationwide survey. Spontaneous perforation of the bile duct in infancy and childhood: a systematic review. Genetic study of congenital bile-duct dilatation identifies de novo and inherited variants in functionally related genes. Predominant extrahepatic biliary disease in autosomal recessive polycystic kidney disease: a new association. Choledochal cyst disease in children and adults: a 30-year single-institution experience. Fatty acid calcium stones in patients with pancreaticobiliary maljunction/choledochal cyst as another cause of obstructive symptoms besides protein plugs. Magnetic resonance cholangiopancreatography of biliary system abnormalities in children. Autosomal recessive polycystic kidney disease and congenital hepatic fibrosis: summary statement of a first National Institutes of Health/Office of Rare Diseases conference. Nonsyndromatic paucity of interlobular bile ducts: light and electron microscopic evaluation of sequential liver biopsies in early childhood. Bile duct anomalies in a male child with Noonan syndrome: a case for ras and notch pathway synergism.
Eyelid depigmentation following corticosteroid injection for infantile ocular adnexal hemangioma antibiotic resistance first discovered augmentin 1000 mg purchase free shipping. Eyelid necrosis following intralesional corticosteroid injection for capillary hemangioma. Adrenal suppression and growth retardation after injection of periocular capillary hemangioma with corticosteroids. Adrenal suppression and failure to thrive after steroid injections for periocular hemangioma. Corticosteroid resistant orbital hemangioma with proptosis treated with interferon alfa-2-a and partial tarsorrhaphy. Recombinant interferon alfa-2b in the treatment of vision-threatening capillary hemangiomas in childhood. Interferon-alfa treatment of facial infantile haemangiomas: with emphasis on the sight-threatening varieties. Resolution of astigmatism after surgical resection of capillary hemangiomas in infants. Early surgical intervention as definitive treatment for ocular adnexal capillary haemangioma. Chapter 8 Vascular Tumors of the Eyelids 135 Eyelid Congenital Capillary Hemangioma: Superficial Type the superficial type of capillary hemangioma (strawberry hemangioma) has typical clinical features and can show dramatic spontaneous regression. Extensive multifocal capillary hemangioma involving upper eyelid, forehead, and temporal scalp. The upper eyelid is being everted showing diffuse involvement of involved tarsal conjunctiva. It is necessary to evert the eyelid in such cases to determine the full extent of the lesion. Deep capillary hemangioma beneath right lower eyelid imparting blue color to skin. This can look similar to hemorrhage into a lymphangioma, but the lesion had slowly progressed and had no acute bleeding episodes. Same child 10 months later showing regression of tumor, less blepharoptosis, and more exposure of pupil. The triplet on left shows forehead involvement, the middle one showed involvement of left upper eyelid, and the right one has finger hemangiomas that are not seen. Chapter 8 Vascular Tumors of the Eyelids 139 Eyelid Congenital Capillary Hemangioma: Surgical Removal Sometimes a capillary hemangioma can be resected entirely with a good result without waiting for it to grow to a large size. Large deep upper eyelid capillary hemangioma in an infant showing complete blepharoptosis. It occurs in varying numbers in virtually all adults, but the lesions are small and often ignored. The number varies from 1 to 2 in children to hundreds in some elderly individuals. It occurs most commonly on the trunk and extremities, but can occasionally affect the eyelids and periocular region. It can range in size from barely visible to a dome-shaped red mass 5 mm in diameter (3). Acquired capillary haemangioma of the eyelid in an adult treated with cutting diathermy. Clinical Features Solitary acquired hemangioma of the eyelid appears as a distinct red to red-blue papule that may range from 0. Eyelid acquired hemangioma has been observed to develop and rapidly enlarge during pregnancy (6). Pathology In its early stages, acquired hemangioma is very similar histopathologically to the congenital capillary hemangioma of infancy, having numerous newly formed capillaries with narrow lumina and prominent endothelial cells arranged in a lobular fashion in the subpapillary region (3). In a fully matured lesion, the vascular lumina become dilated, the endothelial cells more flattened, and the stroma becomes edematous and hyalinized. Some authorities consider the acquired hemangioma to be closely related to pyogenic granuloma, but it generally shows less endothelial proliferation than the latter (4). The term "capillary hemangioma of the pyogenic granuloma type" has been applied to this lesion (3). Management Management of most acquired hemangiomas is simple periodic observation, because they are generally small and have no malignant potential. When a larger one poses a cosmetic problem, complete excision is an appropriate management. Another tiny red lesion is present at the eyelid margin nasal to the larger lesion. Note the dilated vascular channels with thin endothelial cells and erythrocytes in the lumen. Facial nevus flammeus is sometimes seen in patients with no other abnormalities, but it is often associated with variations of the Sturge-Weber syndrome and occasionally the Klippel-Trenaunay-Weber syndrome. The Sturge-Weber syndrome consists of facial nevus flammeus, and ipsilateral epibulbar telangiectasia, congenital glaucoma, diffuse choroidal hemangioma, leptomeningeal hemangiomatosis with calcification, and seizures. Klippel-Trenaunay-Weber syndrome consists of nevus flammeus and hypertrophy of soft tissues and bone in the extremities, presumably related to arteriovenous fistulas. Although it classically occurs in the cutaneous distribution of cranial nerve V (trigeminal nerve), it can have several variations. Unusual retinal and renal vascular lesions in the Klippel-Trenaunay-Weber syndrome. Clinical Features Clinically, nevus flammeus is a congenital, red to purple lesion that can occur in various areas of the skin. When it corresponds to the facial cutaneous distribution of the trigeminal nerve and is associated with neurologic and ocular changes mentioned above, it comprises the Sturge-Weber syndrome (1,2,4).
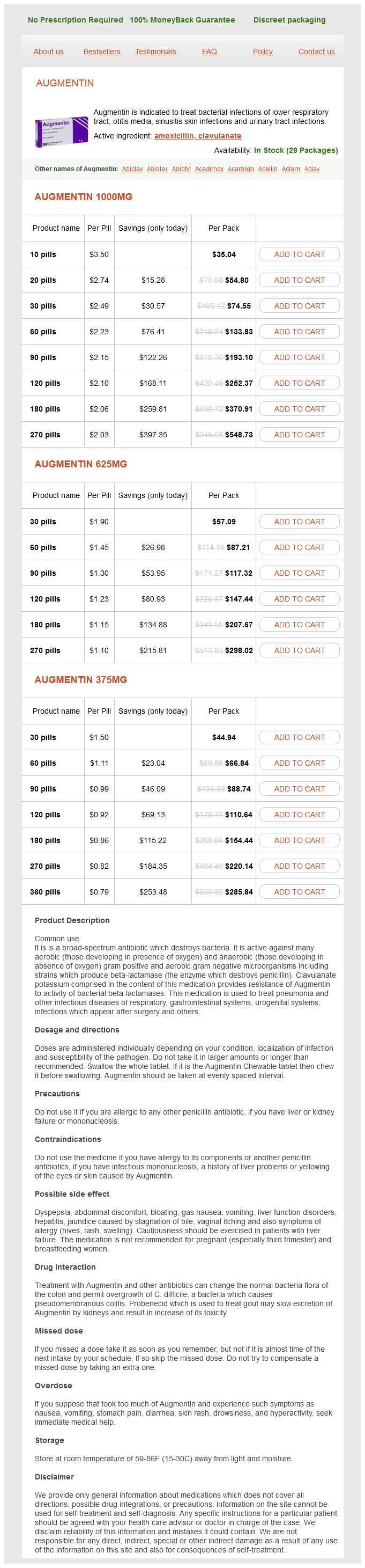
Augmentin Dosage and Price
Augmentin 1000mg
- 10 pills - $35.04
- 20 pills - $54.80
- 30 pills - $74.55
- 60 pills - $133.83
- 90 pills - $193.10
- 120 pills - $252.37
- 180 pills - $370.91
- 270 pills - $548.73
Augmentin 625mg
- 30 pills - $57.09
- 60 pills - $87.21
- 90 pills - $117.32
- 120 pills - $147.44
- 180 pills - $207.67
- 270 pills - $298.02
Augmentin 375mg
- 30 pills - $44.94
- 60 pills - $66.84
- 90 pills - $88.74
- 120 pills - $110.64
- 180 pills - $154.44
- 270 pills - $220.14
- 360 pills - $285.84
Primary closure or reconstruction with cutaneous flaps and grafts allows for cosmetic rehabilitation bacteria zar order augmentin 375 mg with amex. A detailed discussion of reconstruction techniques is beyond the scope of this atlas. In cases where the wound is not readily amenable to primary closure, such as those located in the medial canthal area, the wound can heal spontaneously if left open. This laissez-faire approach can lead to satisfactory cosmetic and functional results in 90% of cases (22). After confirmation of the diagnosis, wide excision and frozen section control or Mohs chemosurgery offer the best control rates (21). Radiotherapy is generally reserved as palliative treatment for aggressive recurrent lesions or for patients who are physically unable to undergo surgery. Metastatic basal cell carcinoma: report of five cases and review of 170 cases in the literature. The association between cigarette smoking and basal cell carcinoma of the eyelids in women. Surgery for primary basal cell carcinoma including the eyelid margins with intraoperative frozen section control: comparative interventional study with a minimum clinical follow up of 5 years. Management of peri-ocular skin tumours by laissez-faire technique: analysis of functional and cosmetic results. However, incomplete removal can be associated with aggressive recurrence, leading to a poorer cure rate. Neglected or incomplete initial excision can result in orbital invasion and rarely death can ensue due to intracranial invasion via emissaries in the orbital bone. Nevoid Basal Cell Carcinoma Syndrome the basal cell nevus syndrome, also known as the Gorlin-Goltz syndrome, or Goltz syndrome, deserves special mention. It is a multisystem, autosomal-dominant syndrome involving both ectoderm and mesoderm tissues (6,7). Other less common ocular abnormalities include congenital cataracts, uveal and optic nerve coloboma, strabismus, nystagmus, and microphthalmos. Imiquimod treatment of superficial and nodular basal cell carcinoma: 12-week open-label trial. The basophilia of the basal cell nuclei give the cellular areas a typical blue color on light microscopy. Curiously, the patient had a simultaneous conjunctival malignant melanoma on the opposite eye. Diffusely infiltrating tumor extending over half of face and destroying the globe. Facial appearance of same patient wearing glasses after exenteration and fitting of the prosthesis. Facial appearance of woman at about age 40 years, showing multiple facial basal cell neoplasms. Facial appearance of same woman at age 86 years, showing extensive involvement and blepharoptosis. X-ray of teeth showing odontogenic keratocyst (clear black area above in area of absence of teeth). Pathology of odontogenic keratocyst, showing keratinizing epithelium and keratin debris in the lumen. Examples of full-thickness eyelid resection and topical imiquimod are illustrated here. The surgical method is shown briefly below and is illustrated in more detail in Chapter 15. Patients who are very old and poor surgical candidates are treated today with topical imiquimod, an agent that boosts the immune system. Appearance several months after treatment showing complete resolution of the lesion. It was excised with frozen section control and closed by primary closure assisted by a temporal semicircular (Tenzel) flap. After circular excision with frozen section control, the large defect and the tight skin made primary closure difficult, so the lesion was allowed to heal by granulation without sutures. The lesion was removed with frozen section control and a free skin graft from upper eyelid of opposite eye was used to close the defect. It can occur at a younger age in patients who are immunosuppressed or who have excess sensitivity to sunlight, particularly albinos. The squamous cells have eosinophilic cytoplasm, intercellular bridges, and can have keratin pearls. Although the tumor foci appear to be discrete microscopically, they actually represent fingerlike extensions passing down from the epidermis. A more poorly differentiated tumor may require immunohistochemistry or electron microscopy to identify the squamous cell origin of the lesion and to rule out other malignant neoplasms. It begins as a sessile or papular lesion that is similar to early basal cell carcinoma. It frequently ulcerates centrally, producing the rodent ulcer appearance; it can be irritating and bleed. This can lead to numbness, pain, blepharoptosis, diplopia, and displacement of the globe. More sizable lesions in which extensive eyelid reconstruction is anticipated should be diagnosed by a shaving or punch biopsy to establish the diagnosis before embarking on definitive surgical management (16). The lesion should then be surgically excised using Mohs microsurgery or frozen section control. Eyelid reconstruction should be undertaken when the margins are confirmed to be negative for tumor. The indications and techniques of these methods are discussed in more detail elsewhere.