Avodart
General Information about Avodart
However, like any other treatment, Avodart additionally has its share of potential unwanted aspect effects. The most typical reported unwanted effects of Avodart embody sexual dysfunction, similar to decreased libido, erectile dysfunction, and decreased semen volume. These unwanted effects are usually delicate and have a tendency to resolve once the treatment is stopped. In uncommon cases, Avodart can even cause allergic reactions, breast enlargement or tenderness, and melancholy.
One of the primary advantages of Avodart over other BPH medications is its long period of action. While other BPH medicines must be taken regularly, Avodart solely must be taken once a day, making it extra convenient for patients. Studies have additionally proven that Avodart offers extended aid of symptoms, with some patients experiencing improvement for as a lot as four years.
Avodart has been in use since 2002 and has been extensively prescribed by doctors to deal with BPH. The medication is taken orally in the form of a capsule, and it works by inhibiting the activity of the enzyme 5 alpha-reductase, which converts testosterone to DHT. By blocking the production of DHT, Avodart effectively reduces the scale of the prostate gland, thus improving urinary signs and circulate fee. It also helps to minimize back the danger of acute urinary retention and the necessity for surgical procedure associated to BPH.
It is essential to hunt medical advice earlier than beginning to take Avodart. The treatment just isn't appropriate for everyone, and people with certain medical circumstances, corresponding to liver illness, shouldn't take it. It also can work together with different medicines, so it is essential to inform your physician of all medicines you may be at present taking.
BPH is a standard condition that impacts males, especially as they age. It is estimated that more than half of males over the age of 50 will expertise BPH. BPH is a non-cancerous situation, however it could cause numerous urinary signs similar to frequent urination, a weak urine stream, and a feeling of incomplete emptying of the bladder. These signs can significantly affect a man's quality of life, and if left untreated, they will result in more serious issues corresponding to urinary tract infections and urinary retention.
Avodart has additionally been just lately accredited by the FDA for use together with another medication, tamsulosin, for the therapy of BPH. This combination has been proven to be more effective in improving urinary symptoms than both medication alone. Tamsulosin is an alpha-blocker that helps to relax the muscle tissue in the prostate and bladder, making it simpler to urinate.
Avodart, also known as Dutasteride, is a medication generally used to treat Benign Prostatic Hyperplasia (BPH), a situation in which the prostate gland becomes enlarged. It is a prescription drug and has been clinically confirmed to be an effective remedy for BPH in men. Avodart belongs to a class of medicine generally known as 5 alpha-reductase inhibitors which work by blocking the production of a male hormone referred to as DHT (dihydrotestosterone) which is liable for prostate gland enlargement.
In conclusion, Avodart is an effective and well-tolerated medication for the remedy of BPH. It has helped many men worldwide to enhance their symptoms and quality of life. It is important to do not overlook that BPH is a progressive situation, and early therapy with medicines like Avodart might help to stop the event of severe complications. Therefore, it's essential to seek medical recommendation if you expertise any urinary signs. With correct prognosis and therapy, BPH may be effectively managed, permitting males to lead energetic and fulfilling lives.
The majority of cases with hemoptysis need bronchoscopy to localize bleeding and exclude a tracheobronchial rupture medicine x xtreme pastillas order generic avodart on line, which can be clinically silent for weeks. Pneumonorrhaphy (suture repair of the lung) is preferred for minor injuries with lobectomy and pneumonectomy performed for more severe injuries. However, it can also occur after blunt thoracic trauma in which sheer forces of acceleration or deceleration leave intraparenchymal lacerations involving airways or vasculature. Continued bleeding into the lung can present with rupture into the pleural space (hemothorax), intraparenchymal hematoma formation, or hemoptysis. In this condition, splenic tissue is transported across the diaphragm after penetrating injury, where it becomes functional and vascularized within the lung. Assessments and interventions are frequently performed empirically because the cause of hemoptysis may not be known at the time of presentation. Therapy to control minor and moderate hemoptysis can usually proceed along diagnostic paths. Massive hemoptysis should be managed within a framework of expeditious therapy to stabilize and resuscitate the patient. A multidisciplinary collaborative approach involving intensivists, pulmonologists, interventional radiologists, and thoracic surgeons is optimal to improve outcomes. Sputum containers should be placed at the bedside of patients who are not intubated to allow measurement of blood loss and an estimate of the bleeding rate. High bleeding rates, hemodynamic instability, and severe oxygenation failure signal the need for rapid evaluation and treatment. In addition to the management steps outlined later, laboratory studies should be obtained, including complete blood cell count, Vascular Monitoring Catheters Use of pulmonary artery catheters has decreased significantly and complications causing hemoptysis occur rarely. More distal and prolonged inflation of the catheter balloon can cause fatal pulmonary artery dissection, pseudoaneurysm formation, or pulmonary artery rupture. Preventive measures include placement of the catheter at an insertion distance when full inflation is required to obtain an occlusion pressure, slowly inflating the balloon (never inflating against resistance), full inflation of the balloon to prevent the catheter tip from projecting beyond the balloon, and daily monitoring of catheter position with chest radiography. If hemoptysis occurs with a pulmonary artery catheter in place, rapid diagnosis and treatment are required. Risk factors for pulmonary artery rupture include concomitant anticoagulation, cardiopulmonary bypass, balloon migration, hypothermia, advanced age, and pulmonary hypertension. An arterial blood gas measurement may be needed to assess ventilation and acid-base status, although pulse oximetry is usually adequate to assess oxygenation. Additional studies may be needed to investigate possible causes of hemoptysis such as infection or vasculitis. The hemodynamic status of the patient should be evaluated and fluids or blood administered for hypotension or evidence of impaired oxygen delivery. Patients with mild to moderate amounts of hemoptysis usually do not require intubation, but intubation in massive hemoptysis is usually needed to facilitate diagnostic and therapeutic interventions as well as to provide support for oxygenation and ventilation. Additional steps may be needed to prevent contamination of the unaffected lung from blood and to preserve respiratory function. Airway and Lung Protection Patency of the airway and the ability to protect the airway should be assessed as soon as hemoptysis is noted. All patients should be provided with supplemental oxygen as needed to maintain adequate Patient Positioning If the source of bleeding is localized to one lung, the patient with massive bleeding should be positioned with the bleeding side down to keep bleeding contained to one lung. Furthermore, if the pulmonary circulation is bleeding, it can be influenced by gravity by placing the bleeding segment higher than other areas of the chest. By converting that segment to a zone 1 condition in which alveolar pressure is higher than pulmonary artery pressure, bleeding may be decreased. Orotracheal intubation is preferred to allow use of a larger endotracheal tube (preferably 8 mm inner diameter or larger) to facilitate suctioning, ventilation, and bronchoscopy. The orotracheal route also allows for selective mainstem bronchial intubation if needed. Mechanisms to localize ventilation to one lung using a single-lumen endotracheal tube include selective intubation of one of the mainstem bronchi and selective endobronchial tamponade with a bronchial blocker (see later discussion). Because of the leftward displacement of the carina in most individuals, an endotracheal tube advanced blindly will almost always intubate the right main bronchus. Unfortunately, the right upper lobe bronchus is so close to the carina that a right mainstem intubation may also cause right upper lobe atelectasis. The ability to ventilate and oxygenate a patient with the right lower and right middle lobes alone depends on the underlying cardiopulmonary reserve. Intubation of the left main bronchus is facilitated by placing the patient in a right lateral decubitus position to shift the mediastinum rightward. Angulation of the endotracheal tube curvature toward the left and progression of the tube over a coudé catheter may be helpful. Double-Lumen Endotracheal Tubes Devices used for single-lung ventilation have also been applied to the management of hemoptysis. Successful placement of this type of endotracheal tube requires training and experience. The smaller suction ports of each independent lumen can cause difficulty in suctioning blood. Endobronchial evaluation requires a pediatric bronchoscope or double-lumen tube removal once bleeding has been controlled. Proximal airway masses may preclude placement of a double-lumen endotracheal tube. A pH assessment of the blood (low pH expected in gastric hemorrhage) and observation of expectorated sputum can be performed at the bedside.
Compared with control subjects treatment for 6mm kidney stone avodart 0.5 mg mastercard, the systemic sympathetic nervous system is activated in patients with mitral regurgitation. Native beta-adrenergic support for left ventricular dysfunction in experimental mitral regurgitation normalizes indexes of pump and contractile function. Effects of chronic beta-adrenergic blockade on the left ventricular and cardiocyte abnormalities of chronic canine mitral regurgitation. Anterolateral papillary muscle rupture complicated by the obstruction of a single diagonal branch. Ischemic mitral regurgitation on the threshold of a solution: from paradoxes to unifying concepts. The case for an aggressive surgical approach to papillary muscle rupture following myocardial infarction: "From paradise lost to paradise regained. Comparison of transthoracic and transesophageal echocardiography for assessment of left-sided valvular regurgitation. Intra-aortic balloon pumping in acute mitral regurgitation reduces aortic impedance and regurgitant fraction. Treatment of severe mitral regurgitation caused by ischemic papillary muscle dysfunction: indications for coronary angioplasty. Six month pilot study of captopril for mildly symptomatic, severe isolated mitral and isolated aortic regurgitation. Effect of enalapril therapy on left ventricular mass and volumes in asymptomatic chronic, severe mitral regurgitation secondary to mitral valve prolapse. Acute effects of cardiac resynchronization therapy on functional mitral regurgitation in advanced systolic heart failure. Role of cardiac dyssynchrony and resynchronization therapy in functional mitral regurgitation. Beta-blockade therapy in chronic heart failure: diastolic function and mitral regurgitation improvement by carvedilol. Is prophylactic beta-adrenergic blockade appropriate in mitral regurgitation: impact of cellular pathophysiology. Differential effects of the angiotensin-converting enzyme inhibitor lisinopril versus the beta-adrenergic receptor blocker atenolol on hemodynamics and left ventricular contractile function in experimental mitral regurgitation. Impact of mitral valve annuloplasty on mortality risk in patients with mitral regurgitation and left ventricular systolic dysfunction. The effect of chordal preservation on late outcome after mitral valve replacement: a randomized study. Two-year outcomes of surgical treatment of moderate ischemic mitral regurgitation. Echocardiographic prediction of left ventricular dysfunction after mitral valve repair for mitral regurgitation as an indicator to decide the optimal timing of repair. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation. Pre-operative atrial fibrillation as the key determinant of outcome of mitral valve repair for degenerative mitral regurgitation. Importance of right ventricular performance measurement in selecting asymptomatic patients with mitral regurgitation for valve surgery. Effects of valve surgery on left ventricular contractile function in patients with long-term mitral regurgitation. Unexpected, dismal left ventricular function after surgery for mitral regurgitation: there is just no excuse for it anymore. Influence of hospital procedural volume on care process and mortality for patients undergoing elective surgery for mitral regurgitation. Valvular-ventricular interaction: the importance of the mitral chordae tendineae in terms of global left ventricular systolic function. Mitral valve replacement with and without chordal preservation in patients with chronic mitral regurgitation. Selecting patients with mitral regurgitation and left ventricular dysfunction for isolated mitral valve surgery. Survival after coronary revascularization, with and without mitral valve surgery, in patients with ischemic mitral regurgitation. The double-orifice technique in mitral valve repair: a simple solution for complex problems. Surgical isolated edge-to-edge mitral valve repair without annuloplasty: clinical proof of the principle for an endovascular approach. Unexplained hypotension: the spectrum of dynamic left ventricular outflow tract obstruction in critical care settings. Nonobstructive hypertrophic cardiomyopathy out of the shadows: known from the beginning but largely ignored. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. Hypertrophic cardiomyopathy is predominantly a disease of left ventricular outflow tract obstruction. Application of genetic testing in hypertrophic cardiomyopathy for preclinical disease detection. Clinical course and prognosis of hypertrophic cardiomyopathy in an outpatient population. Historical perspectives on sudden deaths in young athletes with evolution over 35 years. Diastolic coronary vascular reserve: a new index to detect changes in the coronary microcirculation in hypertrophic cardiomyopathy.
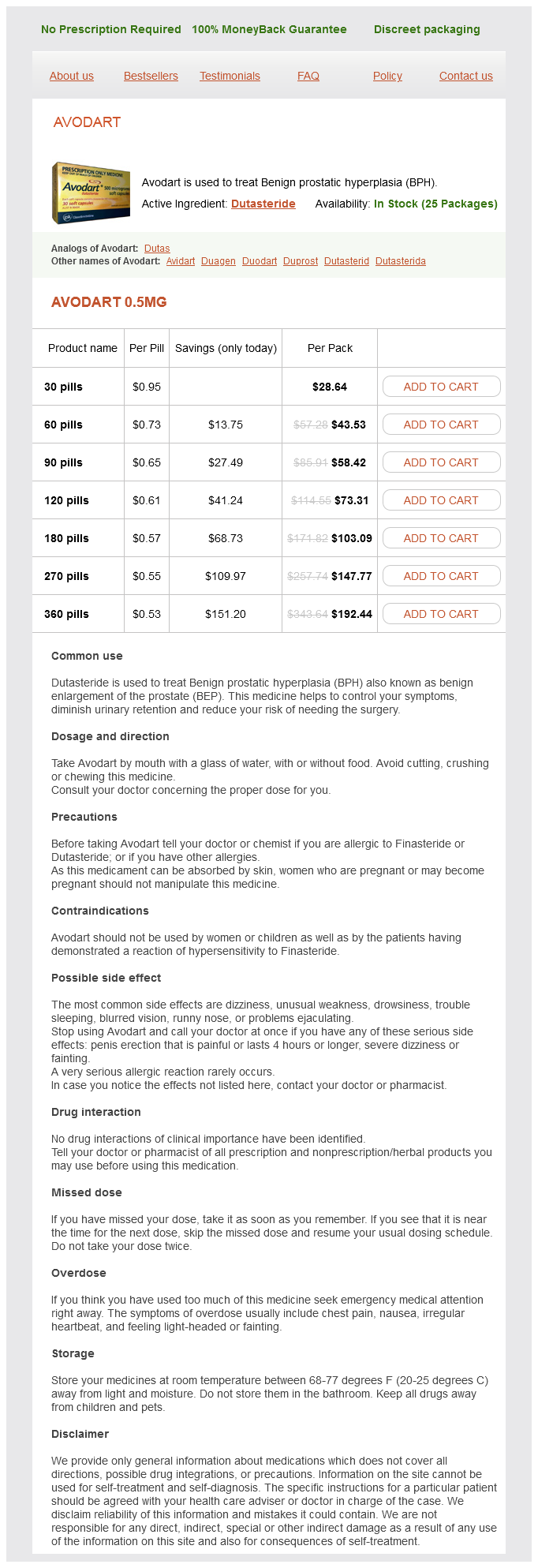
Avodart Dosage and Price
Avodart 0.5mg
- 30 pills - $28.64
- 60 pills - $43.53
- 90 pills - $58.42
- 120 pills - $73.31
- 180 pills - $103.09
- 270 pills - $147.77
- 360 pills - $192.44
In: Abstracts and Proceedings of the 34th Annual Meeting of the Infectious Disease Society of North America symptoms indigestion avodart 0.5 mg low price. In: Abstracts and Proceedings of the 7th Annual Meeting of the Society for Healthcare Epidemiology of America. Reduction of nosocomial infection during pediatric intensive care by protective isolation. The role of gown and glove isolation and strict handwashing in the reduction of nosocomial infection in children with solid organ transplantation. Nosocomial pneumonia is not prevented by protective contact isolation in the surgical intensive care unit. In: Abstracts and Proceedings of the 43rd InterScience Conference on Antimicrobial Agents and Chemotherapy. A prospective study to determine whether cover gowns in addition to gloves decrease nosocomial transmission of vancomycin-resistant enterococci in an intensive care unit. Infection-control measures reduce transmission of vancomycin-resistant enterococci in an endemic setting. Evaluation of dressing regimens for prevention of infection with peripheral intravenous catheters. Needlestick injury in acute care nurses caring for patients with diabetes mellitus: a retrospective study. A five-year study of needlestick injuries: significant reduction associated with communication, education, and convenient placement of sharps containers. Efficacy of safety-engineered device implementation in the prevention of percutaneous injuries: a review of published studies. Advisory Committee on Immunization Practices: recommended adult immunization schedule: United States, 2012. Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Effectiveness of influenza vaccine in health care professionals: a randomized trial. Health care worker beliefs about influenza vaccine and reasons for non-vaccination-a cross-sectional survey. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. Vaccinating healthcare workers against influenza to protect the vulnerable-is it a good use of healthcare resources Pertussis outbreak among adults at an oil refinery-Illinois, August-October 2002. Nosocomial pertussis: costs of an outbreak and benefits of vaccinating health care workers. Health and economic consequences of an outbreak of pertussis among healthcare workers in a hospital in France. Risk factors for hepatitis C virus infection among health care personnel in a community hospital. Evaluation of a mechanical handwashing device with germicidal and non-germicidal products. In: Program and Abstracts of the 15th Annual Meeting of the Association for the Professionals in Infection Control. Clinical evaluation of the degerming efficacy of seven agents for handwashing in hospitals. In: Program and Abstracts of the 24th Interscience Conference on Antimicrobial Agents and Chemotherapy. The efficacy of several new handwashing agents for removing non-transient bacterial flora from hands. In: Abstracts and Proceedings From the 29th Interscience Conference on Antimicrobial Agents and Chemotherapy. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. The clinical and economic impact of deep chest surgical site infections following coronary artery bypass graft surgery. Surgical-site infection due to Staphylococcus aureus among elderly patients: mortality, duration of hospitalization, and cost. A prospective study of outcomes, healthcare resource utilization, and costs associated with postoperative nosocomial infections. Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. Mortality rate attributable to ventilatorassociated nosocomial pneumonia in an adult intensive care unit: a prospective case-control study.