Azithromycin
General Information about Azithromycin
One factor that units azithromycin aside from different antibiotics is its handy dosing routine. It is usually prescribed in a once-daily dose, for a shorter length than other antibiotics, making it a handy choice for patients who've bother sticking to a more frequent dosing schedule. This also reduces the chance of creating antibiotic resistance, which might happen when a drugs is taken for a prolonged time frame.
Azithromycin's effectiveness against respiratory infections is due to its capability to penetrate into the tissues and fluids of the lungs. This allows it to combat bacteria which have settled in these areas and could additionally be inflicting symptoms corresponding to coughing, congestion, and difficulty respiratory. In addition, azithromycin has anti-inflammatory properties, which can help relieve signs and velocity up restoration time.
One of the most common uses of azithromycin is for infections of the upper and decrease respiratory tract. It is a first-line treatment for widespread circumstances such as ear infections, sinusitis, and bronchitis. These infections could be caused by a wide selection of micro organism, together with Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, all of which are prone to azithromycin.
Azithromycin is also commonly used to deal with infections of the pores and skin and soft tissue, similar to cellulitis and impetigo. It may be prescribed as a standalone remedy or together with different drugs, relying on the severity and sort of infection. Its efficacy towards skin infections is due to its ability to target and kill the bacteria that generally trigger these circumstances, similar to Staphylococcus aureus and Streptococcus pyogenes.
Azithromycin is mostly well-tolerated and has a comparatively low threat of side effects. The commonest unwanted effects reported embody abdomen upset, diarrhea, and nausea. These symptoms are often delicate and resolve rapidly. In uncommon instances, azithromycin may cause allergic reactions, which might vary from gentle rashes to extreme anaphylaxis. It is necessary to seek medical attention if any regarding unwanted aspect effects occur while taking this medicine.
In conclusion, azithromycin is a extensively used and efficient antibiotic for the therapy of various bacterial infections, particularly these affecting the respiratory system. Its convenient dosing routine and low danger of side effects make it a popular alternative among healthcare suppliers and patients alike. However, as with all medicines, it is important to use azithromycin solely as directed and under the supervision of a healthcare skilled.
Another frequent use for azithromycin is in the treatment of pneumonia. Pneumonia is a serious infection of the lungs that may be attributable to various bacteria, viruses, and fungi. Azithromycin is especially efficient in opposition to Mycoplasma pneumoniae and Legionella pneumophila, two frequent bacterial causes of pneumonia, and is commonly prescribed as a first-line remedy for these infections.
Azithromycin, generally known by its model name Zithromax, is a generally prescribed macrolide antibiotic used to deal with a big selection of infections. It is efficient in opposition to both gram-positive and gram-negative bacteria, making it a flexible and broadly used medication.
Aside from its use as an antibiotic, azithromycin has also been discovered to have anti-inflammatory and immunomodulatory effects. This implies that it can help scale back irritation and enhance the physique's immune response to infections. This could additionally be significantly beneficial for patients with chronic respiratory situations, such as asthma, who are at a higher risk of creating infections and experiencing extra extreme signs.
The most cost-effective initial approach is percutaneous drainage and alcohol instillation to attempt to ablate the cyst infection rates in hospitals azithromycin 500 mg order line. Placement of a permanent biliary stent is not appropriate for this benign condition. Surgical resection is most appropriate for the -cateninactivated inflammatory hepatocellular adenoma described here, which carries a risk of malignant transformation. Fatty liver disease is another cause of steatosis but is less likely without other features of the metabolic syndrome. While this patient should avoid acetaminophen because of his alcohol use, a patient with acetaminophen hepatotoxicity would typically present with higher levels of transaminases and liver synthetic function abnormalities. Acute hepatitis also generally produces higher levels of liver enzymes and often jaundice. Liver transplant could be considered if the patient does not have a response to medical management, as assessed by a decrease in bilirubin levels and the calculated Lille score after 7 days. Acamprosate may have a role in refractory alcoholism but should be considered only with an experienced addiction psychiatrist. While the patient is overweight and may benefit from weight loss, this is not as critical as discontinuation of alcohol. Vitamin E may have some role in nonalcoholic fatty liver but is not recommended for alcoholic liver disease. Patients with chronic hepatitis C should not consume alcohol because synergistic liver damage can occur. This patient has some relative contraindications to interferon-based therapy, and since she has only minimal fibrosis, there is no urgency for treatment. Discontinuation of alcohol further drives acetaminophen toward its toxic metabolites. Mildly elevated ferritin may be present with chronic alcohol use but does not suggest hereditary hemochromatosis. Ballooning degeneration and Mallory bodies are features of alcoholic hepatitis, which he does not have. Interface hepatitis with plasma cells would be seen in autoimmune hepatitis, which is less likely in this patient. The normal alpha-fetoprotein level should not dissuade you from the diagnosis, particularly in this high-risk patient. The portal vein thrombosis is due to tumor thrombus, as evidenced by arterial enhancement of the clot. Tumor thrombosis is by definition extrahepatic spread of the malignancy, so neither hepatectomy nor transplant is indicated. Anticoagulation or thrombolytic therapy does not have a role in the management of tumor thrombosis. When isolated gastric fundal varices are found, they should raise the possibility of sinistral hypertension from splenic vein thrombosis, especially in the absence of known liver disease. With a prior episode of pancreatitis, this patient has a risk factor for splenic vein thrombosis. Hepatic venography would confirm the diagnosis, but the diagnosis is fairly secure according to the constellation of clinical findings and the lack of visualization of the hepatic veins on Doppler ultrasonography. Thrombolytic therapy is used in acute hepatic vein thrombosis and should be delivered by catheter-directed therapy rather than by systemic dosing. The acute inflammatory state due to her diverticulitis is the precipitating factor. Patients with acute portal vein thrombosis should receive anticoagulation therapy to prevent progression of thrombosis and the development of portal hypertension. In the presence of an intra-abdominal inflammatory process, a bone marrow examination for hematologic disorders is not necessary. Systemic thrombolytic therapy is also not recommended in the absence of acute hepatic decompensation. Colonoscopy is relatively contraindicated in the presence of acute diverticulitis. Band ligation is not effective for large fundic varices (because of the submucosal location of the varices). Surgical expertise for splenorenal shunting typically requires transfer to a tertiary referral center and is best suited for nonemergent situations. While this patient will ultimately benefit from transplant, controlling the active hemorrhage requires emergent treatment. This patient with known cirrhosis presented with an acute upper gastrointestinal tract hemorrhage. Small esophageal varices were noted on examination, and there was evidence of recent bleeding (heme staining in the stomach). Since no other bleeding lesions were identified, the varices are the likely source and should be treated endoscopically to prevent rebleeding. While nonselective -blockade would be appropriate as part of long-term secondary prophylaxis, it does not replace endoscopic therapy, particularly in an acute bleeding episode. This patient will ultimately benefit from transplant, but controlling the active hemorrhage requires emergent treatment. This patient presents with chronic gastrointestinal tract bleeding in the presence of cirrhosis. This patient is having unacceptable adverse effects from the -blocker therapy being used as primary prophylaxis. Given his large varices, his therapy should be changed to an alternate form of primary prophylaxis-in this case, band ligation. Dose reduction may improve his symptoms, but the -blockade would likely be inadequate to prevent variceal hemorrhage (goal heart rate, about 60 beats per minute).
Ulcerative colitis can be divided into ulcerative proctitis (rectal involvement only) bacteria urine hpf purchase azithromycin 500 mg amex, ulcerative proctosigmoiditis (involving the rectum and sigmoid colon), left-sided ulcerative colitis (inflammation from the rectum to the splenic flexure), and extensive colitis or pancolitis (inflammation extends from the rectum to beyond the splenic flexure or involves the entire colon). Most cases of luminal Crohn disease can be divided into ileitis, colitis, and ileocolitis. Much less common is involvement of the jejunum or the upper gastrointestinal tract. A subset of patients has perianal disease with fissures, fistulas, abscesses, and other findings. With the exception of the Pentasa formulation of mesalamine, these medications primarily deliver drug to the colon. This drug was originally developed to treat rheumatoid arthritis, and for that indication, the sulfapyridine moiety is thought to be the active component. The choice of drug therefore depends primarily on the distribution of inflammation. Drug-associated toxicity is common with sulfasalazine, including headache, epigastric pain, nausea and vomiting, and skin rash. Less common but severe adverse events include hepatitis, fever, autoimmune hemolysis, bone marrow toxicity, and others. Folate deficiency is induced by sulfasalazine, and therefore folate supplementation is required. Olsalazine, balsalazide, and mesalamine generally are better tolerated than sulfasalazine. Less common is a hypersensitivity reaction resulting in worsening diarrhea and abdominal pain that may be confused with a colitis flare. Rarely, serious adverse events occur, including interstitial nephritis, pericarditis, pneumonitis, hepatitis, or pancreatitis. Periodic monitoring of renal function is recommended with long-term treatment with any mesalamine formulation, although nephrotoxicity is rare. Olsalazine, balsalazide, and mesalamine may be taken during pregnancy and breastfeeding. Because of these results, the use of antibiotic therapy for Crohn disease is debated, and in the absence of penetrating complications, such as a fistula or abscess, the role of antibiotics as primary therapy in Crohn disease is limited. In contrast, uncontrolled studies and clinical experience indicate that antibiotics such as metronidazole and ciprofloxacin are effective for fistulizing Crohn disease, particularly perianal fistulas. No controlled trials have been performed, but antibiotic therapy is used widely for this treatment indication and is considered to be the first-line therapy in combination with immunosuppressive or biological therapies. Small placebo-controlled and comparative trials have shown that metronidazole and ciprofloxacin are effective for inducing remission in patients with acute pouchitis after colectomy and ileoanal anastomosis for ulcerative colitis. Uncontrolled clinical observations have suggested that metronidazole and ciprofloxacin may be effective for maintaining remission in patients with chronic pouchitis. Adverse events observed with metronidazole include paresthesias, peripheral neuropathy, yeast infections, anorexia, dyspepsia, nausea, a metallic taste, and intolerance to alcohol. Adverse events observed with ciprofloxacin are less common and include photosensitivity, nausea, rash, increased liver enzymes, and tendinopathy, rarely including tendon rupture. Metronidazole can be considered during pregnancy, but it is secreted in breast milk. Antibiotics Controlled trials of various antibiotics have not demonstrated efficacy in treating ulcerative colitis. Three small studies suggested efficacy of metronidazole and ciprofloxacin; however, a placebo-controlled trial of metronidazole did not demonstrate efficacy for inducing remission in active Crohn disease. Similarly, another trial did not demonstrate an adjunctive role for antibiotics in patients receiving budesonide for active Crohn disease. A dose-response study of patients with active ulcerative colitis showed that a prednisone dosage of 40 or 60 mg daily is more effective than 20 mg daily, with more adverse events with a 60-mg dose. Doses larger than 60 mg provide little if any additional efficacy, with more side effects, and should not be used. Most clinicians initiate oral corticosteroid therapy with prednisone at a dosage of 40 to 60 mg daily. For patients with ileocolonic Crohn disease, controlled ileal-release budesonide is an alternative to prednisone, and for patients with ulcerative colitis, 162 Section V. Both formulations of budesonide offer effective therapy with fewer steroid-related side effects (owing to high first-pass hepatic metabolism), although at a higher cost. Placebo-controlled trials have shown that corticosteroid therapy is not effective for maintaining remission in ulcerative colitis or Crohn disease; thus, for patients who respond to steroid therapy, the dose is typically tapered over 2 to 4 months while use of another medication is begun for maintenance. Patients with severely active disease who do not respond to oral corticosteroid therapy are often either hospitalized and given corticosteroids intravenously (eg, methylprednisolone, 40-60 mg daily) or treated with a biological agent. Corticosteroid enemas are effective for inducing remission in left-sided ulcerative colitis or ulcerative proctosigmoiditis, and corticosteroid suppositories are effective for ulcerative proctitis. However, in clinical trials, topical mesalamine is superior to topical corticosteroids, and thus topical corticosteroids are typically reserved for patients who do not tolerate or respond to mesalamine. Short- and long-term adverse events occur frequently in patients receiving corticosteroids. Short-term adverse events include weight gain, moon face, acne, ecchymoses, hypertension, hirsutism, petechial bleeding, striae, and psychosis. Long-term adverse events include diabetes mellitus, increased risk of infection, osteonecrosis, osteoporosis, myopathy, cataracts, and glaucoma, among many others. In contrast, higher-dose (25 mg weekly) parenteral methotrexate is effective for inducing and maintaining remission in Crohn disease.
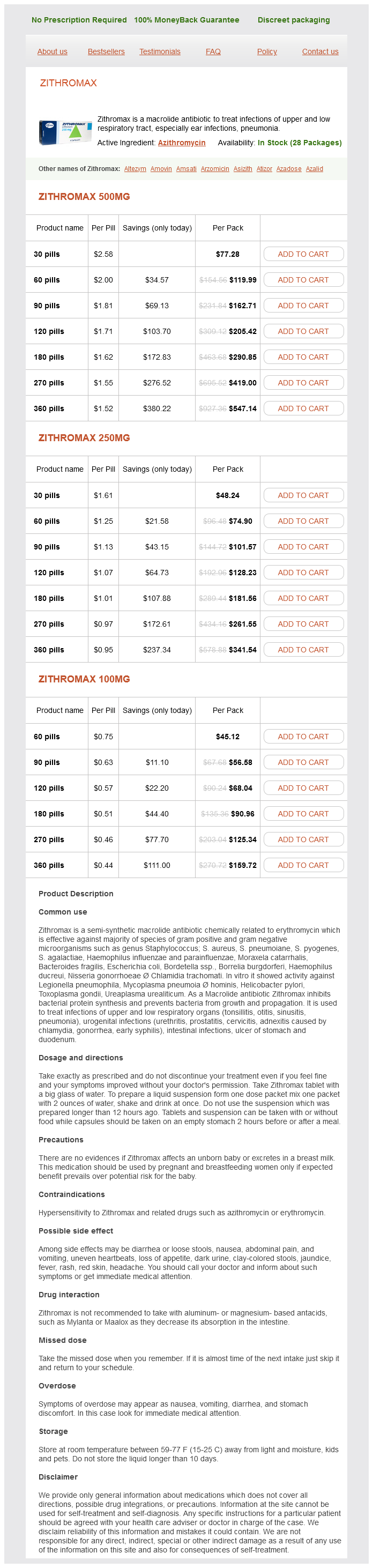
Azithromycin Dosage and Price
Zithromax 500mg
- 30 pills - $77.28
- 60 pills - $119.99
- 90 pills - $162.71
- 120 pills - $205.42
- 180 pills - $290.85
- 270 pills - $419.00
- 360 pills - $547.14
Zithromax 250mg
- 30 pills - $48.24
- 60 pills - $74.90
- 90 pills - $101.57
- 120 pills - $128.23
- 180 pills - $181.56
- 270 pills - $261.55
- 360 pills - $341.54
Zithromax 100mg
- 60 pills - $45.12
- 90 pills - $56.58
- 120 pills - $68.04
- 180 pills - $90.96
- 270 pills - $125.34
- 360 pills - $159.72
A prospective randomized clinical trial of myotomy with and without Dor (or anterior) fundoplication showed that patients with the Dor procedure had much less gastroesophageal reflux antibiotic 750 mg 100 mg azithromycin with visa, as assessed with 24-hour esophageal pH testing, than those without fundoplication (9% vs 48%). This has led to the common practice in most centers of coupling the modified Heller myotomy with fundoplication. Only 2 randomized prospective trials have compared esophagomyotomy with pneumatic dilation. These studies showed that both treatments were equally effective in relieving symptoms initially, but in the study with the longer follow-up, patients who had esophagomyotomy had fewer recurrent symptoms than those who had pneumatic dilation. Overall, there is no difference in life expectancy or mortality for patients with treated achalasia than for the general population. However, there is clear evidence that patients with achalasia (treated or untreated) are at increased risk for esophageal squamous cell carcinoma. There is no consensus about screening; however, most experts recommend endoscopy at least once in the decade following the diagnosis of achalasia. Furthermore, if new or worsening dysphagia develops in a patient with achalasia, upper endoscopy should be performed. The primary drawbacks of pneumatic dilation are the risk of esophageal perforation (approximately 2%) and lack of durability, compared with surgical treatment, according to most studies. A longitudinal incision is initiated on the gastric side approximately 2 cm distal to the gastroesophageal junction and extended proximally 7 cm above the junction. Over the past 20 years, this procedure has been performed safely and successfully with laparoscopy. Long-term studies (10 years of follow-up) have shown that surgical myotomy produces symptomatic relief in 80% to 85% of patients. In nearly 50% of patients who have a modified Heller myotomy, gastroesophageal reflux disease develops; in some patients, Diffuse esophageal spasm is likely a rare disease. The typical symptom complex for this condition is intermittent chest pain (it may radiate to the back or throat) associated with dysphagia. The pathophysiology of diffuse esophageal spasm is poorly understood, but the condition may reflect a forme fruste (ie, an incomplete form) of achalasia. Over the past several decades, it has become clear that diffuse esophageal spasm is a misnomer because the spastic component affects only the smooth muscle in the distal two-thirds of the esophagus. A small study of patients with diffuse esophageal spasm suggested that there may be dysfunction in the endogenous synthesis or degradation of nitric oxide. This finding explains why nitrates often provide benefit in the treatment of diffuse esophageal spasm. The hallmark of diffuse esophageal spasm is the presence of simultaneous contractions in more than 20% of swallows. There must be at least 1 swallow with peristalsis (in distinction from achalasia). However, because the results of radiographic studies may be normal in diffuse esophageal spasm, normal findings do not rule out the diagnosis. Recently, it has been renamed jackhammer esophagus by authors of the Chicago Classification. Nutcracker esophagus was first described more than 3 decades ago, and since that time, there has been considerable controversy about the association of this manometric finding with symptoms. In a study that examined the manometric findings from patients with unexplained chest pain, nutcracker esophagus was the most common abnormal finding, occurring in 12% of patients. Many patients with the manometric finding of nutcracker esophagus do not have chest pain. In an unpublished study at Mayo Clinic, 15% of asymptomatic patients who underwent esophageal manometry before 24-hour impedance pH testing met the manometric criteria for nutcracker esophagus. A study with 24-hour ambulatory esophageal manometry found that patients who had nutcracker esophagus or diffuse esophageal spasm according to stationary manometry frequently switched patterns over 24 hours, suggesting that nutcracker esophagus may be a marker for esophageal spasm. With the use of high-frequency intraluminal ultrasonography to examine patients who have nutcracker esophagus, asynchrony was found in the contractions of the circular and longitudinal muscle layers of the esophagus, and this was reversed with atropine, suggesting that the manometric abnormality may be due to a hypercholinergic state. Nevertheless, the etiology and specific treatment of this manometrically defined disease is still unclear. Treatment should not be initiated for this manometric finding unless there are other supporting objective and symptomatic criteria to support an associated dysfunction. Treatment Because the pathophysiology of discoordinated and hypercontractile esophageal motility disorders is poorly understood and 3. Note the simultaneous, multipeaked contractions of prolonged duration with intermittent peristalsis. B, High-resolution manometry Clouse plot from a patient with diffuse esophageal spasm with high-amplitude simultaneous contractions. Barium esophagram showing "corkscrew" esophagus in a patient with diffuse esophageal spasm. Diltiazem was studied in a randomized, double-blind crossover study (60-90 mg 4 times daily), and, compared with placebo, diltiazem relieved chest pain in patients with nutcracker esophagus. There have been anecdotal reports of the usefulness of nitrates and anticholinergic agents, but these have not been studied in a controlled trial. Gastroesophageal reflux disease has been suggested to have a role in spastic disorders of the esophagus, and some small studies have shown symptomatic improvement with proton pump inhibitor therapy. Trazodone (100-150 mg daily) and imipramine (50 mg daily) have been shown to be effective in improving chest pain in patients with esophageal motility disorders, likely by modifying visceral sensation. This group of patients can be classified into those with hypersensitive esophagus or those with functional dysphagia. Esophagus Injection of botulinum toxin also has been studied in this group of patients. The patients received 100 units of botulinum toxin injected at the Z line (given as 5 circumferential injections, with 20 units/mL in each); 70% of the patients had some improvement and nearly 50% had complete relief. Patients who have profound symptoms (eg, severe dysphagia associated with weight loss or aspiration associated with severe dysphagia) refractory to other treatments may benefit from long esophageal myotomy.