Betapace
General Information about Betapace
In conclusion, Betapace is a crucial medication for these suffering from irregular heartbeats, significantly sustained ventricular tachycardia and ventricular fibrillation. Its effectiveness in controlling these circumstances and its convenient dosing options make it a preferred alternative for many doctors and sufferers. However, like any medicine, it is important to use Betapace as directed and to watch for any potential unwanted effects. With proper usage and monitoring, Betapace may help people with ventricular arrhythmias live a more healthy and extra comfortable life.
As with any medicine, Betapace also comes with some potential unwanted side effects that sufferers should be aware of. These include dizziness, headache, fatigue, nausea, and diarrhea. While most of these side effects are mild and don't require medical attention, in some uncommon cases, more severe side effects, such as chest ache, problem respiratory, or swelling of the face, can happen. If any of those symptoms are experienced, it's essential to seek medical help instantly.
One of the numerous advantages of Betapace is that it comes in each immediate-release and extended-release formulations, making it handy for patients with completely different needs. The immediate-release formulation is used for speedy treatment and is typically taken two or three times a day, whereas the extended-release option is taken solely once a day, making it extra suitable for long-term use.
Betapace is normally prescribed for a specific sort of ventricular arrhythmia referred to as sustained ventricular tachycardia, the place the guts beats at an abnormally quick tempo for an prolonged interval. It may also be used to deal with a extra severe kind of arrhythmia known as ventricular fibrillation, where the heart beats with chaotic, uncoordinated electrical impulses, inflicting it to quiver as a substitute of pumping blood successfully.
In some instances, Betapace will not be appropriate for individuals with pre-existing coronary heart conditions, liver or kidney illness, or a known allergy to sotalol. Pregnant or breastfeeding girls should also use Betapace with caution and solely underneath medical supervision.
Betapace, additionally known by its generic name, sotalol, is a medication used within the therapy of certain types of irregular heartbeats, medically known as ventricular arrhythmias. These conditions can happen on account of numerous reasons, corresponding to heart illness, certain medications, or electrolyte imbalances. If left untreated, ventricular arrhythmias can be doubtlessly life-threatening, making Betapace a significant medication for those who endure from these situations.
Betapace belongs to a class of medicines generally known as antiarrhythmics, which work by controlling the electrical impulses that trigger the guts to beat irregularly. It does this by blocking particular channels in the coronary heart that are answerable for transmitting these impulses. By doing so, it helps in restoring a normal heart rhythm, thereby lowering the danger of problems.
The dosage of Betapace may range depending on the severity of the condition, the affected person's age, and different underlying health circumstances. It is important to follow the prescribed dosage and to not modify it without consulting a doctor first. A sudden change in dosage can result in critical unwanted effects, together with a sudden rapid heartbeat, dizziness, or fainting.
Betapace can even interact with different medicines, together with blood strain drugs, certain antibiotics, and antidepressants. It is important to tell the doctor about all the medicines and dietary supplements one is presently taking before beginning Betapace to avoid potential interactions.
The nephropathy is of multifactorial origin and may form part of the acute tumour lysis syndrome with accompanying tubular necrosis demi lovato heart attack mp3 cheap betapace 40 mg online. These patients are usually underhydrated, acidotic, and have high rates of uric acid production from nucleoprotein degradation in the apoptotic tumours. Acute uric acid nephropathy has occasionally been reported after extremely severe muscular exercise, after severe epileptic seizures, and in patients with gout due to grossly increased rates of de novo purine synthesis. In addition, the renal pelvis and ureters may also be blocked by crystal aggregates and/or uric acid stones. Acute uric acid nephropathy can be avoided by giving allopurinol for several days before starting the chemotherapy or radiotherapy. Imaging techniques should be used to exclude the presence of bilateral ureteric obstruction by radiotranslucent uric acid stones. Treatment is by: · induction of an alkaline diuresis · haemodialysis, peritoneal dialysis, or haemofiltration · percutaneous nephrostomy and/or ureteric catheterization may be needed if there is an element of postrenal obstruction due to impacted aggregates of sodium urate crystals or uric acid stones · disruption or removal of impacted stones. The standard imaging techniques (particularly ultrasonography) are required for the diagnosis of these radiotranslucent stones. Hereditary renal hypouricaemia and uric acid stones the causes of hypouricaemia are summarized in Box 12. Renal hypouricaemia may be due to renal tubular damage by genetic diseases or by toxic damage (Box 12. Reduced net tubular reabsorption of urate occurs as an isolated renal tubular reabsorption defect due to loss of function mutations in the genes directing the synthesis of the urate carriers. Uric acid urolithiasis occurs in about 25% of the homozygotes, most commonly in patients with combined hyperuricosuria and hypercalciuria. Treatment with allopurinol has, counter-intuitively, been used to prevent the recurrence of renal stones in patients who have experienced acute renal injury after exercise. The rationale is to decrease the generation of uric acid thereby decreasing the filtered uric acid load and lowering the risk of precipitation in the renal tubules. Reduced tubular urate reabsorption can occur in other inherited or acquired renal tubule transport defects (Box 12. The clinical spectrum extends from hyperuricaemia alone to hyperuricaemia with profound neurological and behavioural dysfunction. The biochemistry and molecular genetics of this disorder have been studied extensively. Mutation analysis is a valuable tool for genetic counselling, the identification of carriers, and prenatal diagnosis. The present view is that the neurological manifestations are brought about by a neurotransmitter imbalance, probably mainly in the basal ganglia. This imbalance is possibly due to a deficient supply of metabolic energy resulting from the nonsalvage of hypoxanthine and guanine causing a deficiency of adenine nucleotides that provide energy for short bursts of neurotransmitter synthesis. However, the positron emission tomography evidence of dopamine receptor deficiency is the main concrete evidence for a neurotransmitter defect, either directly or indirectly because of guanosine triphosphate deficiency underlying the LeschNyhan syndrome. There is increased excretion of the serotonin metabolite 5-hydroxyindoleacetic acid and decreased levels of homovanillic acid, a major metabolite of dopamine, in the cerebrospinal fluid. Deficiency of basal ganglia dopamine systems emerging during the first 2 months of life has been demonstrated in a mouse model of LeschNyhan syndrome. With kind permission from Springer Science+Business Media: J Inherit Metab Dis, Lesch-Nyhan syndrome: Growth delay, testicular atrophy and a partial failure of the 11-hydroxylation of steroids, 10, 3, 1987, 210223, R. A similar inability to meet energy requirements may underlie the neurological manifestations. In some cases, the enzyme has altered kinetics or is unstable but has 1 to 5% residual activity. The first clinical sign may be the presence of red grit (uric acid crystals with absorbed urinary pigments) on the nappy. Affected infants are hypotonic from birth, although this is frequently not remarked on before poor head control becomes apparent at the age of about 3 months. Postnatal growth, which becomes more marked after the second year of life, is also subnormal. The overall pattern of weight growth follows centile lines for the first 2 years of life and thereafter slows to about 1 kg/year, or about half normal; a pubertal growth spurt is not observed. The poor weight gain cannot be attributed to either renal failure or malnutrition. Torsion dystonia, with its two components of abnormal posturing and episodic rigidity, is superimposed on the basic hypotonia that is present between the dystonic episodes. Severe dysarthria is associated with dyskinesia of the face, mouth, pharynx, and the larynx, which greatly limits communication and even the ability to point accurately, leading to great frustration. The self-injurious behaviour and dyskinesia are eliminated or much reduced when the child is concentrating on a self-selected activity, such as watching an interesting television programme. Self-injury and dyskinesia are exacerbated by excitement, such as the arrival of a visitor, fear, frustration, and unsuccessful attempts at volitional motor activity. The children also appear to be aware of the value of this behaviour as an attention-seeking manoeuvre, and sometimes appear to use it in a manipulative manner. Although learning difficulties have been stressed as a feature of the LeschNyhan syndrome, they are of inconstant severity and are neither marked nor specific. The apparent degree of intellectual disability may be affected by the extensive disorder of expressive motor functions that exceeds the comprehension defect, by the lack of basic social and educational opportunities, and by the lack of intelligence tests for older children who have lacked these opportunities. However, for whatever combination of reasons, there does appear to be a decline of intellect from the age of 8 to 10 years.
Most endocrine surgery units around the world have at least adopted these vessel-sealing devices and perform part of the operation with them blood pressure of normal person betapace 40 mg buy with visa. If surgery is the only option a repeat vocal cord check is mandatory and all information regarding previous surgery should be obtained. The symptoms range from minor voice change in well-compensated cases, to severe functional effects requiring tracheostomy or cordectomy in cases of bilateral palsy. Minimally invasive and robotic surgery the term minimally invasive thyroid surgery encompasses a host of different techniques, which can be regarded as small incision open surgery, endoscopic surgery and robotic surgery. Various endoscopic approaches have been described, either via a lateral or central neck incision. Evidence suggests that, in the hands of experienced endoscopic endocrine surgeons, their safety outcome is comparable to open surgery, and there may be some cosmetic advantage. However, widespread adoption of these techniques cannot be recommended based on evidence. Permanent hypoparathyroidism is not a trivial complication and patients can be significantly compromised despite supplemental calcium and vitamin D analogues. Identification and preservation of parathyroid tissue and autografting where appropriate will aid in avoidance of this complication. Re-operative surgery is generally avoided in this scenario and antithyroid medical therapy should be employed. As with all surgery, the best policy for preservation of a vital structure is accurate and confident identification. Subtle injuries (without voice changes) may only be picked up during a routine postoperative vocal cord examination. This generally resolves spontaneously over weeks to months in the postoperative period. If nerve transection is recognised at operation and local expertise allows, microsurgical techniques can be employed to either primarily repair the damaged nerve or perform a nerve graft using the ansa cervicalis. Early recognition and aggressive treatment is the best way to avoid the high mortality that is associated with thyroid storm. Decompensation of multiple body systems is common, resulting in tachycardia, arrhythmias, congestive cardiac failure, hypotension, hyperpyrexia, agitation, delirium, psychosis, stupor and coma, nausea and vomiting, diarrhoea, and hepatic failure. Aggressive treatment involves multimodal therapy in conjunction with supportive and cooling therapies in the intensive care setting. The drugs are used to block all pharmacologically accessible steps in thyroid hormone production and function. This is generally a result of trauma during control and division of superior pole vessels, and may be clinically silent. A significant bleed is generally obvious and mandates emergency return to the operating theatre and early intubation by an experienced anaesthetist. When identified on the ward, the patient should be sat upright, oxygen therapy employed and sutures removed to decompress the neck. Steroids may be useful in reducing laryngeal swelling and assist in nerve palsy recovery. Recent series have failed to justify such concern in the modern era of thyroid surgery. However, it is a well-known phenomenon in third world countries with large neglected goitres. The anaesthetist should be informed immediately to ensure that the endotracheal tube cuff has not been damaged and the airway is secure. The motor fibers of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Sensitivity, specificity, and cost-effectiveness of the sensitive thyrotropin assay in the diagnosis of thyroid disease in ambulatory patients. Biomarker-based risk stratification for previously untreated medullary thyroid cancer. Revised in 2009, these guidelines form an important reference for clinicians managing patients with thyroid nodules and differentiated thyroid cancers. Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter Grade B recommendation was made to avoid subtotal thyroidectomy due to significant recurrence rates, inadequately treating incidental thyroid cancers, and providing minimal safety advantage over total thyroidectomy. Ultrasonography for the endocrine surgeon: a valuable clinical tool that enhances diagnostic and therapeutic outcomes. The system aims to clarify thyroid cytopathology terminology to facilitate communication among different specialties involved in managing patients with thyroid diseases. It also allows for reliable sharing of data from different laboratories for national and international collaborative studies. Cystic thyroid nodules after aspiration mimicking malignancy: sonographic characteristics. Increased incidence of thyroid carcinoma in France: a true epidemic or thyroid nodule management effects Major role of genes in the etiology of simple goiter in females: a population-based twin study. Goitre prevalence and thyroid abnormalities at ultrasonography: a comparative epidemiological study in two regions with slightly different iodine status. Natural heterogeneity of thyroid cells: the basis for understanding thyroid function and nodular goiter growth. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Extent of routine central lymph node dissection with small papillary thyroid carcinoma. Central lymph node dissection as a secondary procedure for papillary thyroid cancer: is there added morbidity Poorly differentiated thyroid carcinoma: the Turin proposal for the use of uniform diagnostic criteria and an algorithmic diagnostic approach. Poorly differentiated carcinomas of the thyroid with trabecular, insular, and solid patterns: a clinicopathologic study of 183 patients.
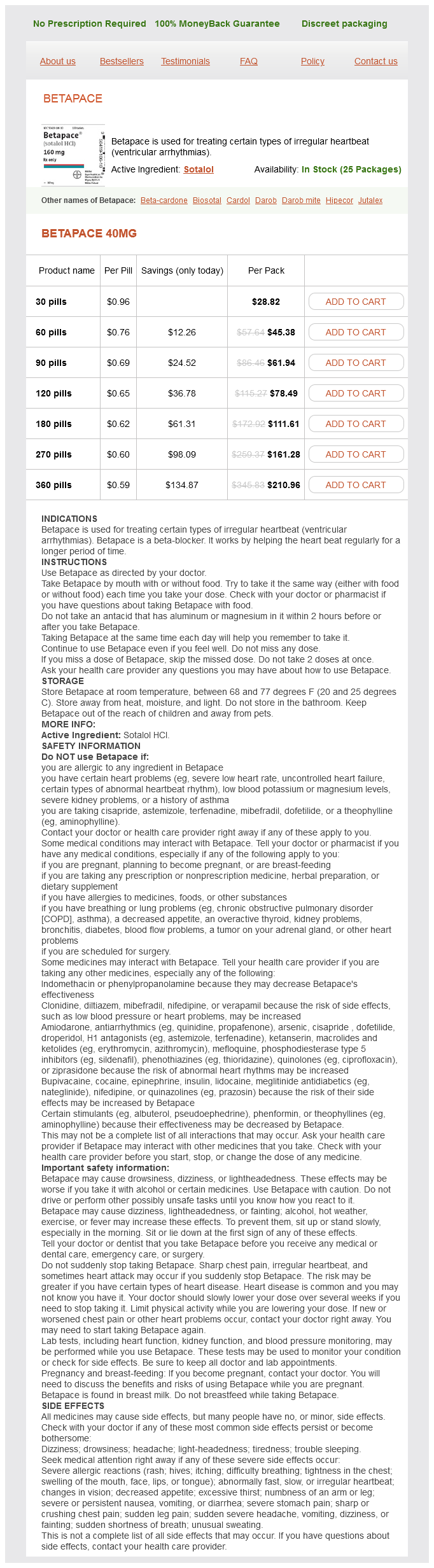
Betapace Dosage and Price
Betapace 40mg
- 30 pills - $28.82
- 60 pills - $45.38
- 90 pills - $61.94
- 120 pills - $78.49
- 180 pills - $111.61
- 270 pills - $161.28
- 360 pills - $210.96
The patient had smaller metastases in contralateral liver but remained free from carcinoid syndrome 4 years after resection of the larger lesion blood pressure medication for ptsd betapace 40 mg mastercard. Prophylactic removal of the mesenterico-intestinal tumour is strongly recommended even in the absence of abdominal symptoms, as this may prevent intestinal complications. Tardy surgical consultation may allow the disease to be increasingly difficult or impossible to manage surgically. It also allows some time for observation and makes surgery or ablation of liver disease safer. Liver surgery consisting of formal hepatic lobectomy or parenchyma-saving liver resections should be undertaken, and this may be combined with wedge resections or simple enucleations of superficially located additional, and even bilateral, lesions. Preoperative portal embolisation may help induce regeneration of a hepatic lobe (without metastases) that is planned to remain after hepatic lobectomy for removal of metastatic tumour. Although methods for visualisation of liver metastases have improved, our experience from operations confirms that many patients have multiple small liver metastases, often not accurately visualised before surgery. As a consequence, liver metastases may be efficiently treated by selective liver artery embolisation. However, tumours larger than 4 cm and tumours close to major vessels may be inefficiently treated (due to heat loss through the perfusing vessels). Complications are reduced in the hands of an experienced interventional radiologist, by prophylactic octreotide infusion during the procedure, and the use of forced diuresis and haemodynamic monitoring during and after the procedure. Special caution is needed in cases where the right hepatic artery originates from the superior mesenteric artery, since mesenteric artery embolism may occur. Patients who have undergone hepatico-jejunostomy or papillotomy are more prone to develop cholangitis or hepatic abscesses afterwards. The results of embolisation are good, although not every patient will respond as expected. Embolisation may be used in cases of multiple unresectable metastases, but it is crucial to carefully consider if the remaining healthy liver parenchyma is sufficient to prevent liver failure in the postembolisation period. Chemoembolisation is arterial embolisation combined with intra-arterial infusion of chemotherapy and may be more effective than embolisation alone, with possibly more pronounced tumour reduction in some cases. Prophylaxis against carcinoid crisis Operation and embolisation in patients with the carcinoid syndrome always entail the risk of inducing a carcinoid crisis, with hyperthermia, shock, arrhythmia, excessive flush or bronchial obstruction. Adrenergic drugs should generally be avoided if hypotension should occur during surgery. Combinations of somatostatin analogue and interferon therapy may increase response rate. Interferon is associated with more adverse effects than somatostatin analogues, mainly flu-like symptoms initially, and later on chronic fatigue and sometimes depression. Autoimmune phenomena may be induced, causing thyroid dysfunction by antithyroid antibodies and occasionally other complications. Side-effects of all analogues include gallstone formation, pancreatic enzyme deficiency and symptoms relating to biliary colic, sometimes necessitating cholecystectomy. Tumours in the base of the appendix require a similar aggressive approach since they may represent colon- rather than appendix-derived tumours. Many may perhaps undergo spontaneous involution, since the prevalence is reported as higher in children than in adults. Treatment for this tumour has mainly included extended ileocolic and mesenteric resection, often performed as re-operation, and additionally chemotherapy. Due to their slow growth rate, palliative tumour debulking may also be undertaken if possible. The increased incidence compared with earlier reports may be due to increased awareness of the diagnosis and use of recently developed diagnostic methods, such as endosonography, as well as more accurate histopathology. These tumours have a higher proliferation rate, commonly regional metastases, and high incidence of liver metastases. However, most patients are asymptomatic and the tumours are found incidentally, which is prognostically beneficial compared with symptomatic presentation. Transrectal endosonography should be used for more precise assessment of tumour extension, possible infiltration in the muscularis propria, and to reveal regional lymph node metastases. Diagnosis is made after histopathological evaluation of biopsies or after removal of the whole nodule. The carcinoid syndrome is extremely rare among these patients and only exceptionally present in cases with liver metastases. Occasional large tumours can be fixed to perirectal tissues and may initially be difficult to distinguish from rectal adenocarcinoma. Previous reports have proposed an increased incidence of concurrent colonic adenocarcinoma. The main sites for tumour spread are regional lymph nodes and the liver, and less commonly lung and bone. Several studies have concluded that there is a correlation between Ki67 expression, tumour size and risk of metastases, although the Ki67 expression generally was low. The immunoreactivity for the different markers is generally unevenly distributed in groups of cells exhibiting focal and patchy distribution. This may indicate development of multiclonal lesions, where additional genetic derangements are prone to occur, causing more aggressive disease in fractions of tumour cells as well as in individual patients. These tumours are frequently associated with distant metastases, local invasion and reduced survival. Our experience of individual patients with large tumours and distant metastases supports this view.