Bupron SR
General Information about Bupron SR
Bupron SR is a member of the aminoketone class of antidepressants. Unlike other antidepressants that primarily work on the neurotransmitters serotonin and norepinephrine, it acts on the brain chemical dopamine. Dopamine is understood to play a major role in regulating mood and motivation, making Bupron SR a useful tool in treating depression.
In conclusion, Bupron SR is a priceless treatment for the treatment of depression and smoking cessation. Its unique mechanism of action and dual benefits make it an attractive choice for people struggling with each situations. If you or a loved one is experiencing symptoms of melancholy or struggling to stop smoking, speak to a healthcare professional to see if Bupron SR could also be an acceptable treatment possibility.
Like any treatment, Bupron SR does have some potential side effects, together with dry mouth, headache, nausea, and insomnia. However, these side effects are normally gentle and have a tendency to improve with continued use. In uncommon cases, Bupron SR may trigger seizures, so you will want to discuss any historical past of seizures with your physician before taking this treatment.
The dual action of Bupron SR makes it a powerful therapy possibility for these suffering from both depression and nicotine habit. By concentrating on each situations, it not only improves temper but also promotes higher total health and quality of life.
Bupron SR is not suitable for everybody and should not be used by individuals with a historical past of an eating disorder or seizures, or those that have taken a monoamine oxidase inhibitor (MAOI) throughout the past 14 days. It is crucial to tell your physician about any medical conditions and medicines you are taking earlier than starting Bupron SR.
Another major benefit of Bupron SR is its effectiveness in aiding smoking cessation. Smoking is a well-known danger issue for a number of health circumstances, including heart disease and lung most cancers. However, quitting smoking is a difficult task, and many individuals struggle to take action on their own. Bupron SR works by reducing the urge to smoke and minimizing withdrawal symptoms, making it easier for people to stop smoking and enhance their general health.
The beneficial dosage for Bupron SR varies depending on the situation being treated. For melancholy, the standard starting dose is 150 mg once day by day, and it could be elevated to a maximum of 300 mg per day. For smoking cessation, the recommended dose is 150 mg as quickly as daily for 3 days, followed by one hundred fifty mg twice every day for seven to 12 weeks. It is important to observe your physician's directions and not exceed the recommended dose.
Depression is a typical mental health dysfunction that impacts millions of people worldwide. It is characterized by persistent emotions of sadness, lack of curiosity in actions, and adjustments in urge for food and sleep patterns. While there are various treatment choices available, many patients wrestle to find reduction from their signs. This is the place Bupron SR is obtainable in.
Bupron SR, additionally identified by its generic name bupropion, is a prescription treatment used to deal with melancholy and assist in smoking cessation. Its unique mechanism of action sets it other than other antidepressants, making it a preferred selection amongst physicians and patients alike.
Consensus guidelines: preconception counseling depression pictures order 150 mg bupron sr with amex, management, and care of the pregnant woman with epilepsy. Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. Stereotactic radiosurgery of the brain using the first United States 201 cobalt-60 source Gamma Knife. The effect of embryonic and fetal exposure to x-ray, microwaves, and ultrasound: counseling the pregnant and nonpregnant patient about these risks. Saving lives and changing family histories: appropriate counseling of pregnant women and men and women of reproductive age, concerning the risk of diagnostic radiation exposures during and before pregnancy. Teratogenic and carcinogenic effects in the offspring after single injection of ethylnitrosourea to pregnant rats. Severe vinblastine-induced leukopenia during late pregnancy with delivery of a normal infant. Normal infant after treatment of acute myeloid leukaemia in pregnancy with daunorubicin. Successful pregnancy and delivery after concomitant temozolomide and radiotherapy treatment of glioblastoma multiforme. Steroid receptor status difference in recurrent intracranial meningioma and breast cancer in the same patient. An analysis of the occurrence of multiple primary neoplasms in meningioma patients in Norway from 1955 through 1986. Presence of progesterone receptors and absence of oestrogen receptors in human intracranial meningioma cytosols. Estrogen and progestin binding by cytosolic and nuclear fractions of human meningiomas. Literature statistics do not support a growth stimulating role for female sex steroid hormones in haemangiomas and meningiomas. Neurological and neurosurgical complications associated with pregnancy and the puerperium. Stereotactic radiosurgery in the treatment of brain metastases: the current evidence. Diagnosis and management of brain metastasis from gestational trophoblastic disease. Blakeley Most brain tumors occur sporadically and without inherited predisposition; however, there are a handful of genetic syndromes that underlie the development of nervous system tumors. These syndromes result from discrete genetic abnormalities and are characterized by well-defined nervous and extra-nervous system manifestations. Most are inherited in an autosomal dominant manner and result from mutations in tumor suppressor genes. In addition, these syndromes provide important models for understanding the critical pathways involved in nervous system tumorigenesis. As such, research into genetic tumor syndromes has supported and will continue to support the development of new targeted therapies for both familial and sporadic tumor conditions. Inheritance is autosomal dominant, although up to 50% of patients may present with de novo mutations and be the first affected family member. However, variable expressivity is observed, meaning that symptoms can vary widely between genotypically similar individuals. As such, tumor development cannot be predicted in any one patient, and the experience of other family members is not predictive. The reasons for this remain unknown but may be influenced by the tumor microenvironment,7 other genes,8 or surrounding cellular haploinsufficiency. Screening neuroimaging is controversial, but generally not pursued unless there are symptoms. Pubertal development and growth should be monitored at least annually for signs of precocious puberty. Intervention should be reserved for those with progressive symptoms or concerning radiographic progression. Chemotherapy remains the backbone of management, with regimens most often including carboplatin with vincristine. These are more likely to be symptomatic with increased intracranial pressure being the most common symptom. Our own small institutional cohort suggests this to be the case even in the setting of radiographic progression. Rapid tumor growth or clinical deterioration should prompt a surgical biopsy to establish tumor grade. When determining treatment for low-grade lesions, radiation therapy should be deferred when feasible. However, highgrade lesions are often treated similarly to sporadic lesions with maximal safe resection, radiation, and chemotherapy. Consensus criteria were first developed at the National Institutes of Health Consensus Conference in 1987 and revised in 1991. Hearing loss, tinnitus, balance difficulty, and rarely vertigo may herald these tumors. In a different patient, a radiographic response of bilateral vestibular schwannomas to bevacizumab, including the baseline lesions (B), with three-dimensional measured volumes of 7. Other nervous system tumors, including cranial nerve, peripheral, and cutaneous schwannomas, are also observed and can become problematic with multiple cranial neuropathies and rarely progressive peripheral neuropathy. After diagnosis, patients should initially be monitored with neuroimaging of suspicious lesions and audiometry at 6-month intervals to establish a trajectory of tumor growth and functional impact.
As discussed in Chapter 127 depression extrovert buy 150 mg bupron sr free shipping, during the course of high-grade glioma, quality of life decreases progressively, which can be significantly exacerbated by the relapses of the disease but also by the administered therapies. Rationale Oligodendroglial tumors have generated high interest as a result of the role of molecular markers in their prognosis and their positive response to systemic chemotherapy in comparison with other high-grade glial tumors. Future Directions Just as carmustine-loaded biodegradable polymers significantly lengthened the survival of patients with recurrent malignant glioma from 23 to 31 weeks after revision resection7 and from 11. Stronger understanding of the biology of these tumors has led to the development of several drugs that work against various disrupted cellular signals in these tumor cells. A very exciting finding in the field of glioma research is the discovery that neural and mesenchymal stem cells have a unique tropism for brain tumor cells. They account for fewer than 2% of all primary brain tumors and have an incidence of fewer than 4 per 1,000,000 people per year in the United States; the incidence is slightly higher in men than in women. However, this may be a result of the longer survival of patients with oligodendroglial tumors. Headaches, mental status change, nausea, vision changes, or weakness can be also present. Another characteristic is the presence of thin branching blood vessels, with a chicken wirelike appearance. Intraoperatively, oligodendrogliomas can have a gelatinous, soft appearance and are pinkish-gray. Calcifications, cysts, necrotic areas, hypervascularity and hemorrhage may also be present. The characteristic molecular marker of oligodendroglial lineage is the 1p19q co-deletion (loss of heterozygosity). This co-deletion not only appears to be strongly associated with oligodendroglial phenotype but also has been demonstrated to be a predictor of longer survival because low- and high-grade oligodendrogliomas are more responsive to treatment. It is postulated that these chromosome regions may contain tumor suppressor genes, which when lost may lead to tumor development, progression, or both. External beam intensitymodulated radiotherapy is usually administered in standard fractions of 1. They are usually peripherally located (cortex or subcortical white matter), diffusely infiltrating with poorly defined margins. In addition, they can manifest calcifications, cystic changes, and intratumoral hemorrhages. Oligodendrogliomas can have discrete heterogeneous enhancement or no enhancement at all. Unlike other malignant gliomas, oligodendrogliomas may be accompanied by mild or no peritumoral edema. Consequently, it is very difficult to differentiate Chemotherapy the recognition that oligodendrogliomas are markedly chemoresponsive has been one of the most significant developments in neuro-oncology. As stated before, in the past, surgery with radiation treatment was the standard of care. A 65-year-old woman presented with tonic-clonic generalized seizures with olfactory auras, signs of hydrocephalus, and left-sided hemiparesis. Unlike other high-grade glial lesions, anaplastic oligodendrogliomas may be accompanied by minimal or no peritumoral edema, as in this case. D, Intraoperative photograph showing the gelatinous consistency and pinkish-gray appearance of this tumor, which also exhibited cysts and necrotic areas. The small enhancing area could correspond to radionecrosis, scarring, or recurrence. G, Positron emission tomographic scan can be used to distinguish recurrence from scar, necrosis, or radiation-related changes. The lack of hypermetabolic activity in the corresponding area helps ruling out actively growing tumor. Current literature suggests that antiangiogenic compounds such as bevacizumab may be also active in recurrent oligodendroglial tumors, but data to support this statement must be stronger. Radiation treatment can be given after surgery and before chemotherapy, or chemotherapy can be given alone, with radiation treatment deferred to tumor progression (preferred alternative). Patients with tumor progression may benefit from further surgery, deferred radiation treatment, "savage" chemotherapy, or a combination of these. However, in view of the striking response of oligodendrogliomas to chemotherapy, this management is under discussion in the scientific community. In the near future, the early use of adjuvant therapies (specially chemotherapy) may be also favored in the treatment of low-grade oligodendrogliomas. In those early studies, oligodendrogliomas were categorized as low- and high-grade gliomas instead of being considered as a separate entity. In addition, current literature contains results from mixed populations of oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas that can be confusing. Overall survival is improved in patients whose tumors have the 1p/19q co-deletion and are treated with the chemotherapy alone group (with deferred radiotherapy to tumor progression). This study may provide some answers to those important questions, but the final results will probably not be available for years. Patient Outcome and Survival the outcome and survival of patients with oligondendrogliomas are favorable in comparison with those of other high-grade glial tumors. Other clinical, surgical, and histopathologic variables have been associated with a prognostic value243 (Table 137-8). The landmark discovery in oligodendrogliomas is that the presence of the 1p/19q co-deletion has been established as a predictor of favorable response to chemotherapy. In contrast, no such benefit was observed for patients with tumors lacking the 1p/19q co-deletion.
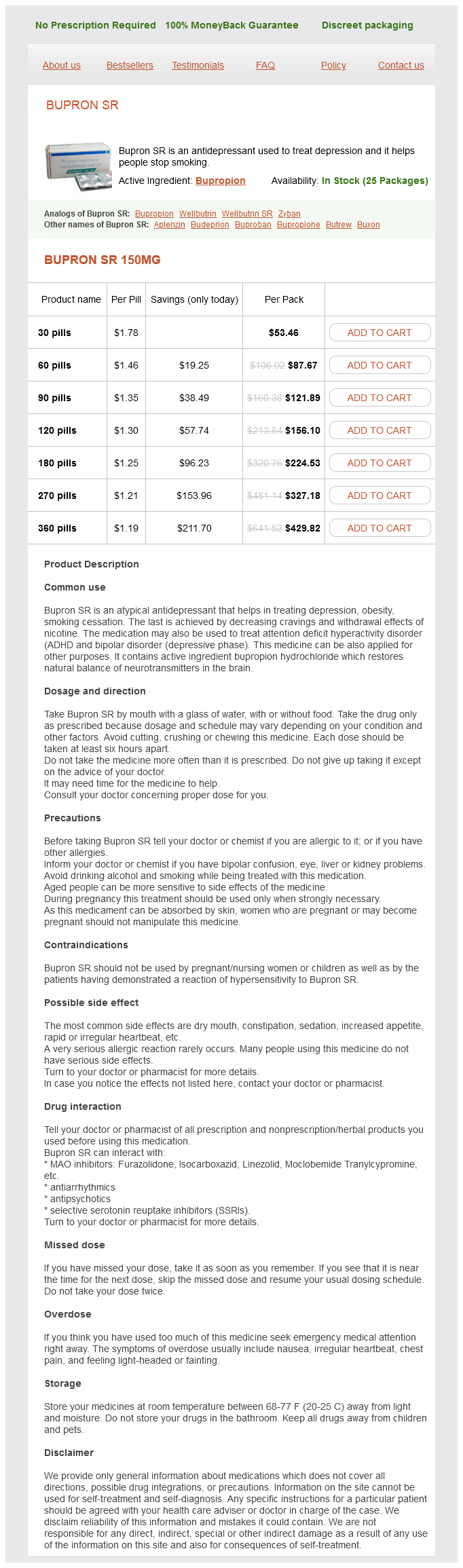
Bupron SR Dosage and Price
Bupron SR 150mg
- 30 pills - $53.46
- 60 pills - $87.67
- 90 pills - $121.89
- 120 pills - $156.10
- 180 pills - $224.53
- 270 pills - $327.18
- 360 pills - $429.82
Because this site is the most commonly proposed origin for these tumors and they are associated with development depression test teens purchase 150 mg bupron sr visa, these plexus remnants may influence the vascularity of the tumor. Accelerated tumor growth was described with testosterone treatment, leading to studies of neoadjuvant flutamide (antiandrogen) treatment. Osteology of the infratemporal fossa and lateral aspect of pterygomaxillary fissure and pterygoid plates with the zygomatic arch removed. Studies using the direction of bony displacement to describe different patterns of growth generally trace the locus of origin to the sphenopalatine foramen, where the posterior part of the middle turbinate attaches. Furthermore the orbit provides an additional route to intracranial extension through the superior orbital fissure. Unilateral nasal obstruction and epistaxis are common early symptoms but often do not prompt diagnosis. Anterior growth invades the posterior aspect of the maxillary sinus and, more superiorly, the ethmoid air cells. With lateral growth the pterygoid plates are eroded, and the tumor extends into the pterygomaxillary fissure. From here it invades the infratemporal fossa and gains access to the inferior orbital fissure, with erosion of the greater wing of sphenoid. The orbit is frequently involved through the inferior orbital fissure as well as through the lamina papyracea from the ethmoid tumor component. When the orbit is involved additional symptoms of diplopia, visual loss, and proptosis may develop. A, Photomicrograph (×50) showing the typical, variably thin-walled blood vessels with variable shapes within a background of fibrocollagenous connective tissue stroma. This is from a deeper region of the lesion, which frequently shows greater stromal cell density than do more superficial regions of nasal angiofibromas. In addition, blood and vessels are more obvious in this particular area because the vessels are congested in this focus. B, Photomicrograph (×200) showing a prominent (at high power) feature typical of nearly all nasal angiofibromas: a generally sparse but rather diffuse inflammatory cell infiltrate composed most prominently (or nearly entirely) of scattered mast cells. Mast cells have a so-called fried-egg appearance, with central round to ovoid nuclei and abundant finely granular basophilic cytoplasm. Axial noncontrast computed tomography scan demonstrating orbital involvement through direct extension with proptosis of the globe. Coronal noncontrast computed tomography scan demonstrating extensive skull base erosion with both intracranial extension and lateral extension to the infratemporal fossa. Coronal T2-weighted magnetic resonance image demonstrating direct extension of the juvenile nasal angiofibroma into the middle cranial fossa, the parasellar region involving the internal carotid artery. Coronal contrast-enhanced T1-weighted magnetic resonance image demonstrating extension of a juvenile nasal angiofibroma into the planum sphenoidale. In published data from India, the rate of intracranial involvement is as high as 90%. First, the tumor may cause direct erosion of the foramen rotundum, ovale, and lacerum. Second, from the infratemporal fossa, tumor can invade directly into the middle cranial fossa. Finally, a particularly vexing intracranial extension occurs through the roof of the sphenoid sinus into the sella and medial to the cavernous sinus. Parasagittal contrast-enhanced T1-weighted magnetic resonance image of juvenile nasal angiofibroma with extension into the orbit and middle cranial fossa. Angiography of internal carotid artery demonstrating tumor blush (arrow) and blood supply from the internal carotid artery branches. Angiograph of extensive juvenile nasal angiofibroma with intracranial component obtained after ophthalmic artery superselective embolization, demonstrating postembolization tumor blush (arrow). Biopsy can be dangerous owing to the vascularity of the tumor and is often not necessary because radiographic studies are fairly specific. Tumors tend to appear isointense to hyperintense on T1- and T2-weighted images and to exhibit avid contrast enhancement. Residual tumor blush after angiographic embolization indicates incomplete vessel occlusion or contralateral vascular supply and may necessitate further angiographic procedures for control. Although embolization is associated with a low rate of complications, anastomoses between the internal maxillary artery and ophthalmic artery can result in loss of vision. However, no randomized controlled trials have been performed to compare surgery with other treatments. In addition, because of the low incidence of disease as well as variations in staging criteria, reporting, and follow-up time, the evidence to support various treatment options is based on systematic reviews, case series, and expert opinion. Techniques for removing earlystage tumors have evolved from open transfacial/transmaxillary approaches and craniofacial resections to more limited open approaches and growing use of endoscopic techniques. As endoscopy has evolved, increasingly complex tumors can be removed through its techniques. However, open and endoscopically assisted open resection are still the approaches of choice for advanced tumors with intracranial extension (Table 160-3). The Radkowski modification of the Sessions staging system, developed in 1996, approximates tumor growth through the various compartments of the skull base with a bias toward open surgery. Recurrence rates tend to relate more closely to tumor stage than to resection method. Open surgery, if performed in the young, carries a theoretically increased risk for damage to the craniofacial growth centers, which could lead to facial asymmetry, malocclusion, or alterations in growth of the middle third of the face. However, when facial incisions are placed correctly at the border of the adjacent facial aesthetic units and closed meticulously, scarring is almost imperceptible. Open surgical techniques can be classified according to the following scheme (see Table 160-3). Surgical approach can be considered according to the location of the incision (anterior versus lateral) and the type of bone work required (creation of a bone flap versus bone removal).