Cafergot
General Information about Cafergot
Cafergot is out there within the type of tablets, suppositories, and injections. The recommended dosage is dependent upon the severity and frequency of the headaches. It is crucial to observe the instructions offered by the doctor or pharmacist fastidiously. Generally, Cafergot ought to be taken on the first signal of a headache to achieve maximum effectiveness.
Like any treatment, Cafergot could trigger some side effects. These include nausea, vomiting, dizziness, and fatigue. Some patients may experience a rise in blood pressure as a end result of vasoconstrictor results of ergotamine. However, these side effects are usually delicate and may be managed by adjusting the dosage or taking the medicine with food.
Cafergot, a medication containing a mixture of caffeine and ergotamine, has been widely used for the remedy of complications since the 1940s. Its effectiveness in relieving migraine and other forms of headaches has made it a popular selection amongst sufferers and healthcare professionals alike.
Cafergot is a prescription medicine used to forestall and deal with vascular headaches, such as migraines. It is a mix of two lively components - caffeine and ergotamine - which work collectively to constrict blood vessels within the brain and reduce inflammation, thus relieving the ache related to headaches.
Cafergot is primarily used for the prevention and remedy of migraine complications. It has additionally been recognized to offer relief for cluster headaches, a rare but extreme kind of headache that happens in clusters over a period of time. The treatment is efficient in lowering the frequency, period, and depth of those headaches. Moreover, it is helpful in relieving other associated symptoms similar to nausea, vomiting, and sensitivity to gentle and sound.
Cafergot has been a trusted medication for the treatment of headaches for a number of years. Its confirmed efficacy and widespread usage make it a preferred alternative among both patients and medical doctors. However, it's essential to make use of this medication as directed and to consult a healthcare skilled earlier than starting any new treatment. With correct utilization, Cafergot can provide relief from headaches and improve the quality of life for individuals affected by these debilitating situations.
Caffeine, a stimulant, helps to extend blood flow within the mind and makes different drugs simpler. In Cafergot, it helps to reinforce the absorption of ergotamine, the main ingredient liable for alleviating complications. Ergotamine is a vasoconstrictor, meaning it narrows blood vessels, thus lowering the pressure on the nerves that trigger the ache associated with headaches.
In case of a missed dose, it's best to take it as quickly as potential. However, if it is close to the time of the following scheduled dose, it is suggested to skip the missed one and continue with the common dosing schedule.
Cafergot can additionally be helpful for individuals who suffer from migraines with aura. Aura refers to visible disturbances, similar to flashing lights or blind spots, which may be typically experienced earlier than a migraine attack. The caffeine in Cafergot might help to ease these symptoms, making it a versatile and reliable possibility for several types of headaches.
It is important to notice that Cafergot should not be used in sufferers with sure medical situations, similar to heart illness, hypertension, liver illness, or kidney illness. It can be not suitable for pregnant or breastfeeding women.
In general pain treatment for plantar fasciitis cafergot 100 mg with amex, this requires the provision of appropriate educational programs and suitable organizational structures. Any unexpected progression of motor block, or the failure of it to resolve, should be considered suspicious and justifies an escalation of clinical care and thorough assessment of the patient. Ideally, low doses of local anesthetic should be used in epidural infusions, so that even if the catheter is placed at a lumbar spinal levels, the likelihood of motor block is low. This scale is widely used and validated, and it is easy to train clinical staff in its use. It does not replace formal neurologic assessment should neurologic deficit be suspected. Suggestive features include systemic pyrexia in association with purulence or cellulitis at the catheter insertion site (128). Delay in decompression of an epidural hematoma or abscess increases the risk of poor recovery of function (132). The use of anticoagulants during epidural infusions needs to be identified and carefully monitored. Guidelines should be established for hospital use to ensure appropriate timing and size of dosing (132). This can provide a consistent response to abnormal or undesirable observations throughout the institution. Professional bodies in a number of countries have issued guidelines for the management of acute pain. However, the benefit or otherwise of any guidelines, whether developed by institutions or professional bodies, will depend on their relevance, effective dissemination and implementation, whether they accurately reflect current knowledge, and degree of compliance. Compliance with guidelines is known to be variable, although it may be better in larger institutions (160) and where staff with pain management expertise and formal quality assurance programs that monitor pain management are available (161). Acute Pain Services Variations in Terminology the term acute pain service is used to cover a variety of different types of service. These can range from those that are a lowcost nursed-based service (162,163) to those that are led by an anesthesiologist but depend on acute pain nurses and are without daily input from an anesthesiologist (164166), through to those that are comprehensive services with acute pain nurses and sometimes other staff such as pharmacists, and which have daily input from and 24-hour cover by anesthesiologists (167 169). However, they also noted that it was not possible to measure the role that other factors. However, regular scheduled input from anesthesiologists and the provision of 24-hour cover may offer additional advantages (170). As well as availability of advice about pain management problems, the anesthesiologist will have expert knowledge about the pharmacology of all analgesic agents, as well as the different delivery techniques available and their risks and benefits. The anesthesiologist will also have a good understanding of the disease processes of the patients they are seeing, and may, if called on, be able to assist with acute postoperative and other medical problems. These must always be done within a cooperative and teambased approach with the primary clinicians caring for the patient. As noted earlier, suboptimal acute pain management may, in some circumstances, result in potential harm to some patients. This information, as well as the data from many surveys published since the 1950s showing that acute pain (both postoperative and in medical wards) was often undertreated, encouraged many of the advances in both acute pain management techniques and drugs made over the last two to three decades. However, these advances have not always led to the anticipated improvements in pain relief. Factors other than just the efficacy of the many techniques and drugs now available for the treatment of acute pain play a part in determining overall patient outcome and include safety (side effects and complications), cost, and any influence on patient outcome, including morbidity and recovery. Efficacy and Outcomes Information about the efficacy of various analgesic drugs and techniques comes from a variety of sources. For example, the close interest shown by investigators could lead to greater nursing attention paid to conventional methods of pain relief, with a consequent improvement in pain relief using these techniques-the "Hawthorn effect" (177). Other findings included significantly greater patient satisfaction, but no difference in length of hospital stay or the incidence of opioid-related side effects (except for an increased incidence of pruritus in the second analysis (29). It is possible that where high nurse-to-patient ratios exist-when it may be possible to give any analgesia truly "on demand"-there is little difference between the techniques. Patient-controlled analgesia had higher incidences of nausea and sedation but was less likely to cause pruritus or urinary retention (64). The device allows delivery of up to six doses each hour, up to a maximum of 80 doses in 24 hours (191,192). It must be replaced every 24 hours, is not yet available in all countries, and is designed for in-hospital use only. Unlike fentanyl patches used for chronic pain management, no reservoir of drug is left in the skin once the device is removed (193). This concern is not unreasonable given that, in any patient, it is known that opioid administration can lead to recurrent episodes of upper airway obstruction when the patient is asleep. However, complications have also been documented in patients given opioids via other routes. Respiratory arrest and the death of three patients receiving postoperative bupivacaine and fentanyl epidural infusions have also been reported (203). The usual sign of respiratory depression described was a decrease in ventilatory frequency. In another report, a patient died after being given intramuscular morphine; during the 2 hours after the injection, he was noted to be "sleeping" and then "unresponsive," and an order was given to continue monitoring of vital signs (204). Epidural Analgesia Because detailed information relating to efficacy and outcomes of epidural is given in Chapter 7, a short summary only of the beneficial effects of epidural analgesia is given in this section. Compared with systemic and epidural opioid analgesia, epidural analgesia with a local anesthetic agent leads to earlier recovery of bowel function after abdominal surgery; the effects are more likely to be seen with thoracic rather than lumbar epidural pain relief (210212). Thoracic epidural analgesia has also been shown to reduce the risk of pneumonia and ventilator days in patients with fractured ribs (213) and reduce the incidence of postoperative myocardial infarction (214).
One-half of the trials reported positive outcomes of epidural steroid injections allied pain treatment center columbus ohio best order for cafergot, and the other half reported negative outcomes. There were significant flaws in the design of most studies included in this analysis, although there appeared to be no relationship between the methodologic quality of the trials and the reported outcomes. A clinically relevant response to treatment was at least 75% improvement or reduction in pain. This review differed from the previous reviews because it was not restricted to epidural steroid injections, and it also considered epidural injections with anesthetics and other injection sites, such as facet joint and local injections. There were Epidural Injection of Steroids: Interlaminar and Transforaminal Approaches Numerous randomized trials have examined the efficacy of epidural injection of steroids for treating acute radicular pain. The rationale behind injecting glucocorticoid into the epidural space is to combat the inflammatory response associated with acute disc herniation (47). There do not appear to be any long-term reductions in pain or disability that stem from long-term epidural steroid use (47,50). Use of this therapy for lumbosacral pain without radicular symptoms has never been proven to be of benefit. The theoretical background supporting the use of epidural steroids is based on the existence of inflammation as the basic pathophysiologic process. Inflammation of nerves in the presence of a herniated disc has further been confirmed during surgery (52), myelography (53), and histologic examinations (54,55). All three systematic reviews are now significantly outdated, and the Cochrane database review performed by Nelemans in 1999 was withdrawn in January 2005, citing the need for an update. It is worth noting that a 80% to 90% probability exists that patients with low back pain will recover within 3 months. The efficacy of epidural corticosteroid injection in the conservative management of sciatica was examined by Buchner et al. Thirtysix patients with lumbar radicular pain due to herniated nucleolus pulposus were randomized to receive epidural steroid injections or no injection. At 2 weeks after injection, those receiving epidural steroid injections had superior improvement in straight-leg raise. There were no differences in pain reduction or functional status at 6 weeks or 6 months after injection. The authors concluded that epidural steroid injections can be recommended only in the acute phase for the conservative management of lumbosciatic pain. All patients had been categorized as potential candidates for surgical nerve root decompression before treatment. A significant reduction of pain occurred early (35 days) in those having an epidural steroid injection, but no difference was noted in the longer-term effects (2-year follow-up). At 3 weeks, those receiving epidural steroids demonstrated a significantly greater reduction in pain, but no difference between groups was seen from 6 to 52 weeks of follow-up. The authors concluded that epidural steroid injections afforded patients earlier relief of pain, but no long-term benefit in pain or need for surgery. When earlier studies are reexamined, a similar early reduction in pain can be seen despite the lack of long-term benefit from epidural steroid injections. Most studies in the literature have used either a mixture of local anesthetics and steroid, saline with steroid, or steroid alone. The steroids most commonly used are either methylprednisolone acetate (DepoMedrol) or triamcinolone diacetate (Aristocort). The doses of methylprednisolone most widely used in the literature vary from 80 mg to 120 mg, and the doses of triamcinolone most commonly used vary from 50 to 75 mg (31,7476). Methylprednisolone acetate has been approved for intramuscular, intrasynovial, soft-tissue, or intralesional injection. It is a glucocorticoid with an elimination half-life of 139 hours, with a range of 58 to 866 hours (77). The transforaminal approach to placing epidural steroids has been advocated as a means of delivering the steroid in high concentration directly to the site of inflammation near the spinal nerve within the lateral epidural space. A recent randomized trial (71) compared the efficacy of transforaminal versus interspinous corticosteroid injection in treating radicular pain in 31 patients. They demonstrated significantly better pain reduction in the transforaminal group at 30-day follow-up. A mailed questionnaire also revealed significantly better pain relief and daily activity levels at 6 months after injection. We are still lacking studies that compare the transforaminal route to the interlaminar route. Two additional recent reviews reinforce the conclusions of earlier publications regarding the use of epidural steroids. The average magnitude of effect is small and generalizability of the observation is limited by the small number of studies, highly selected patient populations, few techniques and doses, and variable comparison treatments; 2) in general, epidural steroid injection for radicular lumbosacral pain does not impact average impairment of function, need for surgery, or provide long-term pain relief beyond 3 months. However, the bulk of the studies do demonstrate more rapid resolution of pain in those receiving epidural steroid injections. Thus, the role for epidural steroid injections in the conservative management of radicular pain is simply to facilitate earlier pain relief and return to full function. It has been approved for administration by intramuscular, intraarticular, or intrasynovial routes (78). No study has compared the effectiveness of triamcinolone and methylprednisolone, and they are probably equally effective. Also, both preparations contain benzyl alcohol, which is potentially toxic when administered locally to neural tissue (83). Most practitioners dilute the steroid with local anesthetic or sterile saline, and the results are apparently comparable with either diluent (84). Some authors have recommended the use of local anesthetics "in the presence of muscle spasms" (85,86). However small the dose, the use of local anesthetic carries some risks, including hypotension, arrhythmias, and seizures from intravascular injections.
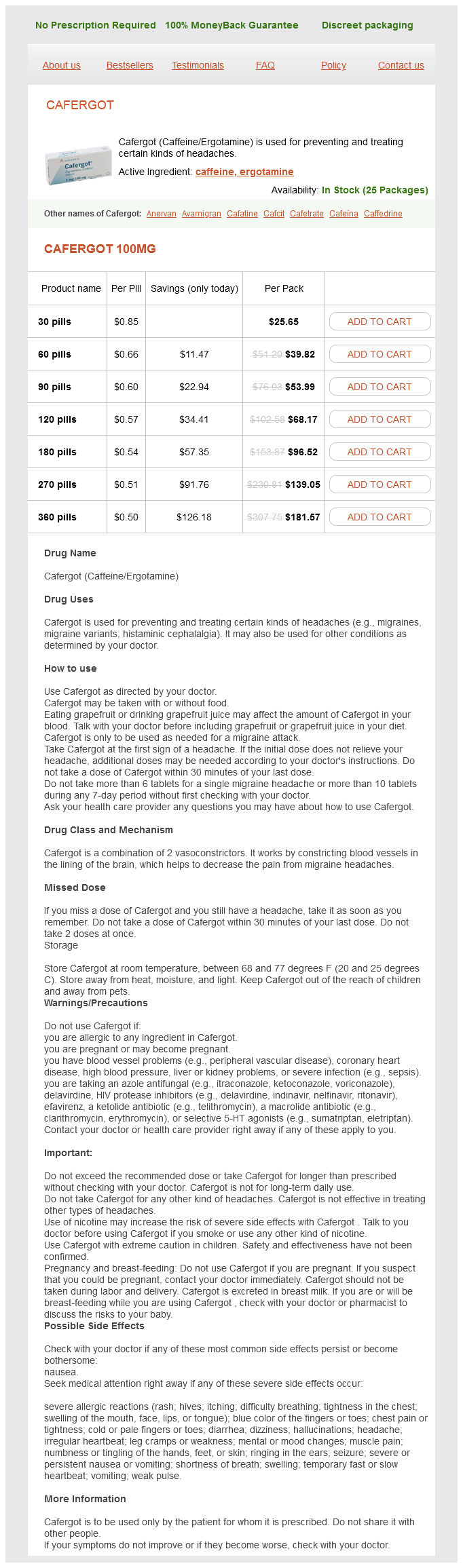
Cafergot Dosage and Price
Cafergot 100mg
- 30 pills - $25.65
- 60 pills - $39.82
- 90 pills - $53.99
- 120 pills - $68.17
- 180 pills - $96.52
- 270 pills - $139.05
- 360 pills - $181.57
The risks factors are not only related to the surgical conditions pain medication for dogs after neuter discount 100 mg cafergot free shipping, but also to preoperative comorbidities. As such, there is some reluctance to use regional anesthesia in emergency surgery, in which the potential benefits of regional anesthesia and analgesia must be balanced against the risks of serious events. Hypovolemia and severe cardiac disorders remain a relative contraindication to the use of neuraxial blockade. Absolute contraindications traditionally include severe bleeding, deranged clotting, and systemic sepsis that could lead to devastating complications if neuraxial blockade is used. However, if appropriate fluid resuscitation, correction of clotting abnormalities, and/or antibiotic prophylaxis are established as soon as the patient is referred to the anesthesiologist, it is possible that neuraxial blockade may be safely performed with the intention that epidural catheter placement would minimize the surgical stress response and attenuate sympathetic hyperactivity. Experimental thoracic epidural block administered to ewes in the presence of hyperdynamic endotoxemia did not cause significant hypotension (93). Local anesthetics should be given in small doses, as they are sufficient to cause extensive neural blockade. Hypotension in response to sympathetic blockade must be corrected aggressively to maintain adequate mesenteric blood Chapter 23: Neural Blockade for Abdominal and Thoracic (Non-vascular) Surgery 529 flow. Hypothermia, another potential consequence of epidural blockade, should be treated by using active warming during surgery to avoid shivering in the immediate postoperative period. Local anesthetics may be beneficial in these circumstances as a result of their anti-inflammatory properties, but, administered in large doses in the presence of sepsis, they can inhibit phagocytosis (94). Fast-track Colonic Surgery and Epidural Anesthesia and Analgesia During the last decade, attempts have been made to apply techniques widely used in ambulatory surgery to major upper and lower abdominal surgery with the intent of accelerating the recovery process. Epidural blockade remains a critical intervention, considered necessary for a rapid recovery program following colonic resection, because of the benefits relating to reduced stress response, effective analgesia, and early restoration of bowel function, early food intake, and early mobilization (9597). However, a number of investigations have shown that, despite the excellent analgesia provided by an effective working epidural, postoperative recovery is not accelerated (80); typically because the pathophysiology of surgical stress is made up of a constellation of components that require attenuation possible only with a multimodal approach. This perioperative program requires optimization of preoperative surgical and medical care, pharmacologic and physiologic attenuation of intraoperative stress response, goal-directed fluid balance, maintenance of normothermia, a minimally invasive surgical approach, optimal analgesia, enforced mobilization, and oral feeding. The benefits of epidural analgesia become most apparent when used as part of a multimodal analgesic regimen. Based on this program, some prospective controlled studies have been able to show an accelerated recovery process with minimal morbidity (98101). Spinal anesthesia with bupivacaine is associated with prolonged recovery and a high incidence of postoperative urinary retention compared with general anesthesia and local infiltration (104). Anorectal Surgery and Regional Anesthesia Anorectal surgery includes hemorrhoidectomy, biopsy, fistulotomy, sphincterotomy, polyp removal, and excision of rectal tumors. To facilitate the surgical approach, patients are positioned either prone, in lateral decubitus, or lithotomy. Minor procedures may be performed under local infiltration; although the injection is extremely painful, it has the advantage of minimal recovery time, good postoperative pain control, and no urinary retention. Caudal blockade provides selective sensory and motor block in the anorectal area, which facilitates ambulation and early discharge. The addition of adjuvants (morphine, fentanyl, epinephrine, clonidine) provides analgesia for 12 to 18 hours for inpatient procedures. Conversely, spinal anesthesia provides a rapid-onset, reliable block with a great success rate. Urinary retention is a recognized complication of both techniques compared with local infiltration and sedation (105). As the safety of general and neuraxial techniques increased, peripheral block was seldom utilized. Outcome studies support the use of neuraxial anesthesia and analgesia to improve pain relief, normalize respiratory function (and reduce respiratory infections), facilitate return of bowel function, and allow early hospital discharge. Recent investigations suggest that plexus (paravertebral) as well as peripheral (intercostal, abdominal wall block, field infiltration) may also be associated with these benefits (see also Chapters 6 and 7). Inguinal Hernia Repair and Regional Anesthesia Hernia repair is a very common operation performed on an ambulatory basis. Different anesthetic techniques are available, including general anesthesia, spinal anesthesia, inguinal field block, and paravertebral block (104). Effects of high thoracic epidural analgesia on myocardial blood flow in patients with ischemic heart disease. Thoracic epidural bupivacaine attenuates supraventricular tachyarrhythmias after pulmonary resection. A prospective randomised study of the potential benefits of thoracic epidural anesthesia and analgesia in patients undergoing coronary artery bypass grafting. Thoracic epidural anesthesia does not improve the incidence of arrhythmia after thoracic esophagectomy. Improvement of diaphragmatic function by a thoracic extradural block after abdominal surgery. Assessment of thoracic epidural analgesia during general anesthesia using pupillary reflex dilation: A preliminary study. Post thoracotomy pain after thoracic epidural analgesia: A prospective follow-up study. Thoracic epidural anesthesia combined with general anesthesia: the preferred anesthetic technique for thoracic surgery. Drug combination in pain treatment: A review of the published evidence and a method for finding the optimal combination. A direct search procedure to optimize of epidural bupivacaine, fentanyl: And for postoperative analgesia combinations clonidine. Analgesia after thoracotomy: Epidural fentanyl/bupivacaine compared with intercostal nerve block plus intravenous morphine. A comparison of thoracic and lumbar epidural techniques for post-thoracoabdominal esophagectomy analgesia. Thoracic versus lumbar administration of epidural morphine for postoperative analgesia after thoracotomy.