Clarinex
General Information about Clarinex
In rare circumstances, Clarinex could cause extreme unwanted effects such as an allergic response, problem respiration, chest pain, and irregular heartbeat. If you experience any of these signs, cease the treatment and seek immediate medical attention.
Why choose Clarinex?
Firstly, Clarinex is a second-generation antihistamine, which means it's newer than the first-generation antihistamines similar to Benadryl. This makes it less likely to trigger drowsiness, a common aspect impact of older antihistamines, and makes it appropriate for use during the day. This is very beneficial for many who need to be alert and productive throughout the day.
Secondly, Clarinex offers reduction for a longer length in comparability with many other antihistamines. It has a protracted half-life, meaning it stays within the body for an extended interval, offering aid for as much as 24 hours with only one daily dose. For those that have busy schedules and cannot afford to take multiple doses throughout the day, Clarinex could be a handy option.
There are many antihistamines available out there, so why should one choose Clarinex? Well, there are a quantity of causes that make this medicine stand out.
Some common unwanted aspect effects of Clarinex embody complications, dry mouth, and fatigue. These side effects are usually gentle and don't require medical attention. However, in the event that they persist or worsen, consult your doctor.
Allergies are a typical condition that affects tens of millions of individuals worldwide. While some might experience gentle signs, others undergo from more extreme reactions that may significantly impression their every day lives. Thankfully, there are many drugs available to alleviate allergy signs, and considered one of them is Clarinex.
Clarinex is on the market as a 5mg pill and ought to be taken orally, with or without meals. The dosage may vary relying on the age and severity of the signs. It is always finest to comply with the directions of your physician or the instructions on the packaging fastidiously. Generally, adults and kids aged 12 years and above can take one pill of Clarinex as soon as a day. For youngsters aged 6 to eleven years, the beneficial dosage is 2.5mg taken once a day. Consult your doctor for the suitable dosage for children underneath 6 years of age.
As with any medicine, there are precautions to be taken whereas using Clarinex. It is essential to inform your physician about any current medical conditions, allergy symptoms, or medications you take earlier than beginning on this medication. Pregnant and breastfeeding girls must also seek the advice of their doctor before taking Clarinex.
Precautions and unwanted effects
What is Clarinex?
How to use Clarinex?
Clarinex, also identified as desloratadine, is an antihistamine medication used to treat the signs of hay fever and other allergies. It is available in pill kind and acts by blocking the consequences of histamine, a substance produced by the physique in response to allergens. Histamine is liable for causing the annoying signs of allergic reactions, corresponding to sneezing, itching, and a runny nose. By blocking the action of histamine, Clarinex helps to relieve these symptoms and supply relief for those suffering from allergies.
In conclusion, Clarinex is a protected and effective choice for treating allergy symptoms. With its long-lasting relief, minimal unwanted aspect effects, and versatility in treating various signs, it has become a preferred alternative amongst sufferers. However, it is all the time advisable to consult a well being care provider earlier than beginning any new medication to make sure its safety and effectiveness in your particular condition. With Clarinex, you presumably can bid goodbye to those pesky allergy signs and enjoy a better high quality of life.
Another advantage of Clarinex is its effectiveness in treating a extensive range of signs. It effectively relieves the common signs of allergic reactions, such as sneezing, itching, watery eyes, and a runny nose. It is also beneficial for the remedy of hives and pores and skin itching brought on by allergies. The versatility of this medicine makes it a go-to choice for so much of sufferers.
Sézary syndrome is a systemic variant of mycosis fungoides characterized by erythroderma allergy unc 5 mg clarinex sale, generalized lymph node enlargement, and the presence of circulating 533 neoplastic cells. As in mycosis fungoides, the skin shows dermal and epidermal infiltration with cerebriform lymphocytes. The peripheral blood film has numerous small or large neoplastic cells with cerebriform nuclei containing condensed chromatin. Because these cells may appear in small numbers in both benign skin diseases and early stages of mycosis fungoides, most criteria require that their level exceed 1,000/mm3. Peripheral T-Cell Lymphoma, Unspecified this category includes about 50% of the peripheral T-cell lymphomas in Western countries. Most cases occur in adults, and the disease usually presents with nodal involvement, but disseminated disease is common, often with circulating neoplastic cells and affected extranodal sites, especially the skin. These lymphomas cause diffuse infiltration of lymph nodes with neoplastic cells that are variable, but most commonly medium- to large-sized cells with irregular, pleomorphic nuclei and prominent nucleoli. Vascular proliferation in the lymph node is common, and often a mixed inflammatory reaction is prominent, including eosinophils, plasma cells, small lymphocytes, and epithelioid histiocytes. Multinucleated cells resembling ReedSternberg cells and "clear cells" with very pale cytoplasm may be present. Nodal Peripheral T-Cell Lymphoma with T-Follicular Helper Phenotype Patients with this disorder tend to present with constitutional symptoms, rashes, polyclonal hypergammaglobulinemia, immunosuppression, and generalized lymphadenopathy. It generally occurs in older adults and has an aggressive course because of the associated immunodeficiency. Lymph nodes show prominent arborizing vasculature with expansion of the interfollicular areas by atypical T cells with clear cytoplasm (so-called "clear-cell immunoblasts"). These cells induce proliferation of follicular dendritic cells and recruit B cells to the lymph node. An IgH gene rearrangement can be seen in 30% of cases, in addition to T-cell receptor gene rearrangement, which is present in over 90%. The usual clinical features are generalized lymph node enlargement and constitutional symptoms, including fever. The disease is commonly widespread at the time of diagnosis, typically involving such extranodal sites as skin, bone, lung, and liver. The neoplastic cells are pleomorphic, but despite this lymphoma having three variants-common, lymphohistiocytic, and small-cell-all cases include some characteristic cells called "hallmark cells" because they are present in all types. These have eccentric nuclei shaped like horseshoes or kidneys, sometimes with a perinuclear eosinophilic area. In the common variant, which accounts for about 70% of cases, large hallmark cells typically predominate, and they possess abundant cytoplasm that is clear, 534 basophilic, or eosinophilic. Multiple nuclei may occur, the chromatin usually is dispersed, and nucleoli are prominent. Sometimes, the hallmark cells are less numerous than the large neoplastic cells with rounded nuclei. Neoplastic cells are rarely visible in the peripheral blood film, where they are large and pleomorphic. Bone marrow biopsies may show the large, pleomorphic, and sometimes multinucleated lymphoma cells in an interstitial, focal, or diffuse pattern. Hodgkin lymphomas are defined by the presence of diagnostic tumor cells, known as ReedSternberg cells, in the appropriate cellular environment. In classical Hodgkin lymphoma, the ReedSternberg cells are single or multinucleated cells with prominent central nucleoli. Even with marrow involvement, they are also uncommon in the bone marrow aspirate, where they appear as large cells with two nuclei and prominent nucleoli. On bone marrow biopsy, neoplastic cells are present in about 10% of cases and usually exist in a mixture of small lymphocytes, 535 eosinophils, and macrophages. Variations include the presence of numerous ReedSternberg cells with few other cells, a fibrotic marrow with few neoplastic cells, and a hypocellular marrow with scattered foci of neoplastic and reactive cells. Nodular Lymphocyte Predominant Hodgkin Lymphoma this group accounts for 5% of Hodgkin lymphoma and typically occurs in the fourth to sixth decade of life. It usually causes localized lymph node enlargement in cervical, axillary, and inguinal lymph nodes. The histology is characterized by a nodular infiltrate of small lymphocytes and histiocytes with scattered large atypical cells called L&H cells ("lymphocytic and/or histiocytic ReedSternberg cells"). There may be morphologic overlap between cases of nodular lymphocytepredominant Hodgkin lymphoma and T-cell/histiocyte-rich forms of large B-cell lymphoma; a broad panel of immunohistochemical stains is necessary to resolve this differential. The disease has a fairly indolent course with a good prognosis despite frequent relapses. Classical Hodgkin Lymphoma this group accounts for 95% of cases of Hodgkin lymphoma and has a bimodal age distribution with a peak between 20 and 30 years and a smaller peak in the elderly. Most patients present with localized lymph node enlargement affecting cervical, mediastinal, axillary, or para-aortic regions. Primary extranodal involvement is rare, as is bone marrow infiltration, except in advanced disease or severely immunodeficient individuals. All subtypes of classical Hodgkin lymphoma will have variably numerous ReedSternberg cells with the identical immunophenotype (described above). Nodular Sclerosis Hodgkin Lymphoma this type accounts for about 70% of classical Hodgkin lymphoma, with a median age of 28 and equal gender distribution. Lymph nodes have a thickened capsule with broad bands of fibrosis dividing the lymphoid tissue into nodules composed of a polymorphous cell population, with small lymphocytes, plasma cells, eosinophils, and macrophages admixed with less numerous ReedSternberg cells.
It should begin with a binary statement of positive or negative allergy symptoms duration 5 mg clarinex with visa, followed by statements citing which cell populations were analyzed. If positive, the percentage of total cells should be cited along with the most salient immunophenotypic properties. Although specimens are sometimes received for the evaluation of other immune abnormalities, any interpretation of the results should be performed with great caution. The rosette test is still the most widely used screening test in the United States. Still, flow cytometry can be useful in confirming that a myeloid population is neoplastic when diagnostic features are not known or are pending evaluation. What follows is a concise description of flow cytometry for clinically relevant purposes in myeloid neoplasms. Aside from subtle abnormalities like abnormally dim or abnormally bright expression of expected antigens, detection of aberrant antigen expression is useful and important. Again, dim/partial expression is not significant, but uniform expression by a distinct, discrete myeloid population is typically indicative of a neoplasm. Diagnostic criteria for myeloid neoplasms in which the neoplastic cells are mature. The use of flow cytometry in such diseases is limited to the assessment of blasts in the event that a blast crisis has been diagnosed by clinical and morphologic findings. Also, cases with "abnormal maturation patterns" in which diagnostic criteria are not met are not found to have an increased future risk for development of a myeloid neoplasm. Also important is the general lack of lymphoid antigen expression (although some lymphoid antigens may be aberrantly expressed by neoplastic blasts). Acute biphenotypic leukemia is rare, and coexpression of markers for all three lineages is extremely rare. In cases in which surface antigen evaluation is ambiguous for lineage, cytoplasmic antigen evaluation frequently is helpful. Because no well-defined immunophenotype exists in mixed phenotype acute leukemia, these cases must be evaluated on a case-by-case basis. Finally, both mixed phenotype acute leukemia and acute bilineal leukemia should be distinguished from undifferentiated acute leukemia. These neoplasms are defined by lymphoblast morphology and confirmed by immunophenotype. Whereas a population of some sIg+ and some sIg+ reactive B cells is called polytypic, a neoplastic population with only sIg+ or sIg+ is called "monotypic. For example, an sIgk+ lymphoma may exist in a specimen with a relatively large number of nonneoplastic B cells; because the background B cells have a normal:, the overall ratio may be skewed only slightly or not at all, depending on the size of the neoplastic population. In such cases, permeabilizing the cells and assessing cytoplasmic immunoglobulin light chain expression often shows clear monotypic expression. Whereas the process of B-cell ontogenic maturation is limited to peripheral lymphoid organs, T-cell populations are highly plastic at all sites. Also, temporary "abnormal" T-cell populations commonly arise during immune reactions and can be seen in numerous clinical scenarios in patients with different kinds of illnesses. Because any clinically relevant neoplasm is an abnormal growth, diagnosis of a neoplasm must be based upon demonstration of an expanded population. Although it involves skin and marrow, because it is typically leukemic, a blood sample usually is submitted for diagnosis. Because most patients are asymptomatic, a definitive diagnosis is not usually required. The diagnosis of lymphoma is typically easy to make on the basis of a large population of circulating and/or infiltrative, markedly atypical lymphoid cells. For these reasons, bone marrow core biopsy immunostaining is the best and most accurate technique for analysis of myeloma (see below). Because "junk" and dead cells typically fall on that line, in general, populations of cells in that location would be assumed to be "background," not representing true expression. An important concept that should be emphasized is that, consequent to the action of therapeutic drugs, often, the immunophenotype of the cancer cells changes after therapy. In others, there are subtle changes, like a decrease or increase in the level of expression of an antigen. In some cases, the changes are relatively dramatic, prompting reversion to genetic analysis, to prove the relationship to the prior cancer. The methods described are proprietary, requiring specific, nonstandard processing machinery, reagents, and cytometers; as such, the published methods for circulating tumor cell detection cannot be performed in a 90 standard laboratory. After the collection, the photographed events are visually examined by a technologist, who decides whether the "positive event" is actually a tumor cell. Moreover, its use seems to be waning and there are questions about the efficacy of the information. The advantages are cost savings due to the use of far less reagents and labor savings due to not having to maintain the flow cytometry apparatus. The downside is that, because the aliquots in the wells are so small, the number of cells analyzed is far less. Still, for most specimens, laser scanning cytometry works well for diagnostic purposes. The reasons for such limited use are not known, but may be due to resistance to change platforms and/or to a lack of effective marketing from laser scanning cytometry manufacturers. Although some practitioners are adept at analysis of maturation patterns for diagnostic purposes and have supported its use since the late 1990s, this technique has never found widespread acceptance for diagnostic purposes or been included in any well accepted scheme for diagnostic criteria. Unlike solid organs, in which most of the cells in a biopsy are tumor cells, in hematopoietic lesions, the cells of interest are admixed with large populations of background cells. For most purposes, a skilled practitioner can find a population of interest on one slide, then look at another slide and discern whether the second antigen is expressed by the population of interest, by inference from the spatial location in the tissue.
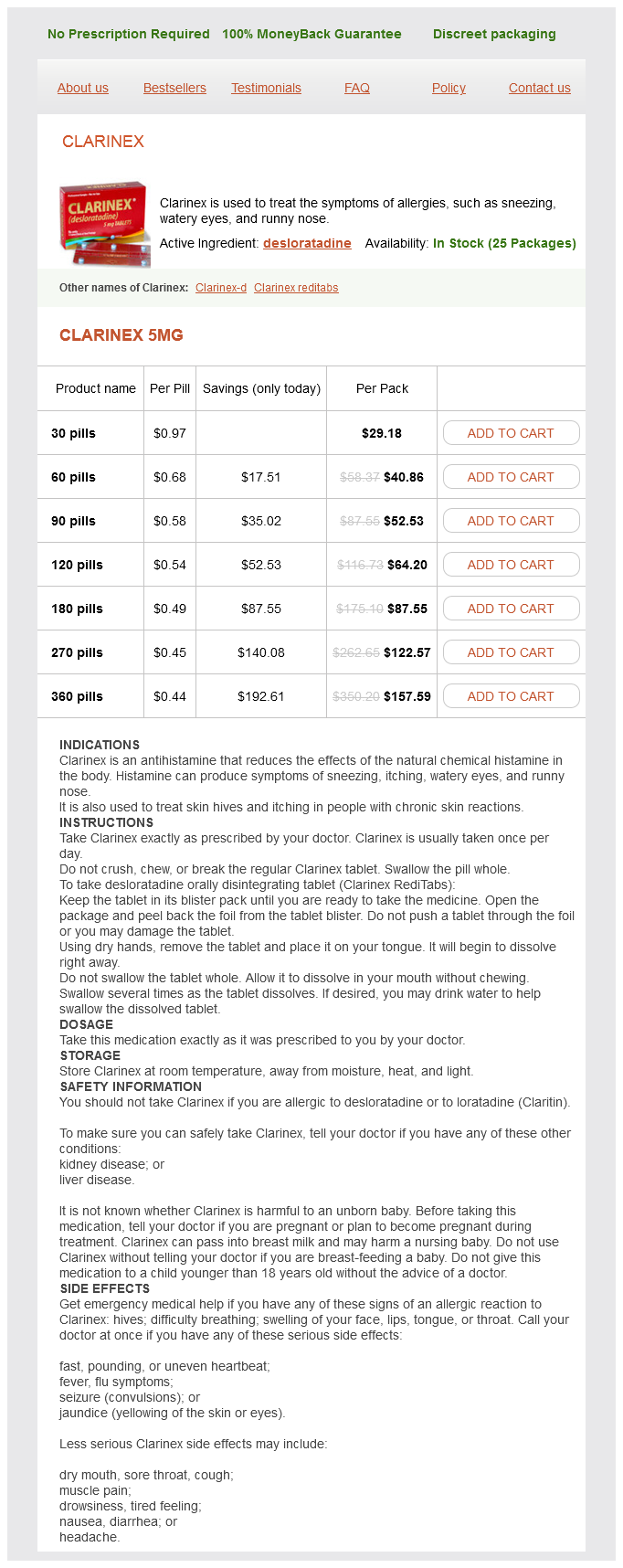
Clarinex Dosage and Price
Clarinex 5mg
- 30 pills - $29.18
- 60 pills - $40.86
- 90 pills - $52.53
- 120 pills - $64.20
- 180 pills - $87.55
- 270 pills - $122.57
- 360 pills - $157.59
Occasionally allergy medicine you can take when pregnant clarinex 5 mg buy otc, endometrial implants are seen on the cervix or vaginal walls during speculum examination, appearing as nonblanching red or brownish/blackish areas or firm nodules. Asymptomatic lesions do not require treatment, although biopsy for histology is appropriate if the diagnosis is unclear. There are no specific laboratory tests for endometriosis (Signorile & Baldi, 2015). Women with irregular, heavy, or irregular bleeding may warrant endometrial biopsy and testing for anemia. Transvaginal ultrasound is a relatively low-cost technology that can play a role in ruling out other diagnoses and that may identify endometriomas, adenomyosis, and, occasionally, deeply infiltrating endometriosis in the bladder, uterosacral ligaments, rectum, or rectovaginal septum. Transrectal ultrasound may identify bowel involvement and aid in surgical planning (Kodaman, 2015). Endometriosis and adenomyosis are really diagnoses of histology and require surgical biopsy for confirmation. Differential Diagnoses Other gynecologic and nongynecologic causes of chronic pelvic pain include bladder pain syndromes, irritable bowel syndrome, pelvic-floor muscle myalgias, and other gynecologic anatomic abnormalities. Management Women experiencing symptoms of endometriosis variants generally can choose among expectant management, medical therapies, and surgery. Considerations relating to fertility are discussed in the "Special Populations" subsection. Goals of medical management include both symptom management and maintenance of desired fertility. Ovulation suppression is a primary target of medical therapy, with the goal being to eliminate or reduce ectopic endometrial activity. There is insufficient evidence to compare the pain relief effectiveness of specific agents or specific regimens, either as initial treatment or for postsurgical maintenance. Benign Gynecologic Conditions 647 treatments may recur when the medical therapy is discontinued. Additional medications directed at pain control, including neurotransmitter modulators and opioids, are used for chronic pelvic pain associated with endometriosis. While surgery is required for definitive diagnosis of endometriosis, this modality is now reserved for treatment for women with debilitating symptoms and poor response or intolerance to medical therapy. Laparoscopic removal of implants and adhesions is effective for pain management and resolution of symptomatic endometriomas, although removal may decrease ovarian reserve (Brown & Farquhar, 2014). In addition, moderate-quality evidence supports a role for laparoscopic interventional surgery in increasing pregnancy and live birth rates for women with endometriosis and infertility. Following conservative surgery, medical suppression is often restarted, as pelvic pain symptoms may recur in as many as 40% of women (Kodaman, 2015). Repeat procedures increase risks of postoperative adhesions and damage to ovarian reserve. Endometriomas larger than 4 cm are typically removed, even if asymptomatic, as they have been associated with ovarian cancers (Kodaman, 2015). Women who have severe pain, but wish to preserve their fertility and have not responded to other treatments, may consider a presacral neurectomy (excision of the portion of the superior hypogastric plexus that provides sympathetic innervation to the uterus) (Kodaman, 2015). This complex procedure is done infrequently, but provides better long-term pain control when compared to laparoscopic procedures alone. The definitive surgery for endometriosis is hysterectomy with salpingo-oophorectomy. Women may be most likely to choose hysterectomy if they do not desire a future pregnancy and have resistant symptoms that are severely impacting their quality of life. They should know that pain persists after definitive surgery in as many as 15% of women, and may increase again over time in as many as 5% more (Kodaman, 2015). Women who elect ovarian preservation have the benefit of bone preservation and positive cardiovascular effects, but increase their risk of persistent or recurrent symptoms sixfold (Kodaman, 2015). In contrast, use of add-back estrogen post oophorectomy appears to have minimal effects on the risk of persistent or recurrent symptoms. For isolated adenomyosis, women may choose to undergo complete hysterectomy with ovarian preservation. Other potential agents under investigation for endometriosis management include statins, given that blocking cholesterol biosynthesis may inhibit bioconversion activity in implants; immunomodulators, to modify immune surveillance for ectopic cells; angiogenesis inhibitors, to limit implant proliferation; synthetic steroids, which are used in other countries to treat endometriosis, but are currently banned in the United States due to their risk of abuse as performance-enhancing drugs; and valproic acid, which appears to reverse silencing of apoptotic genes that effect endometriosis (Quass, Weedin, & Hansen, 2015). Nonpharmaceutical agents under investigation include the 648 Chapter 26: Benign Gynecologic Conditions antioxidant hormone melatonin; certain isoflavones. Results for these modalities remain preliminary, however, and the preparations are nonstandardized, so they may contain varying amounts of active ingredients (Quass et al. Pregnant Women Although the etiology is unclear, women with either endometriosis or adenomyosis have increased risks when they do achieve pregnancy, including late miscarriage, preterm birth, fetal growth restriction, and antepartum hemorrhage (Brosens et al. These outcomes may be related to progesterone resistance and/or the increased risk of subclinical atherosclerosis, a condition that is also associated with endometriosis. Older Women In postmenopausal women, emerging evidence suggests that while symptom resolution is typical, endometriosis-related problems may sometimes persist (Brosens et al. For example, women with endometriosisassociated infertility may have early-onset menopause; as many as 4% of women, especially obese women, continue to have active symptoms after menopause, even in the absence of hormone therapy; use of hormone therapy or tamoxifen has been implicated in symptom recurrence after menopause for some women; and there is a low (less than 1%) but increased risk of malignant transformation of endometrial implants, especially on the ovaries (Brosens et al. Special Populations Adolescents Endometriosis should be considered in the differential diagnosis of even premenarcheal girls with chronic pelvic pain, as cases of biopsyconfirmed symptomatic implants have been reported (Brosens et al. Also, endometriosis is more common in girls with imperforate hymen or other obstructive Müllerian anomalies.