Cleocin Gel
General Information about Cleocin Gel
One of the advantages of Cleocin Gel is that it can be applied directly to the affected areas, making it a convenient and focused remedy. It can be well-tolerated by most people, and side effects are typically gentle and transient. The most typical unwanted facet effects embody pores and skin irritation, dryness, peeling, and itching. In uncommon cases, it could cause more extreme side effects, such as allergic reactions or the event of a serious intestinal infection called Clostridioides difficile-associated diarrhea (CDAD). It is essential to debate any potential dangers with your healthcare supplier before starting treatment.
Cleocin Gel has been shown to be an efficient treatment for severe pimples when used as directed. Studies have found that it may possibly significantly scale back the variety of inflammatory lesions and improve general zits severity. It has also been discovered to be secure and effective for long-term use in adults and adolescents.
Cleocin Gel is usually utilized to the affected areas of the pores and skin twice day by day, in the morning and night, after washing the skin with a gentle cleanser. It is important to comply with your healthcare provider's directions fastidiously and to proceed using the medication for the total prescribed length. It could take a quantity of weeks before you see noticeable improvement, so endurance is key. It can be recommended to avoid utilizing different topical merchandise, such as harsh cleansers, astringents, or merchandise containing benzoyl peroxide, whereas utilizing Cleocin Gel.
Cleocin Gel, also known as Clindamycin Phosphate Topical Gel, is a prescription medication used for the therapy of severe zits. It is an antibiotic that works by killing micro organism that can cause zits. Cleocin Gel is a topical medicine, that means it's utilized directly to the skin, and it's out there in the type of a gel or lotion.
Overall, Cleocin Gel is a reliable choice for those battling extreme pimples. It supplies a focused and convenient approach to deal with acne, and has been proven to be efficient in reducing breakouts and bettering the looks of the pores and skin. If you might be coping with cussed acne that is not responding to different therapies, speak to your healthcare supplier about whether Cleocin Gel may be an appropriate possibility for you.
The lively ingredient in Cleocin Gel, clindamycin phosphate, is an antibiotic that belongs to the lincosamide class. It works by inhibiting the growth of bacteria, such as Propionibacterium acnes, a common bacteria discovered on the skin that can contribute to the development of zits. By decreasing the number of micro organism on the skin, Cleocin Gel helps to decrease irritation and the frequency of breakouts.
Severe zits can be a irritating and embarrassing condition. It is characterised by pink, inflamed, and sometimes painful pimples and nodules on the face, neck, chest, and back. These lesions can even depart behind unpleasant scars. While there are numerous over-the-counter remedies obtainable for zits, Cleocin Gel is commonly prescribed for more extreme cases that do not reply to other medications.
Factor analysis identified five common factors, thus emphasizing the utility of assessing common dimensions of experimental and clinical pain acne between eyebrows purchase cleocin gel once a day. Another experiment by Klepac and co-workers (1981) assessed high or low levels of either cold pressor pain or electrical tooth pulp pain in a 2 × 2 factorial design. Overall intensity scores differentiated the two types of stimulation, which also resulted in qualitatively different responses. In summary, validated methods have been developed to assess one, two, and more dimensions of the pain experience. Naliboff (Gracely & Naliboff 1996) identified four criteria for increasing the number of dimensions: A multidimensional system may increase utility if it: (1) leads to an increase in accuracy of pain reports. If, for example, the amount of prickliness of a pain is a clear marker of certain types of tissue pathology then assessment of only sensory and affective intensity (painfulness) may yield poorer diagnostic discrimination. Similarly, pain ratings with very unusual patterns of multidimensional ratings might indicate malingering or confusion. There are also instances in which such measures are necessary, such as assessment of pain in animals and infants or in adults with poorly developed language skills. Although arguments have been made for the exclusive use of non-verbal methods, these procedures can also be influenced by extraneous factors. They use similarity to verbal report to establish concurrent validity, thus suggesting that verbal measures are preferable if available. Generally, arguments for the superiority of one method over another often reflect the tendency of research laboratories to specialize in a single method. The resulting differences have sparked lively debate, identified important measurement flaws, and generally improved the technology of pain assessment. There is a growing consensus that in most situations, effective pain assessment may ultimately result from an approach that integrates information from these separate, complementary sources of information. However, as discussed further, the considerable plasticity in pain processing and the many examples of disassociation between non-verbal measures and subjective reports indicate that ultimately, pain can be defined only by a verbal description of the perceptual experience. Behavioral Measures It is well known that pain elicits stereotypical behavior in both humans and animals. Grimacing, vocalization, licking, limping, and rubbing are often elicited by a painful stimulus. Both these naturally occurring reactions and trained operant behavior (such as manipulating a bar to escape a painful stimulus) have been used to assess the magnitude of stimulusevoked pain sensation. Many have been used more extensively for the assessment of clinical pain syndromes (Keefe and Dolan 1986, McDaniel et al 1986). Exceptions include studies of facial expression evoked by experimental stimulation (Patrick et al 1986) or analysis of pain expressions from photographs (LeResche 1982). Early studies focused on autonomic measures such as heart rate and skin conductance but found that these responses habituated quickly and were non-specific because they were evoked by painful, non-painful, or novel stimulation. Autonomic measures continue to be assessed, but the bulk of such studies examine physiological measures related to neural processing. Progressing from the periphery to the brain, these methods examine microneurographical recordings of primary afferent activity, spinal reflexes, evoked and ongoing cortical activity, recording and stimulation of the thalamus and brain during neurosurgical procedures, and functional brain imaging. Microneurography Neurophysiological recording of afferent activity in animals has provided a wealth of information about the function of nociceptors. Human microneurography uses recording methods tested in animal research to investigate peripheral mechanisms in unanesthetized normal volunteers. The pioneering experiments (Vallbo and Hagbarth 1968) recorded from myelinated A fibers and, subsequently, from unmyelinated C-fiber afferents (Torebjork and Hallin 1970). Human microneurography is a powerful tool that can compare intervening primary afferent activity in response to both the evoking stimulus and the resulting sensation. This method has characterized several functional classes of C fibers, including polymodal nociceptors that are sensitive to heat, mechanical, and chemical stimulation. A marking method has been used to identify another class of mechano-insensitive C fibers that probably mediate blunt pressure pain and, when inflamed, respond to mechanical punctate stimulation (Namer and Handwerker 2009, Schmelz and Schmidt 2010). The mechanically insensitive C fibers have been shown to be involved in aspects of central sensitization, for example, in mediating spontaneous pain following injections of capsaicin and the resultant mechanical hyperalgesia (Schmelz et al 2000). Microneurography has identified neural signatures for itch and compared flare responses in human, pig, monkey, and rat subjects and activity in the terminal arborization of C-fiber nociceptors (Weidner et al 2003, Namer and Handwerker 2009, Schmelz and Schmidt 2010). This method remains a valuable conduit to the functioning of pain primary afferents in both health and disease. These reflexes are commonly elicited by a train of electrical pulses (typically five 1-msec pulses at 200300 Hz) and, rarely, by laser stimulation (Andersen et al 2006) and mechanical stimulation, such as ballistic impacts (Beise et al 1999). Basic studies have assessed nociceptive specificity (Kaube et al 2000, de Tommaso et al 2001, Romaniello et al 2002), optimized parameters (Katsarava et al 2002), and determined the spatial organization of reflexes as a function of intensity and locus of stimulation (Andersen et al 2001). These studies have provided information about the neural organization of the nociceptive system, including the convergence of occipital and trigeminal cutaneous afferents. In addition, the amplitude of evoked reflexes has been shown to correlate with other physiological parameters such as cerebral evoked potentials or the concentration of administered analgesics and anesthetics or circulating opioids (Skljarevski and Ramadan 2002). Nociceptive reflexes share the temporal resolution that is a feature of the following methods in this section. This resolution has been used to investigate mechanisms mediating pain and pain modulation. Edwards and colleagues (2002) took advantage of the precise timing characteristics of cutaneous electrical stimulation to deliver stimuli to the sural nerve during different phases of the cardiac cycle. Using either the amplitude of the nociceptive reflex produced by specific stimulus intensities or the amount of current needed to evoke the reflex, these authors found reduced sensitivity during the systolic pressure pulse consistent with an arterial baroreceptor mechanism of hypertensive hypoalgesia. Several studies have also demonstrated modulation of lower limb or jaw muscle reflexes by deep muscle pain evoked by the infusion of hypertonic saline (Andersen et al 2000), by intramuscular electrical stimulation (Andersen et al 2006), by brief heat (Andersen et al 1998), and by simple limb movement (Don et al 2008). These studies indicate that inhibition of reflexes is not a unitary, homogeneous effect but varies depending on at least the type and location of the conditioning tonic stimulation.
These central changes do not occur or are significantly attenuated in subdiaphragmatically vagotomized animals into which illness-inducing agents have been injected intraperitoneally (for discussion see Sawchenko et al 1996; Dantzer et al 2000, 2007) skin care zits quality 20 gm cleocin gel. The pain and hyperalgesia that occur following activation of the innate immune system by intraperitoneal injection of lipopolysaccharide are suggested to be produced by activity in the subdiaphragmatic vagal afferents, specifically those running in the hepatic branch. These results suggest that vagal afferents, probably those innervating the liver, are activated by pro-inflammatory cytokines released by activated macrophages (Kupffer cells), dendritic cells, and leukocytes. The pro-inflammatory cytokines either activate the vagal afferents directly or bind specifically to glomus cells in the abdominal paraganglia that are innervated by vagal afferents. Activation of vagal afferents in this way leads to activation of neurons in the nucleus tractus solitarii and subsequently activation of noradrenergic neurons in the A1 and A2 areas of the brain stem that project to the hypothalamus. Stimulation of somatic tissues by lipopolysaccharide with resultant local release of inflammatory cytokines also generates a febrile response, which is a component of the protective sickness behavior. This response is also, at least in part, mediated by spinal or trigeminal primary afferent neurons. The functional nature of these afferent neurons is unknown (Romeo et al 2001, Navarro et al 2006). Watkins, Maier, and co-workers developed the general thesis that vagal abdominal afferents projecting through the hepatic branch of the abdominal vagus nerve form an Cytokines and Inflammatory Pain: A Peripheral Mechanism Studies of mechanical and heat hyperalgesic behavior in rats have shown that tissue injury, injection of the bacterial cell wall endotoxin lipopolysaccharide, or injection of the plant polysaccharide carrageenan generates tissue inflammation and sensitization of nociceptors. Pathogenic stimuli activate resident cells, which release the inflammatory mediator bradykinin (an octapeptide cleaved from plasma 2-globulins by kallikreins circulating in plasma) and other mediators. The two peripheral pathways, involving cytokines, by which nociceptive afferents can be sensitized are under the inhibitory control of circulating glucocorticoids (indicated by asterisks in. Proof of such interaction between nociceptive afferents, inflammatory cytokines, and sympathetic (noradrenergic) terminals is still lacking and requires direct recording of the activity of nociceptors via electrophysiological techniques. Role of pro-inflammatory cytokines in generating pain and hyperalgesia by activation and sensitization of afferent nociceptive neurons during tissue inflammation or trauma with nerve injury. Some steps in this scheme are hypothetical and need to be verified experimentally in neurophysiological experiments (see discussion by Watkins and Maier 2002; Watkins et al 2007a, 2007b). The underlying mechanisms are related to morphological, biochemical, and physiological changes in the primary afferent and central neurons. One important peripheral component in the generation of neuropathic pain after nerve trauma is peripheral inflammation involving immune and immune-like cells. Nerve trauma is followed by invasion of hematogenous macrophages and activation of Schwann cells and fibroblasts. The pro-inflammatory cytokines released intraneurally are believed to be an important component in the generation of ectopic impulses in lesioned afferent nerve fibers and therefore in the generation of neuropathic pain. The underlying mechanisms by which the interleukins contribute to the generation of ectopic impulses in nociceptive afferent neurons remain an important area for research (Watkins and Maier 2000, 2002; Scholz and Woolf 2007; Austin and Moalem-Taylor 2010). These changes in peripheral afferent neurons are followed by complex changes in the spinal cord and in supraspinal centers. The role of pro-inflammatory cytokines released by glia (microglia and astrocytes) in the spinal cord and activated by pathogens (bacteria and viruses), by transmitter released by nociceptive afferents, or by other substances released by neurons. The cellular and molecular mechanisms underlying the development and maintenance of allodynia and hyperalgesia are time dependent and different (Watkins and Maier 2000, 2002; Scholz and Woolf 2007; Watkins et al 2007a, 2007b; Milligan and Watkins 2009; Austin and Moalem-Taylor 2010). The parameters of the immune tissues potentially controlled include proliferation, circulation, and trafficking of lymphocytes; functional activity of lymphoid cells. The mechanisms of this influence remain largely unsolved (Ader and Cohen 1993, Besedovsky and del Rey 1995). In view of the functional specificity of the sympathetic pathways (Jänig 2006, Jänig and McLachlan 2012), a key unanswered question is whether the immune system is supplied by a sympathetic pathway that is separate from other functionally distinct sympathetic pathways (such as vasoconstrictor pathways to resistance vessels or cutaneous blood vessels, and secretomotor pathways to sweat glands or other glands). Several observations support the idea of a distinct sympathetic channel of communication from the brain to the immune system that is under control of the hypothalamus: First, primary and secondary lymphoid tissues are innervated by postganglionic noradrenergic sympathetic neurons. Varicosities of the sympathetic terminals can be found in close proximity to T lymphocytes and macrophages (see Madden et al 204 Section One Neurobiology of Pain Stimulus (pathogenic challenge) Resident cells Bradykinin, other Third, experimental studies performed on the spleen of rodents involving surgical or chemical sympathectomy, stimulation of the splenic nerve, recording from the splenic nerve, and lesioning or stimulation of distinct hypothalamic sites argue that a hypothalamicsympathetic neural system may specifically control the immune system (Katafuchi et al 1993, Hori et al 1995, Okamoto et al 1996). However, in certain pathological conditions this system may also be involved in the generation of pain. These conditions have been defined by quantitative investigations conducted on patients with pain depending on the sympathetic nervous system. On the basis of these quantitative data, hypotheses have been developed to experimentally test the mechanisms underlying the role of the (efferent) sympathetic nervous system in the generation of pain. The behavioral and reduced (in vivo and in vitro) animal models for studying sympatheticsensory coupling have been discussed critically (Jänig 2009a). Sympathetically maintained pain includes ongoing pain and pain evoked by mechanical and cold stimulation. It may be present in complex regional pain syndrome types 1 and 2 and in other neuropathic pain syndromes (Stanton-Hicks et al 1995). The idea that the efferent sympathetic nervous system is involved in pain is based on a long history of clinical observations that have been documented in the literature (White and Sweet 1969, Bonica 1990, Harden et al 2001). Representative of these multiple observations on patients with sympathetically maintained pain are quantitative experimental investigations (Torebjörk et al 1995, Price et al 1998, Ali et al 2000, Baron et al 2002). These investigations demonstrate the following: · Physiological activation of sympathetic neurons. The interpretation of these data is that nociceptors are excited and possibly sensitized by noradrenaline released by sympathetic fibers. Noradrenaline acts on the adrenoceptors of nociceptors and/or the excitatory effect is generated indirectly, for example, through changes in tissue blood flow. Role of cytokines in sensitization of nociceptors during inflammation and the underlying putative mechanisms leading to hyperalgesia. Pathogenic stimuli activate resident cells and lead to the release of inflammatory mediators (such as bradykinin). Pro-inflammatory cytokines are synthesized and released by macrophages and other immune or immune-related cells.
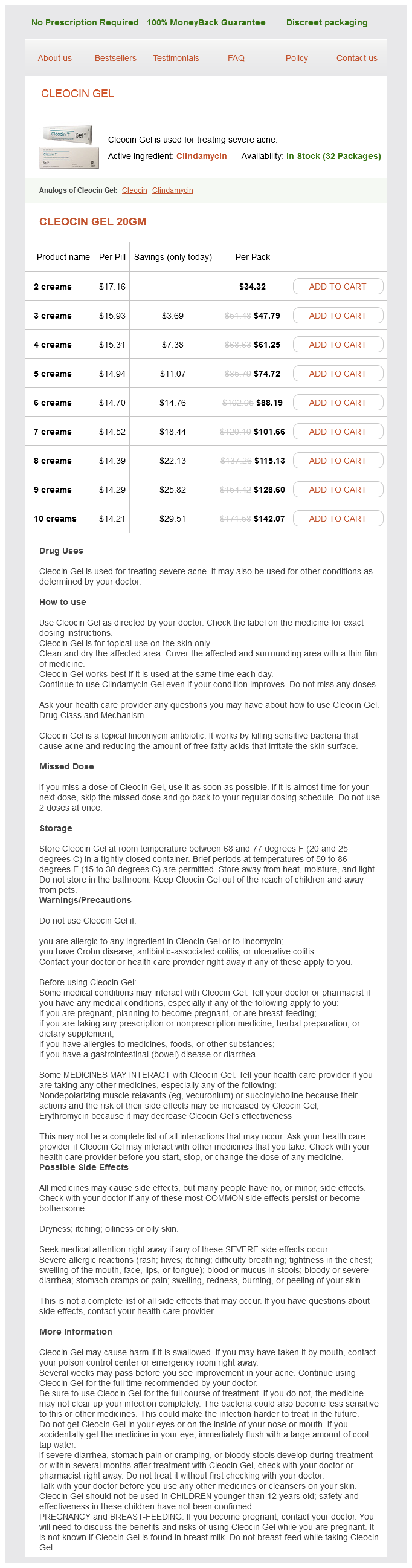
Cleocin Gel Dosage and Price
Cleocin Gel 20gm
- 2 creams - $34.32
- 3 creams - $47.79
- 4 creams - $61.25
- 5 creams - $74.72
- 6 creams - $88.19
- 7 creams - $101.66
- 8 creams - $115.13
- 9 creams - $128.60
- 10 creams - $142.07
Overall, these strategies may have some benefit in managing acute pain but appear to provide little benefit in managing chronic pain (Boothby et al 1999) acne quiz cleocin gel 20 gm order online. Task Persistence the extent to which people continue their usual daily activities as a strategy to manage pain has been labeled task persistence (Jensen et al 1995). Task persistence is one of the few pain-coping strategies that has fairly consistently been associated with positive outcomes, including disability and depression (Jensen et al 1995, Tan et al 2005, Garcia-Campayo et al 2007, Jensen et al 2011), and it is one of the more frequently endorsed pain-coping strategies (Ersek et al 2006). Recent developments in using electronic devices to quantify activity level may prove useful in both research and clinical settings, either to monitor (Bussman et al 1998) or increase physical activity (Talbot et al 2003) or to track increases associated with treatment of pain (Agarwal et al 2007). In some instances, measurement of actual physical function has been performed in the clinical office (Harding et al 1994), and the use of similar measures in epidemiological studies (Fried et al 2001) suggests that such measures may be feasible for monitoring physical capabilities in clinical settings. However, widespread use of these direct measurements continues to be hampered largely by issues of feasibility. For these reasons, all the widely used measures of function involve self-report by the patient. The specificity of this latter approach is a clear advantage of these scales but not appropriate for other painful conditions that do not affect that particular activity in most patients. The measures included here were chosen because of their use in many different painful conditions but may not be appropriate when a disease-specific measure is available, commonly used, or recommended by consensus panels. Coping Self-Statements Some studies have found positive self-statements to be associated with adaptive functioning. As with other pain-coping strategies, the positive impact of coping self-statements is not consistent across studies and outcome domains. Reviews conclude that positive coping self-statements do not generally show a consistent relationship with reduced pain and improved functioning (Boothby et al 1999, DeGood and Cook 2011). However, these coping self-statements are an integral component of most psychological interventions for pain management and show change with treatment. Spirituality and Religiosity Prayer is one the most frequently endorsed pain-coping strategies, and although spiritual and religious beliefs contribute to many positive types of coping behavior, these beliefs can also direct negative coping behavior (Pargament et al 2000, Wachholtz and Pearce 2009). Higher scores on this scale are generally correlated with greater pain severity, disability, and distress (Andersson 2008), although the results are inconsistent (Boothby et al 1999). The correlational nature of this research does not illuminate whether people pray and hope more in response to difficult times or whether this coping strategy contributes actively to poorer adaptation to chronic pain (Boothby et al 1999). Patients with rheumatoid arthritis have reported large day-to-day variation in the frequency and nature of daily religious/spiritual coping, and some dimensions of religious/spiritual pain coping were associated with higher positive and lower negative mood (Keefe et al 2001). Research on acceptance of chronic pain suggests that spirituality may be a key dimension of accepting pain when the spiritual dimension is presented as positive and guiding (Risdon et al 2003). Interest in the health benefits of spirituality/ religiosity (Hill and Pargament 2003) and the frequent use of spiritual/religious coping strategies for managing pain suggest that continued, expanded investigation of this domain might be informative in future studies. For this to be fruitful, new scales will have to be developed or adapted from other areas of investigation (Pargament et al 2000). Pain-Related Function Pain-related function is one of the most important outcomes in the pain literature, second only to pain severity, with which it is highly correlated. Pain-related function typically includes ratings by patients of the extent to which pain causes disability or interferes with activities. Most measures of pain-related function assess multiple domains of function, including daily activities, work, socializing, and recreation, and many include ratings of the impact of pain on mood and in most instances include ratings of the impact of pain on sleep. Thus, many of these measures confound the assessment of physical and psychosocial function. Widespread use of this scale, which has been translated into numerous languages, has yielded an extensive literature on the psychosocial aspects of pain. The scale includes 12 subscales, many of which measure psychosocial function, including social support, negative mood, life control, specific responses from the significant other (solicitous, distracting, or punishing responses to pain), and activity level. Some of the earliest assessments of physical activity and function relied on diaries of "uptime," or the amount of time patients spend sitting, standing, or walking (Fordyce et al 1973). The perceived interference scale is embedded in the first section of the instrument and includes 11 items that assess interference or change in satisfaction in day-to-day activities, sleep, work, social and recreational activities, marriage and family activities, household chores, and friendships (Rudy 1989). The instructions do not include any specific time frame, and most items do not specify a time frame. This scale is typically used as a summary of four activity scales in which social activities, activities away from home, household chores, and outdoor work are assessed with 18 items. Validation of these two subscales is provided by an extensive literature from multiple countries and many different types of pain conditions documenting expected relationships with other measures of interference, activity level, disability, and function. Improvements in treadmill capacity and reductions in downtime correlated with increases in general activity in patients with musculoskeletal pain enrolled in a multidisciplinary rehabilitation program (Burns et al 1998). These scales have been used extensively to measure outcomes of multidisciplinary rehabilitation, psychological treatments of chronic pain, and even a brief (1. However, not all studies show the expected changes when using these scales (Nielson et al 1992). Randomized, controlled clinical trials have used these scales extensively to document improvements following psychological and rehabilitative treatments in a number of chronic pain populations. It has been translated into many different languages and its use extended to a wide range of chronically painful conditions (Dworkin et al 2005). Some investigators have added additional domains: self-care, recreational activities, and social activities (Jensen et al 2002). Pain Behavior Pain behavior-the actions that communicate pain-has long been assessed clinically, and now a systematic, empirical literature has amassed from a variety of systematic methodologies developed for observing and coding overt pain behavior (Labus et al 2003).