Crestor
General Information about Crestor
Crestor works by inhibiting the enzyme HMG-CoA reductase, which is responsible for the production of ldl cholesterol in the liver. By reducing the manufacturing of ldl cholesterol, this medication helps decrease the whole cholesterol levels within the body. It additionally increases the levels of high-density lipoprotein (HDL), often identified as 'good' ldl cholesterol, and decreases the degrees of low-density lipoprotein (LDL), known as 'bad' cholesterol, and triglycerides.
Crestor is proven to be efficient in lowering levels of cholesterol and stopping the development of atherosclerosis. Clinical trials have proven that it could lower LDL levels of cholesterol by up to 60%, while increasing HDL cholesterol by 15%. It has also been shown to scale back the risk of coronary heart attacks, strokes, and different cardiovascular events in sufferers with excessive levels of cholesterol.
Crestor, also known by its generic name rosuvastatin, is a prescription drug used to lower cholesterol levels within the blood. It was first approved by the Food and Drug Administration (FDA) within the United States in 2003 and is manufactured by AstraZeneca. It is now available in lots of international locations and is among the mostly prescribed statins.
In conclusion, Crestor is a extensively used and effective treatment for the remedy of high cholesterol and atherosclerosis. It is necessary to observe the prescribed dosage and inform the physician of any potential side effects. Along with medicine, a nutritious diet and regular train are additionally essential in controlling cholesterol levels and reducing the danger of heart disease.
However, like any other medication, Crestor additionally has its potential unwanted effects. The commonest side effects embody headache, muscle pain, nausea, and weakness. In rare circumstances, Crestor could cause a serious situation referred to as rhabdomyolysis, where breakdown of muscle tissue can lead to kidney failure. It is important to consult a physician instantly if any symptoms of this condition, corresponding to muscle pain, tenderness, or weak point, are skilled while taking Crestor.
High ldl cholesterol and atherosclerosis are two of the most typical health situations that tens of millions of people face worldwide. Both these circumstances are intently associated as high cholesterol levels can result in the development and development of atherosclerosis, a situation where the build-up of fatty deposits, also identified as plaque, occurs within the partitions of the arteries. This build-up can finally lead to blockages and enhance the risk of heart attack and stroke. To combat these circumstances, doctors often prescribe statins, a category of medication that help lower levels of cholesterol. One such drug in this class is Crestor.
Crestor may interact with certain drugs, so it is essential to inform the physician of all of the medications which are presently being taken, including over-the-counter medication and supplements.
The beneficial beginning dose of Crestor is 10-20 mg as quickly as daily, with or with out meals. The dosage could additionally be increased to a maximum of 40 mg per day if essential. Crestor is available in tablet type in different strengths, together with 5 mg, 10 mg, 20 mg, and forty mg. For patients who've issue swallowing tablets, the medication may be crushed and combined with a spoonful of applesauce or yogurt.
Because vaginal neoplasia is unoommon cholesterol jfk ratio discount crestor express, most management strategies are derived from small, retrospective, and statistically unde. Management ofValN is inlluenc:ed by bistologic diagnosis; neoplasia grade; and lesion siu:, number, and location. Each treatment method has advantages and disadvantages and none has proven superior efficacy. Thus, observation is preferable in most cases, and aggressive treat· mcnt is avoided. Observation Preinvasive Lesions of the Lower Anogenital Tract 643 be spread on the vulva for protection. It carries a significant risk ofserious morbidity and is reserved for select ca&e&. In a review of 136 cases of vaginal carcinoma in situ, radiation therapy was used in 27 patients, and a lO~percent cure rate was noted. However, 63 percent developed significant complications that included vaginal steno. Furthermore, radiation treatment compromises subsequent cytologic, colpoacopic, and histologi. For treatment of recurrent high-grade ValN, a lower diswas associated with C02 laser ablation compared with medical treatment (Bogani, 2019). Patients with any grade of vaginal neoplasia require long-term monitoring, because the persistence and recurrence. Monitoring includes collection of vaginal cytology and performance of vaginoscopy approximately 2 to 4 months after tteatment is completed. Continued surveillance with periodic cytology with or without vaginoscopy at 6- to 12-month. The keratlnlzlng, stratified squamous epithelium is characterized by cells that have increasing cytoplasm as they mature from base to surface. Cells In all eplthellal layers are disordered and have nuclear pleomorphlsm, chromatin abnormalities, and a variably greater nudeus-to-cytoplasm ratio. This particular example has a papillomatous surface, a common finding in these lesions. In this classic example, the squamous epithelium appears relatively mature but has notable cytologic atypia (nuclear pleomorphism, prominent nucleoli) involving the basal and suprabasal cell layers. Abnormal keratinocyte differentiation is evidenced by dyskeratosis and individual cell keratinization. However, one study identifying trends in the incidence of vulvar carcinoma in situ found a fourfold rise from 1973 to 2000. Instead, they tend to arise in a background of inflammatory dermatosis, particularly lichen sclerosus. If clinical findings warrant, review by an experienced gynecologic pathologist may be helpful (van den Einden, 2013). They may be white, hyperkeratotic plaques; hyperpigmented lesions; or erythematous areas. As an alternative, 1-percent toluidine blue, a nuclear stain, may hdp define lesions Qoura, 1998). However, because its use is technically more challenging and results are fraught with. The most abnormal-appearing areas are biopsied, although necrotic areas often yidd nond. Topical anesthetics can be applied several minutes prior to injeaion of local anesthesia to decrease discomfort. Iflesions are close to the clitoral hood, general anesthesia is often warranted due to greater pain with injection of local anesthesia and increased tis. Careful documentation, mapping of vulvar biopsy si~, and photographs can aid future management. Selection of the best location to biopsy is aided by magnification of the vulva, perineum, and perianal skin, usually with a colposcope. Vulvar epithelial changes are enhanced by applying a 3to 5-percent acetio-acid-soaked gauze pad to the vulva for 5 minutes prior to vulvoscopy. Because vulvar epithelium is keratini2:ed, application of acetic acid to achieve a useful visible effect requires longer time to develop. This is usually well tolerated but may cause pain or burning if comorbid vulvar irritation, ulceration, or fissures are present. Acetic acid accentuates surface topography and may reveal acetowhite lesions not seen grossly. This distance affects disease management, particularly if ablative procedures are considered. Regardless of the modality selected, treatment side effects are common and can include vulvar discomfort, poor wound healing, infection, and scarring that may result in chronic pain or dyspareunia. Thus, treatment objectives include: (1) excluding and preventing invasive disease, (2) preserving vulvar appearance and function, and (3) improving patient symptoms. Because disease recurrence is related to surgical margin status, intraoperative frozen-section histologic analysis of the specimen margins is advantageous (Friedrich, 1980; Jones, 2005). Hopkins and colleagues (2001) reported disease recurrence rates of 20 percent for cases with negative surgical margins but 40 percent for those with positive margins. Moreover, due to disease location, some patients are best treated by combined excisional and ablative procedures. As C02 laser ablation does not allow evaluation of a surgical specimen, invasive carcinoma must be excluded by adequate biopsy beforehand. Ultrasound is used to cause cavitation and disruption of affected tissue, which is then aspirated and collected (Section 43-29, p.
Both pre- and postmenopawal women treated with tamoxifen for breast cancer have a higher risk for benign ovarian cygt formation (Chalas cholesterol test kit cvs crestor 20 mg purchase fast delivery, 2005; Simpk:im 2005). Premenopausal women and women with greater body mass index are disparatdy a1fected. If clinical signs of malignancy are present, surgical exploration is indicated, and tamoxifen is discontinued. Several epidemiologic studies have linked smoking with functional cyst devdopment (Holt, 2005; Wyshak, 1988). Although the exact mechanism(s) is unknown, changes in gonadotropin secretion and ovarian function are suspected (Michnovia, 1986). Surgical excision may be reasonable for large persistent cysts, usually those > 10 cm, or for smaller ones producing persistently bothersome symptoms. With a corpus luteum, transvaginal sonography and applied color Doppler typically display a brightly colored ring because of enhanced vascularity surrounding the cyst. Bilateral, multiple smooth-walled cysts form and range in size from 1 to 4 cm in diameter. These cysu typically resolve spontaneously following removal of the stimulating hormone source. Diffuse low-level echoes, which are commonly associated with recent hemorrhage, are seen throughout this smooth·walled cyst B. In categorizing tumors within the epithelial family, benign turners are designated as adenomas; malignant tumors, as carcinomar, and those with exuberant cellular proliferation without invasive behavior as low malignant potential (Chen, 2003). Thus, serous cystatlmofibroma describes a benign, mainly cystic tumor of the ovarian epithelial tumor group in which stromal components predominate (Prat, 2009). T eratomas arise from a single germ cell, and therefore may contain any of the three germ layers-ectoderm, mesoderm, or endoderm. T eratomas are classified as: Immature teratoma-This neoplasm is malignant and described in Chapter 36 (p. Immature tissues from one, two, or all three germ cell layers are found and often coexist with mature dements. Mature teratoma-This benign tumor contains mature forms of the three germ cell layers: 1. Mature cystic teratoma develops into a cyst, is common, and may also he called benign cystic teratoma or dmnoid cyst. Fetiform teratoma or homunculus forms a doll-shape, as the germ cell layers display considerable normal spatial differentiation. Monodermal teratoma-This benign tumor is composed either solely or predominantly of only one highly specialized tissue type. Of the monodermal teratomas, those composed dominantly of thyroid tissue are termed struma ovarii. These benign tumors constitute approximately 10 to 25 percent of all ovarian neoplasms and 60 percent of all benign ovarian neoplasms (Koonings, 1989; Peterson, 1955). These cystic tumors are typically slow growing, and most measure between 5 and 10 cm (Comerci, 1994). When sectioned, most cysts appear unilocular and typically contain one area of localized growth, which protrudes into the cystic cavity. Ovarian neoplasms can be distinguished histologically depending on their cell type of origin. These are grouped as epithelial tumors, germ cell tumors, sex cordstromal tumors, and others shown in Table 10-3. Ofbenign ovarian neoplasms, serous and mucinous cystadenomas and mature cystic teratoma are the most common (Pantoja, 1975). Microscopically, endodermal or mesodermal derivatives may be found, but ecrodermal elements usually predominate. The cyst is typically lined with keratinized squamous epithelium and contains abundant sebaceous and sweat glands. The Rokitansky protuberance is usually the site where the most varied tissue types are found and is a common location · Benign Serous and Mucinous Tumors these are members of the surface epithelial neoplasia group, and both are lined by cells similar to those lining the fallopian tube. This simple cyst has a fibrous wall and is lined by a single layer of benign, columnar tubal-type eplthellum with cilia. Muclnous cystadenomas are typlcally multlloculated cysts llned by a single layer of benign mucln-contalnlng eplthellum. Muclnous fluid ls secreted by the eplthellum and contained within the cystic mass. In this image, it is the amorphous material above the epithelium and is stained pink (asterisk). In this classic histologic example, ectodermal elements include skin (Sk), sebaceous (Se), and eccrine (E) glands, whereas mesodermal elements are smooth muscle (Sm) and adipose A). This transformation occurs in <2 percent of mature cystic teratomas (Black, 2015; Comerci, 1994). Patients older than 50 years or with mas4es > 10 cm are at greater risk (Chiang, 2017; Park. The diverse tis4ues found within teratomas do not arise by fertilization of an ovum by spenn. Instead, they are thought to devdop from genetic material contained within a single oocyte by asexual parthtntJgmesis.
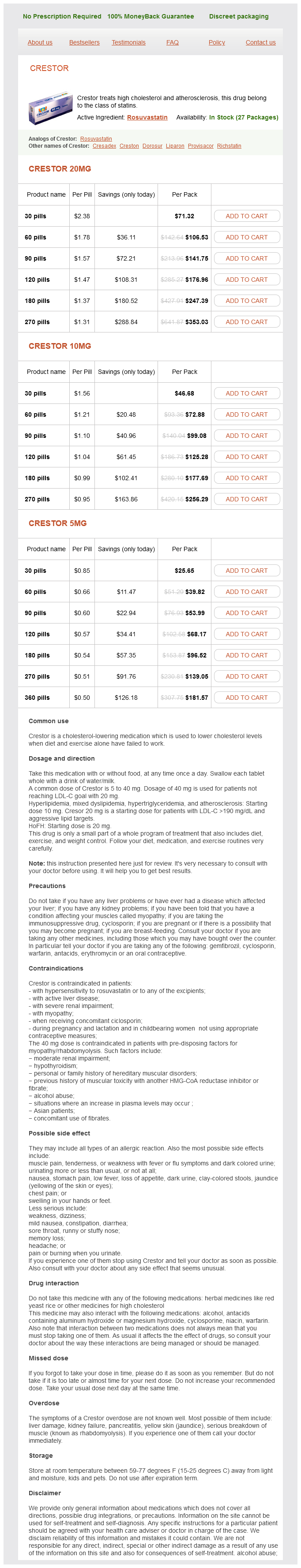
Crestor Dosage and Price
Crestor 20mg
- 30 pills - $71.32
- 60 pills - $106.53
- 90 pills - $141.75
- 120 pills - $176.96
- 180 pills - $247.39
- 270 pills - $353.03
Crestor 10mg
- 30 pills - $46.68
- 60 pills - $72.88
- 90 pills - $99.08
- 120 pills - $125.28
- 180 pills - $177.69
- 270 pills - $256.29
Crestor 5mg
- 30 pills - $25.65
- 60 pills - $39.82
- 90 pills - $53.99
- 120 pills - $68.17
- 180 pills - $96.52
- 270 pills - $139.05
- 360 pills - $181.57
If an initial Pap test result is negative lowering good cholesterol foods list buy crestor 10 mg free shipping, testing should be repeated 6 or 12 months later and then continued every 12 months. After three consecutive, negative Pap test results, the interval of Pap testing can be extended to 3 years. For women aged ~30 years, cytology screening can be followed as just described, or cotesting every 3 years can begin. Cervical cancer screening is continued indefinitdy even in those aged 65 years or older who have been adequately screened. Those with prior high-grade cervical neoplasia or cancer should have annual vaginal cuff cytology. A digital examination of the anal canal to detect masses is recommended routinely. Anal cytology testing is discouraged unless referral to centers that offer high-resolution anoscopy is available to address abnormal results. The absence of a cervix should be confirmed by examination or pathology report, as many women are inaccurate in their personal reporting of hysterectomy type. Women who have undergone supracervical hysterectomy should continue routine screening. Recommendations for vaginal cytology after total hysterectomy in women with prior highgrade cervical neoplasia or cancer are less clear. Vaginal cancer is still rare in these individuals, and screening offers uncertain benefit (Saslow, 2012). The American College of Obstetricians and Gynecologists (2018b) recommends Pap testing of the vaginal cuff every 3 years for 20 years after initial posttreatrnent surveillance, which is traditionally a schedule of three Pap tests in the first 2 years posthysterectomy. Vaginal cuff cytology should be collected such that the chosen collection device makes optimal contact with the upper vaginal walls. The cuff is sampled with gentle but firm pressure, drawing the device across it several times in the same direction so as not to lose cells. Deep indentations in the vaginal cuff can be sampled with an endocervical brush, and these cells are added to the transport medium. Women with diabetes mdlitus or those with rheumatoid arthritis or inflammatory bowd disease not treated with immune suppressants can be screened according to guiddines for average-risk women. Clinically, the key elements reported are specimen adequacy and epithelial cell abnormalities Tables 29-3 and 29-4 (National Cancer Institute Workshop, 1989; Nayar, 2015; Solomon, 2002). The 2014 Bethesda System Cytology Report Components Specimen Type Conventional (Pap smear) Liquid-based (Pap test) Other Specimen Adequacy Satisfactory for evaluation Unsatisfactory for evaluation reason specified) General Categorization (optional) (American College of Obstetricians and Gynecologists, 2018b; Massad, 2013). Moreover, recommendations cannot address all clinical situations and individualized management is essential. These will offer more customized management of individual patients depending on their past and current results (Castle, 2019; Demarco, 2017). Specimen Adequacy this is reported as satisfactory or unsatisfactory for evaluation and is based on slide cellularity and the presence of obscuring blood or inflammation. If atrophy or a specific cervical or vaginal infection is present, treatment before repeat cytology may be helpful. Rarely, obscuring blood or inflammation on cervical cytology sample indicates invasive cancer. Negative for intraepithelial lesion or malignancy Epithelial cell abnormality (see Table 29-4) Other (see Interpretation/Results) Interpretation/Results Negative for intraepithelial lesion or malignancy Epithelial cell abnormalities (see Table 29-4) Non-neoplastic findings (optional) Cellular variations (atrophy, keratosis, metaplasia) Reactive cellular changes (inflammation, repair, radiation) Glandular cells status posthysterectomy Organisms Trichomonas vagina/is Fungal organisms consistent with Candida spp. Shift in flora suggestive of bacterial vaginosis Cellular changes consistent with herpes simplex virus Cellular changes consistent with cytomegalovirus Bacteria consistent with Actinomyces spp. Other nonneoplastic findings (optional) Other Endometrial cells in a woman ~45 years of age Other malignant neoplasms (specified) Adjunctive Testing Computer-Assisted Interpretation Educational Notes and Comments (optional) Epithelial Cell Abnormality Management A cytology report interprets a screening test and does not provide a final diagnosis. Instead, a final diagnosis is determined Preinvasive Lesions of the Lower Anogenital Tract 633 subsequently by colposcopy and directed biopsies, as indicated. The endocervical cells are viewed from the side in this fragment, Imparting a "picket fence- appearance. Normal squamous cells representative of the superficial eplthellal layer eoslnophlllc-stalnlng cell) and Intermediate cell layer basophilic-staining cells) lfe In the background. The dysplastic squamous cells have nuclear membrane irregularities and a high nucleus-to-cytoplasm ratio, reflecting cytologlc Immaturity. Altematively, immediate excision is acceptable in some nonpregnant patients depending on other fu. Adenocarcinoma cytology can be designated as endoccrvical, endometrial, or exttauterine. The risk of endometrial and other reproductive tract cancers and risk of cancers at other sites such as breast, ovary, and colon are also elevated. It also includes endometrial sampling in patients aged ~35 years or in younger women with risk fu. If atypical endometrial cells are specified in the cytology report, initial endometrial and endocervical sampling are acceptable. If initial evaluation of a glandular abnormality is negative, funher management and surveillance should be guided by current clinical guidelines. Cytology results suspicious for squamous cell carcinoma or adenocarcinoma are rare and carry the highest risk of invasive cancer. If initial evaluation fails to reveal invasive cancer, a diagnostic excision procedure is indicated. Clinical Considerations Directing Colposcopy Clinical objedives Provide a magnified view of cervix, vagina Identify cervical squamocolumnar junction Detect lesions suspicious for neoplasia Direct lesion biopsy Cllnlcal Indications Abnormal or recurrent inadequate cervical cancer screening result Grossly visible cervical lesion Unexplained lower genital tract bleeding Unexplained vaginal discharge Contraindications: none Relative contraindications Upper or lower reproductive tract infection Uncontrolled, severe hypertension Uncooperative or overly anxious patient Table 29-5). Colposcopic examination is optimally timed to avoid menses but is not delayed if there is a visible cervical lesion or abnormal bleeding, or if the patient is unlikely to return. In cases of severe cervicitis or other pelvic infection, treatment may be indicated before performing biopsies or endocervical curettage. However, abnormal cervical discharge without an identified pathogen may be a cancer indicator.