Deltasone
General Information about Deltasone
Deltasone is primarily used to deal with situations that contain inflammation, together with allergic reactions, bronchial asthma, rheumatoid arthritis, and certain pores and skin problems. It can also be useful in managing situations such as ulcerative colitis, which is a type of inflammatory bowel illness, and multiple sclerosis, which is an autoimmune dysfunction.
Before beginning Deltasone treatment, it's essential to debate the potential risks and advantages with a healthcare provider, particularly if the affected person has a history of allergic reactions or other medical situations.
For bronchial asthma sufferers, Deltasone helps to scale back airway inflammation and improve respiratory. It does so by lowering the production of mucus and swelling within the airways, making it easier for air to move out and in of the lungs.
Like another medicine, Deltasone is associated with some potential unwanted side effects. The commonest unwanted facet effects embrace elevated urge for food, weight acquire, temper adjustments, problem sleeping, and an increased threat of infections. These side effects usually subside as soon as the medicine is discontinued or the dosage is lowered.
It is necessary to note that Deltasone should not be stopped abruptly, as it could possibly cause withdrawal signs such as fatigue, joint ache, and fever. The dosage should be progressively decreased under the supervision of a medical professional to avoid these signs.
In ulcerative colitis, Deltasone is prescribed to reduce inflammation and relieve signs such as stomach pain, diarrhea, and rectal bleeding. It works by concentrating on the immune system and decreasing the production of chemical compounds that cause irritation in the colon.
Deltasone is a medication that falls underneath the class of corticosteroids, which are hormones produced by the adrenal glands. It is usually prescribed to reduce inflammation and alleviate signs in various conditions corresponding to ulcerative colitis and asthma.
Deltasone is available in various varieties, including tablets, liquid, and injectable form. The dosage and length of treatment rely upon the specific situation being handled, the severity, and the affected person's response to the treatment.
In conclusion, Deltasone is a broadly used treatment for managing varied situations that involve inflammation. It is a potent anti-inflammatory drug that helps to cut back signs and improve the standard of life for patients. However, you will need to use this medication under the guidance of a medical professional and to remember of the potential unwanted facet effects. With proper use, Deltasone may be an efficient and important remedy option for these suffering from inflammatory situations.
One of the main features of Deltasone is to suppress the immune system's response to inflammation, which is the physique's natural response to injury or infection. By doing so, it helps to reduce redness, swelling, ache, and different signs associated with irritation.
In some circumstances, Deltasone can also cause extra severe side effects, including hypertension, diabetes, osteoporosis, and cataracts. It is essential to inform the physician of any pre-existing medical conditions earlier than starting Deltasone therapy.
Zidovudine use in the context of triple nucleoside analog therapy has also been investigated allergy medicine hydroxyzine deltasone 20 mg purchase with amex. Randomized data are lacking to support the use of zidovudine with more recently introduced antiretroviral agents. However, observational data support the efficacy of the triple combination of zidovudine with lamivudine and raltegravir (an integrase inhibitor) in both treatment-naive and experienced patients (Kang et al. Zidovudine has fallen out of favor both because of high rates of less-serious short-term toxicities (such as nausea malaise and headache) and because of the risk of long-term side effects such as mitochondrial toxicity and related lipoatrophy. The mechanism of this effect may be through prolongation of platelet survival, with zidovudine therapy associated with decreased plasma levels of glycocalicin, a platelet protein that correlates inversely with platelet survival (Panzer et al. The response time may be highly variable (median, 912 weeks), but bleeding episodes resolve with therapy and the positive effects of zidovudine on platelet count may persist for more than 18 months even with 7. Some reports suggest that high doses (1000 mg per day) of zidovudine may be more effective at increasing platelet count than standard doses (500600 mg per day) (Boyar and Beall, 1991; Landonio et al. More recent work provides strong evidence for the efficacy of combination antiretroviral therapy in this setting (Atta et al. Subsequent reports also supported a possible role for zidovudine in the management of this condition (Dalakas et al. There is no direct evidence available for this strategy in the setting of postexposure prophylaxis and no randomized trial is ever likely to be undertaken. In particular, both animal and human data support the safety and efficacy of zidovudine for use in this context. The women 3682 Zidovudine were treated with zidovudine (100 mg orally five times daily before delivery, 2 mg/kg i. Subsequent work has also demonstrated the importance of commencing infant zidovudine therapy as soon as possible (and within the first 48 hours) after birth for maximum efficacy (Wade et al. A recent study has shown clearly that combining extended zidovudine therapy (up to 6 weeks of age) with extended nevirapine treatment of newborns substantially reduced the incidence of nevirapine resistance (Lidström et al. Thymidine and zidovudine metabolism in chronically zidovudine-exposed cells in vitro. Zidovudine did not enhance the antiviral effect of interferon-alpha (Janssen et al. A pilot study examined the efficacy of adding zidovudine to interferon-alpha in the treatment of hepatitis C virus. A total of 30 patients with chronic hepatitis C infection were enrolled for interferon-alpha (36 million units per day for 3 weeks and then three times weekly for 21 weeks) with oral zidovudine (500 mg per day, commencing at the beginning of week 8 of interferon-alpha therapy). Lactic acidemia in human immunodeficiency virus-uninfected infants exposed to perinatal antiretroviral therapy. A case of acute encephalopathy caused by the human immunodeficiency virus apparently responsive to zidovudine. Kinetic and inhibitor studies of acetaminophen and zidovudine glucuronidation in rat liver microsomes. In vitro inhibition of hepatitis B virus replication by 2,3 -dideoxyguanosine, 2,3 -dideoxyinosine, and 3-azido-2,3-dideoxythymidine in 2. Thymidine and 3-azido-3-deoxythymidine metabolism in human peripheral blood lymphocytes and monocyte-derived macrophages. Ribavirin antagonizes inhibitory effects of pyrimidine 2,3-dideoxynucleosides but enhances inhibitory effects of purine 2,3-dideoxynucleosides on replication of human immunodeficiency virus in vitro. Pharmacokinetics of zidovudine administered intravenously and orally in children with human immunodeficiency virus infection. The pharmacokinetics of zidovudine administered by continuous infusion in children. The in vitro and in vivo antiretrovirus activity, and intracellular metabolism of 3-azido-2,3dideoxythymidine and 2,3-dideoxycytidine are highly dependent on the cell species. Acquired immune deficiency syndrome-related pulmonary non-Hodgkin lymphoma regressing after zidovudine therapy. Zidovudine-based lyticinducing chemotherapy for Epstein-Barr virus-related lymphomas. Treatment of adult T-cell leukaemia/ lymphoma: current strategy and future perspectives. Meta-analysis on the use of zidovudine and interferon-alfa in adult T-cell leukemia/lymphoma showing improved survival in the leukemic subtypes. Synergistic cytotoxic effect of azidothymidine and recombinant interferon alpha on normal human bone marrow progenitor cells. Persistent mitochondrial dysfunction and perinatal exposure to antiretroviral nucleoside analogues. A high incidence of lactic acidosis and symptomatic hyperlactatemia in women receiving highly active antiretroviral therapy in Soweto, South Africa. Ordered appearance of zidovudine resistance mutations during treatment of 18 human immunodeficiency virus-positive subjects. Zidovudine sensitivity of human immunodeficiency viruses from high-risk, symptom-free individuals during therapy. Effects of discontinuation of zidovudine treatment on zidovudine sensitivity of human immunodeficiency virus type 1 isolates. Phase I evaluation of zidovudine administered to infants exposed at birth to the human immunodeficiency virus. Effect of continuous-infusion zidovudine therapy on neuropsychologic functioning in children with symptomatic human immunodeficiency virus infection. Short-term, combined use of paracetamol and zidovudine does not alter the pharmacokinetics of either drug. Susceptibilities of human immunodeficiency virus type 1 enzyme and viral variants expressing multiple resistance-engendering amino acid substitutions to reserve transcriptase inhibitors. Inhibition of human immunodeficiency virus type 1 replication in vitro by the bisheteroarylpiperazine atevirdine (U-87201E) in combination with zidovudine or didanosine.
Ether lipid-ester prodrugs of acyclic nucleoside phosphonates: activity against adenovirus replication in vitro allergy testing using saliva deltasone 10 mg buy without a prescription. The effects of cidofovir 1% with and without cyclosporin a 1% as a topical treatment of acute adenoviral keratoconjunctivitis: a controlled clinical pilot study. Cytotoxicity of antiviral nucleotides adefovir and cidofovir is induced by the expression of human renal organic anion transporter 1. Intracellular metabolism of the antiherpes agent (S)-1-[3-hydroxy-2-(phosphonylmethoxy)propyl]cytosine. Adenoviral infections and a prospective trial of cidofovir in pediatric hematopoietic stem cell transplantation. Alkoxyalkyl prodrugs of acyclic nucleoside phosphonates enhance oral antiviral activity and reduce toxicity: current state of the art. Enhanced antiproliferative effects of alkoxyalkyl esters of cidofovir in human cervical cancer cells in vitro. Successful cidofovir treatment of smallpox-like disease in variola and monkeypox primate models. Refractory human papillomavirus-associated oral warts treated topically with 13% 7. Clinical uses of the drug 3567 cidofovir solutions in human immunodeficiency virus type 1-infected patients. Selective inhibition of human papillomavirusinduced cell proliferation by (S)-1-[3-hydroxy-2-(phosphonylmethoxy) propyl]cytosine. Evaluation of nucleoside phosphonates and their analogs and prodrugs for inhibition of orthopoxvirus replication. Oral treatment of murine cytomegalovirus infections with ether lipid esters of cidofovir. Enhanced inhibition of orthopoxvirus replication in vitro by alkoxyalkyl esters of cidofovir and cyclic cidofovir. Adenovirus-associated hemorrhagic cystitis in a pediatric renal transplant recipient. Transmission of monkeypox among persons exposed to infected prairie dogs in Indiana in 2003. Effects of cidofovir treatment on cytokine induction in murine models of cowpox and vaccinia virus infection. Successful treatment of recurrent vulvar intraepithelial neoplasia resistant to interferon and isotretinoin with cidofovir. Inhaled cidofovir as an adjuvant therapy for recurrent respiratory papillomatosis. Inhibitory activities of three classes of acyclic nucleoside phosphonates against murine polyomavirus and primate simian virus 40 strains. Progressive orf virus infection in a patient with lymphoma: successful treatment using imiquimod. Early diagnosis of adenovirus infection and treatment with cidofovir after bone marrow transplantation in children. Real-time blood plasma polymerase chain reaction for management of disseminated adenovirus infection. Potent inhibition of hemangioma formation in rats by the acyclic nucleoside phosphonate analogue cidofovir. Inhibitory effects of acyclic nucleoside phosphonate analogs, including (S)-1-(3-hydroxy-2phosphonylmethoxypropyl)cytosine, on Epstein-Barr virus replication. Cidofovir for cytomegalovirus infection and disease in allogeneic stem cell transplant recipients. The Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Cidofovir for adenovirus infections after allogeneic hematopoietic stem cell transplantation: a survey by the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Successful treatment of an acyclovir- and foscarnet-resistant herpes simplex virus type 1 lesion with intravenous cidofovir. Treatment of herpesvirus associated primary effusion lymphoma with intracavity cidofovir. Susceptibility of human herpesvirus 6 to antiviral compounds by flow cytometry analysis. Intravenous cidofovir for resistant cutaneous warts in a patient with psoriasis treated with monoclonal antibodies. A rapid screening assay identifies monotherapy with interferon-ss and combination therapies with nucleoside analogs as effective inhibitors of Ebola virus. The lipid moiety of brincidofovir is required for in vitro antiviral activity against Ebola virus. Resolution of recalcitrant molluscum contagiosum virus lesions in human immunodeficiency virus-infected patients treated with cidofovir. Monitoring of Epstein-Barr virus load after hematopoietic stem cell transplantation for early intervention in post-transplant lymphoproliferative disease. Biochemical basis for increased susceptibility to cidofovir of herpes simplex viruses with altered or deficient thymidine kinase activity. The impact of cidofovir treatment on viral loads in adult recurrent respiratory papillomatosis. Prevention and inhibition of nasopharyngeal carcinoma growth by antiviral phosphonated nucleoside analogs.
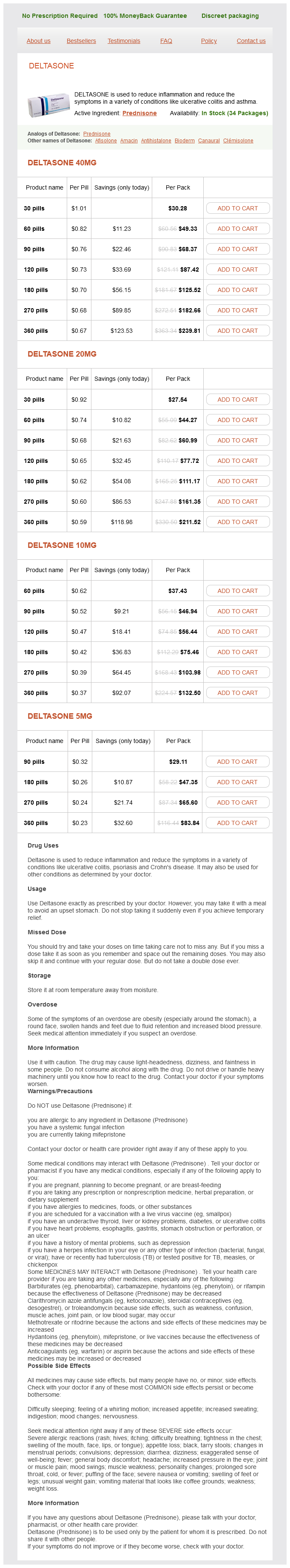
Deltasone Dosage and Price
Deltasone 40mg
- 30 pills - $30.28
- 60 pills - $49.33
- 90 pills - $68.37
- 120 pills - $87.42
- 180 pills - $125.52
- 270 pills - $182.66
- 360 pills - $239.81
Deltasone 20mg
- 30 pills - $27.54
- 60 pills - $44.27
- 90 pills - $60.99
- 120 pills - $77.72
- 180 pills - $111.17
- 270 pills - $161.35
- 360 pills - $211.52
Deltasone 10mg
- 60 pills - $37.43
- 90 pills - $46.94
- 120 pills - $56.44
- 180 pills - $75.46
- 270 pills - $103.98
- 360 pills - $132.50
Deltasone 5mg
- 90 pills - $29.11
- 180 pills - $47.35
- 270 pills - $65.60
- 360 pills - $83.84
Approximately 15% of patients virologically suppressed on a protease inhibitorcontaining regimen and then switched to a nonnucleoside reverse transcriptase inhibitor regimen for simplification or toxicity reasons will subsequently develop viral rebound allergy testing redmond wa deltasone 10 mg order on line, likely due to archived nucleoside analog mutations, which facilitate the emergence of mutations to the nonnucleoside reverse transcriptase component of the regimen (Masquelier et al. Nevirapine resistance mutations occur in the majority of protease inhibitorexperienced patients (92%) failing a subsequent nevirapine plus protease inhibitor regimen by 24 weeks. The Y181C mutation accounted for 76% of nonnucleoside reverse transcriptase inhibitor mutations and was seen alone in 15% of isolates. Because nevirapine has a long half-life and is eliminated from the body slowly, exposure to suboptimal nevirapine levels in maternal and infant plasma as well as breast milk for up to 3 weeks promotes the rapid selection of nevirapine-resistant viruses. Several studies have documented frequencies of acquisition of resistance mutations to nevirapine of 1569% after singedose intervention strategies (Arrive et al. The following nevirapine resistance mutations have been selected after a single 200-mg dose of nevirapine: K103N, V106A, Y181C, Y188C, and G190A (Eshleman et al. The Y181C mutation is commonly detected first (7 days after single-dose nevirapine) and often becomes undetectable at 68 weeks, when the K103N mutation is most frequently observed (Eshleman et al. The rates of resistance vary according to subtype, with 3069% in subtype C, 35% for subtype D, and 19% for subtype A (Eshleman et al. In addition, nevirapine resistance mutations have been detected 48 weeks postpartum in the breast milk of 4065% of women infected with subtypes A, C, and D who received a single dose of nevirapine for prevention of mother to child transmission (Hudelson et al. Individuals with subtype C infection experiencing virological failure with nevirapine-based treatment regimens, 82% had mutations present, of which the Y181C, V106A, K103N, V106M, G190A, and V108I predominated (Wallis et al. Antimicrobial activity 3859 mutations detected in one compartment only (Lee et al. There was no difference in rates of selection of nevirapine resistance at 14 weeks in infants exposed to extended nevirapine versus extended nevirapine plus zidovudine prophylaxis (83% vs. K103N- and Y181C-resistant variants persisted in 83% of infants at 6 months and 66% at 12 months (Fogel et al. There does not appear to be an increase in detection of resistance mutations in subsequent pregnancies when a single dose of nevirapine is used in both pregnancies. The prevalence of resistance mutations was similar regardless of whether women had received a single dose of nevirapine for the first pregnancy (33%), whether they had taken two doses in the same pregnancy (25%), or whether they had received a single dose for the second time in a subsequent pregnancy (27%), with the most common mutations being K103N and V106A/M (Flys et al. The presence of resistance mutations has been shown to decrease the virological response to nevirapine-containing combination antiretroviral regimens if initiated within 6 months after exposure to single-dose nevirapine (Jourdain et al. Detection of K103N in women after a single dose of nevirapine was associated with reduced likelihood of achieving and maintaining virological suppression (61% vs. The risk of virological failure is greater for women after single-dose nevirapine compared with women with low frequency detectable nevirapine-resistant variants not exposed to single-dose nevirapine (Boltz et al. The prevalence of nevirapine resistance was reduced in infants by the addition of zidovudine (4 mg/kg twice daily for 1 week) to single-dose nevirapine (Eshleman et al. Resistance after treatment interruption Resistance mutations were detected in 20% of subjects with viral suppression who were enrolled in a treatment interruption study after discontinuation of antiretroviral therapy. Continuation of the nucleoside reverse transcriptase backbone of a nevirapine-containing regimen for a further 5 days after discontinuation of nevirapine continues inhibition of viral replication during the period of the plasma half-life decay of nevirapine and may prevent emergence of mutations associated with nevirapine resistance (Mackie et al. Occasional subtype C viruses from treatment-naive individuals have the G190A substitution, causing high-level resistance to nevirapine, due to the presence of naturally occurring polymorphisms associated with this subtype (Loemba et al. In general, nevirapine resistance mutations are rare in treatment-naive women infected with subtypes A, C, or D (Church et al. For example, G190E exhibits greater impairment of replication capacity than other mutations within this codon (Huang et al. The most common mutation appearing after nevirapine failure is the Y181C substitution, which confers high-level resistance to nevirapine in 100% of cases (Casado et al. In comparison, 29% of viral isolates with the Y181C mutation remain fully susceptible to efavirenz, but only 14% remain susceptible to delavirdine (Casado et al. Patients with phenotypic susceptibility to efavirenz after failing on a nevirapine-containing regimen had a significantly greater reduction in viral load (1. Early virologic responses in the presence of Y181C are observed, but are short-lived and generally lost by 8 weeks (Antinori et al. The presence of K103N selected by nevirapine is not associated with reduced susceptibility to rilpivirine or etravirine in vitro; however, clinical confirmation is required (Melikian et al. The prevalence of nevirapine hypersusceptibility is estimated to be 840% among samples submitted for resistance testing. Hypersusceptibility is associated with nucleoside reverse transcriptase inhibitor resistance (Shulman et al. However, the multinucleoside reverse transcriptase inhibitor resistance mutation Q151M is associated with reduction in nevirapine hypersusceptibility (Whitcomb et al. It is unknown whether in vitro hypersusceptibility consistently translates to superior virologic efficacy and clinical response in vivo. It has also been demonstrated in adults that the Y181C mutation is able to restore partial susceptibility to zidovudine in the setting of zidovudine resistance (Larder, 1992). Nevirapine has been shown to inhibit the removal of nucleoside analog monophosphate entities from the catalytic site, thus maintaining the chain termination effect (Basavapathruni et al. Consistent with these mechanistic observations, synergistic interactions have been reported for nevirapine when used in vitro in combination with the nucleoside analog reverse transcriptase inhibitors zidovudine (Koup et al. Nevirapine is bound in a hydrophobic pocket created on contact of the inhibitor with the enzyme in the p66 "palm" of reverse transcriptase, near but not overlapping the polymerase active site and in contact with the "thumb" subdomain of reverse transcriptase (De Clercq, 1993; Kohlstaedt et al. The two binding sites are spatially and functionally associated, such that synergistic activity would be expected when the two drug classes are combined (De Clercq, 1998). When nevirapine is not present, the pocket site is filled by the tyrosines of codons 181 and 188, and a pocket is formed only when these aromatic side chains rotate (Tantillo et al. Nevirapine has a decreased affinity for the mutant compared with wild-type reverse transcriptase due to a faster inhibitor dissociation rate from the wild-type enzyme (Spence et al. Others consider that only polymerase and not ribonuclease H function is affected by this group of compounds (Loya et al. The lead-in period of 200 mg daily must not continue beyond 28 days due to risk of development of resistance.