Desyrel
General Information about Desyrel
Desyrel has been out there available within the market for over 30 years and has proven significant success in treating despair. It was first introduced in 1981 as a therapy for melancholy, however later studies have proven its effectiveness in treating different psychiatric issues, corresponding to anxiousness and insomnia.
Desyrel is out there in numerous types, such as instant and extended-release tablets, however it is essential to comply with the instructions supplied by the physician or pharmacist. The preliminary dose typically starts low and progressively increases until the desired therapeutic impact is achieved. It could take several weeks for Desyrel to reach its full impact, and it's essential to continue taking the medication as prescribed, even if the signs improve, to prevent a relapse.
In conclusion, Desyrel is a extensively prescribed antidepressant that has been proven efficient in restoring the imbalance of chemicals within the brain that can lead to despair. Its helpful aspect impact profile, ease of use, and multiple varieties make it an attractive choice for individuals fighting this dysfunction. However, like all medication, it's important to make use of Desyrel as prescribed and to communicate any considerations with a healthcare supplier for appropriate administration. With the right therapy plan, depression may be effectively managed, and individuals can lead fulfilling lives.
The precise mechanism of how Desyrel works isn't totally understood, however it is believed to influence the degrees of serotonin, a chemical that controls temper, sleep, and appetite. It works by blocking the serotonin receptors, preventing the reuptake of serotonin by the neurons in the mind, which will increase the levels of serotonin available to improve temper and alleviate symptoms of melancholy.
As with any medication, Desyrel has potential side effects, though they're normally delicate and may resolve on their very own over time. These may include nausea, dry mouth, headache, dizziness, and constipation. In rare circumstances, extra severe unwanted aspect effects, such as changes in blood stress, heart rhythm, and liver injury, might occur. It is essential to debate any regarding symptoms with a healthcare supplier instantly.
Desyrel, also known by its generic name, Trazodone, is an antidepressant medication commonly prescribed for the treatment of depression. It belongs to a category of drugs known as serotonin antagonist and reuptake inhibitors (SARIs) that work by restoring the balance of sure chemical substances within the brain, specifically serotonin and norepinephrine. These chemical substances are responsible for regulating temper and emotions and once they become imbalanced, it could lead to melancholy.
One of the advantages of Desyrel is that it has a favorable side effect profile compared to other antidepressants. It is well-tolerated by most patients and has a lower probability of causing sexual dysfunction, weight achieve, or sedation, which are widespread unwanted facet effects of other antidepressants. This makes it a preferred selection for older adults, who could also be more delicate to unwanted effects.
Depression is a standard psychological well being disorder affecting more than 264 million individuals globally. It is characterized by persistent feelings of disappointment, lack of curiosity in actions, modifications in appetite, problem sleeping, and low energy. Some individuals may experience thoughts of hopelessness and worthlessness, making it difficult to carry out daily activities. Fortunately, with correct treatment, depression can be managed, and Desyrel is one of the medicines most prescribed by docs.
Inhaled glucocorticoids are first-line therapy for management of the inflammatory component of asthma anxiety symptoms rash order desyrel 100 mg online. Inhaled glucocorticoids are very effective and are much safer than systemic glucocorticoids. Because of their potential for toxicity, these drugs are prescribed only when symptoms cannot be controlled with safer medications (inhaled glucocorticoids, inhaled beta2 agonists). Because the risk for toxicity increases with duration of use, treatment should be as brief as possible. These preparations are largely devoid of serious toxicity, even when used in high doses. The most common adverse effects are oropharyngeal candidiasis and dysphonia (hoarseness, speaking difficulty). To minimize these effects, patients should rinse the mouth with water and gargle after each administration. With long-term, high-dose therapy, some adrenal suppression may develop, although the degree of suppression is generally low. In contrast, with prolonged use of oral glucocorticoids, adrenal suppression can be profound. Glucocorticoids can slow growth in children and adolescents-but these drugs do not decrease adult height. Short-term studies have shown that inhaled glucocorticoids slow growth; however, long-term studies indicate that adult height, while delayed, is not reduced. Less is known regarding whether glucocorticoids suppress growth and development of the brain, lungs, and other organs, in part because having asthma alone can affect organ growth. Because the benefits of inhaled glucocorticoids tend to be much greater than the risks, current guidelines for asthma management recommend these drugs for children while monitoring for evidence of complications. Fortunately, the amount of loss is much lower than the amount caused by oral glucocorticoids. To minimize bone loss, patients should (1) use the lowest dose that controls symptoms, (2) ensure adequate intake of calcium and vitamin D, and (3) participate in weight-bearing exercise. There has been concern that prolonged therapy might increase the risk for cataracts and glaucoma. While this may be an issue of concern with continuous use of high-dose inhaled glucocorticoids, this problem is not associated with long-term use of low to medium doses of inhaled glucocorticoids. When used acutely (less than 10 days), even in very high doses, oral glucocorticoids do not cause significant adverse effects. Potential adverse effects include adrenal suppression, osteoporosis, hyperglycemia, peptic ulcer disease, and, in young patients, growth suppression. As discussed in Chapter 72, prolonged glucocorticoid use can decrease the ability of the adrenal cortex to produce glucocorticoids of its own. If systemic therapy is stopped suddenly, as when switching from oral therapy to inhalation therapy, the patient can die. Similarly, during times of severe physical stress when the body would normally produce high levels of glucocorticoids, if the dose of systemic glucocorticoids is not increased to meet the increased need, the patient can die. When discontinuing a systemic glucocorticoid, you must be sure that it is done gradually to allow the body to resume production of the endogenous hormone. On the other hand, if a patient taking systemic glucocorticoids experiences severe physical stress, such as a motor vehicle crash, or is scheduled for a stressful procedure such as surgery, you must make certain that the provider remembers to prescribe additional glucocorticoids to supplement for the endogenous hormone that the patient cannot produce. For long-term treatment, alternate-day dosing is recommended to minimize adrenal suppression. After symptoms have been controlled for 3 months, dosages should be decreased gradually to establish the lowest dosage that can keep the patient free of symptoms. As discussed previously, the dosage of oral glucocorticoids must be increased during times of stress. Adrenal suppression is also a concern when discontinuing prolonged use of oral glucocorticoids or when transferring from an oral route to an inhaled route. Several months are required for recovery of adrenocortical function, so it is important to decrease the dosage gradually. A complete list of contraindications to oral glucocorticoids is presented in the Summary of Major Nursing Implications at the end of this chapter. In patients with asthma, these drugs can decrease bronchoconstriction and inflammatory responses such as edema and mucus secretion. Three leukotriene modifiers are currently available: zileuton, zafirlukast, and montelukast. Zileuton blocks leukotriene synthesis; zafirlukast and montelukast block leukotriene receptors. Current guidelines recommend using these agents as second-line therapy (if an inhaled glucocorticoid cannot be used) and as add-on therapy when an inhaled glucocorticoid alone is inadequate. Although generally well tolerated, all the leukotriene modifiers can cause adverse neuropsychiatric effects, including depression, suicidal thinking, and suicidal behavior. The dosage should be kept as low as possible to minimize adrenal suppression, possible bone loss, and other adverse effects. Budesonide suspension [Pulmicort Respules] is the first inhaled glucocorticoid formulated for nebulized dosing. The product is approved for maintenance therapy of persistent asthma in children 1 to 8 years old. Improvement should begin in 2 to 8 days; maximal benefits may take 4 to 6 weeks to develop.
This route has three advantages: (1) therapeutic effects are enhanced by delivering drugs directly to their site of action anxiety disorder 3000 generic desyrel 100 mg buy, (2) systemic effects are minimized, and (3) relief of acute attacks is rapid. Four types of inhalation devices are employed: metered-dose inhalers, Respimats, dry-powder inhalers, and nebulizers. When 2 inhalations are needed, an interval of at least 1 minute should separate the first inhalation from the second. Accordingly, patients will need a demonstration, as well as written and verbal instruction. About 80% affects the oropharynx and is swallowed, and the remaining 10% is left in the device or exhaled. Some spacers contain a one-way valve that activates upon inhalation, obviating the need for good hand-breath coordination. Some spacers also contain an alarm whistle that sounds off when inhalation is too rapid, thus maximizing effective drug administration. They can also prevent bronchospasm that may occur with sudden intake of an inhaled drug. Note that, when a spacer is used, more medication reaches its site of action in the lungs, and less is deposited in the mouth and throat. Patient Care Concerns Inhaled glucocorticoids are the preferred long-term treatment for children of all ages, including infants. Face masks are recommended for the administration of inhaled glucocorticoids to children younger than 4 years. Montelukast is the only leukotriene modifier approved for children ages 1 to 5 years. Of the leukotriene modifiers, montelukast and zafirlukast are Pregnancy Risk Category B,a while zileuton is Risk Category C. Inhaled glucocorticoids are much safer for this population than systemic formulations. Nebulizers A nebulizer is a small machine used to convert a drug solution into a mist. The droplets in the mist are much finer than those produced by inhalers, resulting in less drug deposit on the oropharynx and increased delivery to the lung. Inhalation of the nebulized mist can be done through a face mask or through a mouthpiece held between the teeth. Because the mist produced by a nebulizer is inhaled with each breath, hand-breath coordination is not a concern. Nebulizers take several minutes to deliver the same amount of drug contained in 1 inhalation from an inhaler, but for some patients, a nebulizer may be more effective than an inhaler. Although nebulizers are usually used at home or in a clinic or hospital, these devices, which weigh less than 10 pounds, are sufficiently portable for use in other locations. Adverse reactions to inhaled glucocorticoids are generally minor, as are reactions to systemic glucocorticoids taken acutely. However, when systemic glucocorticoids are used long term, severe adverse effects are likely. Mechanism of Antiasthma Action Glucocorticoids reduce asthma symptoms by suppressing inflammation. Specific anti-inflammatory effects include: · Decreased synthesis and release of inflammatory mediators. There is also some evidence that glucocorticoids may increase the number of bronchial beta2 receptors, as well as their responsiveness to beta2 agonists. Because beneficial effects develop slowly, these drugs cannot be used to abort an ongoing attack. Glucocorticoids do not alter the natural course of asthma, even when used in young children. Administration is done with a jet nebulizer equipped with a mouthpiece or face mask; ultrasonic nebulizers should not be used. For children who are not taking an oral glucocorticoid, the initial dosage is 500 mcg/day in one or two doses. For children who are taking an oral glucocorticoid, the initial dosage is 1000 mcg/day in one or two doses. Additional information on dosing of budesonide and other inhaled glucocorticoids is provided in Table 76. Methylprednisolone, prednisone, and prednisolone are preferred glucocorticoids for oral therapy of asthma. When beginning therapy with oral glucocorticoids, dosing initially focuses on bringing symptoms under control. Because effects are not immediate, zileuton cannot be used to abort an ongoing attack. Zileuton is less effective than an inhaled glucocorticoid alone, and appears to be less effective than a long-acting inhaled beta2 agonist as adjunctive therapy in patients not adequately controlled with an inhaled glucocorticoid. Mechanism of Action Benefits derive from inhibiting 5-lipoxygenase, the enzyme that converts arachidonic acid into leukotrienes. Pharmacokinetics Zileuton is given orally and undergoes rapid absorption, both in the presence and absence of food. Zileuton is rapidly metabolized by the liver, and the metabolites are excreted in the urine. A few patients have developed symptomatic hepatitis, which reversed after drug withdrawal. The recommended schedule is once a month for 3 months, then every 2 to 3 months for the remainder of the first year, and periodically thereafter. Postmarketing reports indicate that zileuton and the other leukotriene modifiers can cause adverse neuropsychiatric effects, including depression, anxiety, agitation, abnormal dreams, hallucinations, insomnia, irritability, restlessness, and suicidal thinking and behavior.
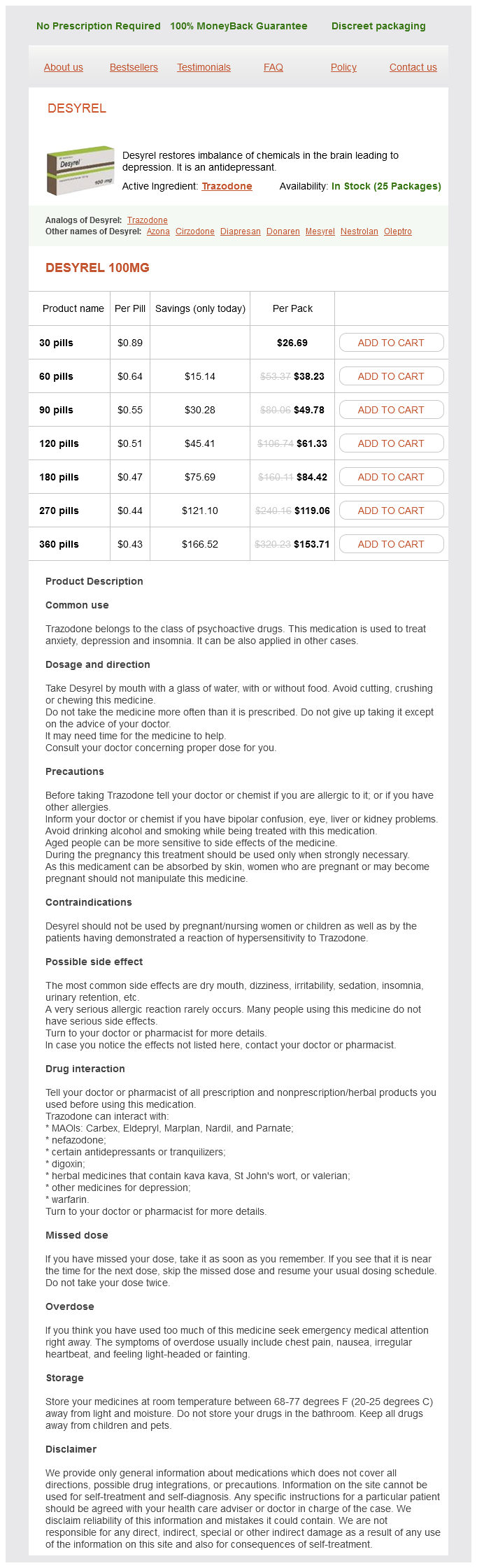
Desyrel Dosage and Price
Desyrel 100mg
- 30 pills - $26.69
- 60 pills - $38.23
- 90 pills - $49.78
- 120 pills - $61.33
- 180 pills - $84.42
- 270 pills - $119.06
- 360 pills - $153.71
As discussed in Chapter 64 anxiety symptoms 6 dpo discount 100 mg desyrel with mastercard, an oral formulation of tranexamic acid, marketed as Lysteda, is used to treat heavy cyclic menstrual bleeding. These antibodies, referred to as inhibitors, neutralize the clotting factor and thereby render factor replacement ineffective. In most cases, the antibodies develop early, typically after only 9 to 12 courses of treatment. The risk of inhibitor development among African American and Hispanic patients is unusually high (up to 50%). The procedure involves repeated administration of factor replacement products over an extended time. The success rate is high (63% to 83%) for patients with hemophilia A and very low for those with hemophilia B. No human proteins are used in making this agent, so there is no risk of transmitting a human virus. Treatment is very expensive: A single 90-mcg/ kg dose for a 70-kg patient costs about $13,000. Dosing can be repeated every 6 hours, but the total daily dose must not exceed 200 units/kg. Accordingly, selection between them is based on previous response and prescriber preference. Both options are effective because they bypass the blockade caused by the inhibitor. Hemophilia may be severe, moderate, or mild, depending on the degree of clotting factor deficiency. Patients with severe hemophilia may experience lifethreatening hemorrhage in response to minor trauma, whereas those with mild hemophilia may experience little or no excessive bleeding. Replacement therapy may be done prophylactically (to prevent bleeding and thus prevent joint injury) or on demand (to stop an ongoing bleed or to prevent excessive bleeding during surgery). All clotting factor concentrates, whether plasma derived or recombinant, are equally effective. However, because recombinant factors are, in theory, slightly safer than plasma-derived factors, recombinant factors are considered the treatment of choice. Although we can monitor the activity of clotting factors in blood to help guide treatment, dosage is ultimately determined by the clinical response. With both factors, the goal is to maintain plasma factor levels above 1% of normal. Two drugs-aminocaproic acid and tranexamic acid-can suppress fibrinolysis and can promote hemostasis in hemophilia A and hemophilia B. These antifibrinolytic agents are more effective for preventing recurrent bleeding than for stopping an ongoing bleed. Both factors may be given prophylactically (to prevent bleeding and subsequent joint injury) or "on demand" (to stop ongoing bleeding or prevent excessive bleeding during anticipated surgery). Identifying High-Risk Patients Use with caution in patients with a history of allergic reactions to the factor concentrate. Record the following each time you give a factor concentrate: · · · · Time and date Infusion site and rate Total dose Manufacturer, brand name, lot number, and expiration date of the factor concentrate therapy). Clotting factor concentrates can cause allergic reactions, ranging from mild to severe. Inform patients about symptoms of anaphylaxis (wheezing, tightness in the throat, shortness of breath, swelling in the face), and instruct them to seek immediate emergency care if these develop. Minimizing Adverse Interactions Teach home caregivers about: · the importance of having an assistant, who can give aid · · · · · · or call for help if complications arise the importance and proper method of hand washing Making dosage calculations Reconstituting the powdered factor concentrate Infusion technique Cleanup and waste disposal Recording the time, date, and other information listed in this section Aspirin. Ongoing Evaluation and Interventions Evaluating Therapeutic Effects Success is indicated by preventing bleeding (during prophylactic therapy) or controlling bleeding (during on-demand a Patient education information is highlighted as blue text. Most deficiency anemias result from deficiency of iron, vitamin B12, or folic acid. Uptake and Distribution the life cycle of iron begins with (1) uptake of iron into mucosal cells of the small intestine. Iron in the ferrous form (Fe++) is absorbed more readily than iron in the ferric form (Fe+++). Following uptake, iron can either (2a) undergo storage within mucosal cells in the form of ferritin (a complex consisting of iron plus a protein used to store iron) or (2b) undergo binding to transferrin (the iron transport protein) for distribution throughout the body. Utilization and Storage Iron that is bound to transferrin can undergo one of three fates. The majority of transferrin-bound iron (3a) is taken up by cells of the bone marrow for incorporation into hemoglobin. Small amounts (3b) are taken up by the liver and other tissues for storage as ferritin. Lastly (3c), some of the iron in plasma is taken up by muscle (for production of myoglobin), and some is taken up by all other tissues (for production of iron-containing enzymes). After hemoglobin is made in bone marrow, iron re-enters the circulation (4) as a component of hemoglobin in erythrocytes. Iron released by this process re-enters the plasma bound to transferrin (6), and then the cycle begins anew. Metabolic Functions Iron is essential to the function of hemoglobin, myoglobin (the oxygen-storing molecule of muscle), and a variety of iron-containing enzymes. In the discussion that follows, the numbers in parentheses refer to the circled numbers in the figure.