Diarex
General Information about Diarex
One of the main causes of diarrhea and dysentery is the presence of harmful micro organism in the digestive tract. Diarex's antibacterial properties help to remove these bacteria, providing relief from diarrhea and dysentery. In addition, the herb Coneru current in Diarex has been scientifically proven to inhibit the growth of micro organism corresponding to E. coli, Salmonella, and Shigella, which are frequent causes of diarrhea and dysentery. This makes Diarex an effective and secure way to manage these circumstances.
In conclusion, Diarex is a natural and effective resolution for managing diarrhea and dysentery. Its highly effective antibacterial and astringent properties provide aid from these circumstances while promoting overall digestive well being. With its time-tested natural formulation, Diarex is a protected and dependable selection for these looking for a pure approach to handle diarrhea and dysentery.
Another notable herb in Diarex is Shalmali, which has carminative properties. This means that it helps to relieve fuel and bloating, which might often accompany diarrhea and dysentery. This herb also has anti-inflammatory properties, making it efficient in soothing the inflamed intestinal lining and decreasing signs like abdominal ache and cramps.
Moreover, Diarex's astringent properties assist to contract the intestinal muscle tissue and cut back the frequency of bowel actions. This helps to regularize bowel actions and relieve signs such as stomach cramps and loose stools. The herb Guduchi present in Diarex has been discovered to have astringent properties that help to scale back intestinal irritation and soothe the digestive tract. This not solely supplies relief from diarrhea and dysentery but in addition promotes total digestive health.
Diarex is an herbal formulation that has been used for tons of of years in Ayurvedic medicine to deal with various gastrointestinal issues. It is a combination of herbs similar to Coneru, Guduchi, Shalmali, Shankh Bhasma, and Musta, which work synergistically to supply reduction from diarrhea and dysentery. These herbs have highly effective antibacterial and astringent properties, making Diarex a perfect alternative for managing these conditions.
What units Diarex other than other over-the-counter drugs is its natural formulation. The mixture of herbs in Diarex has been used in Ayurvedic medication for centuries to treat gastrointestinal issues. This makes it a safe and efficient choice for managing diarrhea and dysentery, even for long-term use.
Diarrhea and dysentery are common gastrointestinal problems that affect millions of people worldwide. These situations can be attributable to numerous factors such as viruses, micro organism, parasites, and meals poisoning. Often, individuals resort to over-the-counter drugs to alleviate the discomfort caused by these situations. However, these medications might solely provide temporary aid and might have antagonistic unwanted facet effects. This is the place Diarex is available in, a natural and efficient answer for managing diarrhea and dysentery.
Furthermore, Diarex additionally contains Shankh Bhasma, which is a supply of pure calcium and magnesium. These minerals play a vital position in maintaining the proper functioning of the digestive system. They help to strengthen the intestinal muscle tissue and promote wholesome digestion. Additionally, Shankh Bhasma has antacid properties that help to neutralize extra stomach acid, providing reduction from circumstances similar to acidity and heartburn, which are often associated with diarrhea and dysentery.
The brachium of the inferior colliculus (inferior quadrigeminal brachium) ascends ventrally gastritis diet foods to eat generic 30 caps diarex with amex. It conveys fibres from the lateral lemniscus and inferior colliculus to the medial geniculate body. On each side, the dorsal region is the tegmentum and the ventral part is the crus cerebri. Corticonuclear and corticospinal fibres occupy the middle two-thirds of the crura and descend via the pons and medulla. Corticonuclear fibres end in the nuclei of the cranial nerves and other Internal Structure Transverse Sections of the Midbrain Crus Cerebri Cerebral aqueduct Nucleus of inferior colliculus Mesencephalic tract and nucleus of trigeminal Lateral lemniscus Central tegmental tract Medial lemniscus Reticular formation Periaqueductal grey matter Trochlear nucleus Medial longitudinal fasciculus Temporopontine fibres Superior cerebellar peduncle Corticospinal and corticonuclear fibres Substantia nigra Frontopontine fibres Posterior perforated substance Crus cerebri Decussation of superior cerebellar peduncles Interpeduncular fossa. Corticopontine fibres arise in the cerebral cortex and form two groups, both of which end in the pontine nuclei. The frontopontine fibres from the frontal lobe, principally areas 6 and 4, traverse the internal capsule and then occupy the medial sixth of the ipsilateral crus cerebri. The temporopontine fibres, which are largely from the posterior region of the temporal lobe, traverse the internal capsule but occupy the lateral sixth of the ipsilateral crus. Parietopontine and occipitopontine fibres are also described in the crus, lying medial to the temporopontine fibres. There are few fibres from the primary sensory cortex in corticopontine projections. Mesencephalic Tegmentum the mesencephalic tegmentum is directly continuous with the pontine tegmentum and contains the same tracts. At inferior collicular levels, grey matter is restricted to scattered collections of neurones in the reticular formation and the tectum near the cerebral aqueduct. The trochlear nucleus is in the ventral grey matter near the midline, in a position corresponding to the abducens and hypoglossal nuclei at other levels. It extends through the lower half of the midbrain, just caudal to the oculomotor nucleus and immediately dorsal to the medial longitudinal fasciculus. The trigeminal mesencephalic nucleus occupies a lateral position in the central grey matter. It ascends from the upper pole of the main trigeminal sensory nucleus in the pons to the level of the superior colliculus in the midbrain and is accompanied by a tract of both peripheral and central branches from its axons. They are arranged in many small groups that extend as curved laminae on the lateral margins of the periaqueductal grey matter. Apart from these nuclei, the mesencephalic tegmentum contains many other scattered neurones, most of which are included in the reticular formation. Fibres enter the tegmentum and pass ventromedially around the central grey matter to the median raphe, where most cross in the decussation of the superior cerebellar penduncles and then separate into ascending and descending fascicles. Some ascending fibres either end in or give collaterals to the red nucleus, which they encapsulate and penetrate. Some uncrossed fibres are believed to end in the periaqueductal grey matter and reticular formation, interstitial nucleus and posterior commissural nucleus (nucleus of Darkshevich). The latter nucleus may send efferent fibres to the medial longitudinal fasciculus and posterior commissure. Descending fascicles end in the pontine and medullary reticular formation, the olivary complex and, possibly, cranial motor nuclei. The medial longitudinal fasciculus adjoins the somatic efferent column, dorsal to the decussating superior cerebellar peduncles. The medial, trigeminal, lateral and spinal lemnisci form a curved band dorsolateral to the substantia nigra. Some fibres of the lateral lemniscus end in the nucleus of the inferior colliculus, encapsulating it and synapsing with its neurones. The remaining fibres (direct lemniscal) join inferior colliculusderived fibres and enter the inferior quadrigeminal brachium, which starts at this level and carries the fibres to the medial geniculate body. Some fibres to the inferior colliculus are collaterals of direct lemniscal fibres. Superiorly, level with the superior colliculus, the tegmentum contains the red nucleus, which extends into the subthalamic region. The ventromedial central grey matter around the aqueduct contains the oculomotor nucleus, which is elongated and is related ventrolaterally to the medial longitudinal fasciculus and caudally reaches the trochlear nucleus. The oculomotor nucleus is divisible into neuronal groups that are partially correlated with the motor distribution of the oculomotor nerve. A group of preganglionic parasympathetic neurones, the accessory oculomotor (EdingerWestphal) nucleus, which controls the activity of smooth muscle within the eyeball (for pupillary constriction), lies dorsal to the oculomotor nucleus (Ch. Substantia Nigra the substantia nigra is a lamina of many multipolar neurones that extends through the whole midbrain, from the medial to the lateral crural sulcus and from the pons to the subthalamic region. The substantia nigra is semilunar in transverse section, concave dorsally and thicker medially, where it is traversed by oculomotor axons as they stream ventrally to their point of exit in the interpeduncular fossa. Extensions from its convex ventral surface pass between fibres of the crus cerebri. The substantia nigra is subdivided into a dorsal pars compacta and a ventral pars reticulata (reticularis), and the cells of these two parts have different connections. The pars compacta consists of many darkly pigmented neurones that contain neuromelanin granules. Their arrangement is irregular, and they partially penetrate the subjacent pars reticulata. The pars reticulata extends rostrally as far as the subthalamic region and is considered to be homologous with the medial segment of the globus pallidus, which it resembles structurally. There are reciprocal connections between the substantia nigra and the basal ganglia. Efferent fibres from the basal ganglia end largely, but by no means exclusively, in the pars reticulata. Topographically organized striatonigral fibres originate from the caudate nucleus and putamen and project to the pars reticulata.
All meningeal layers are derived from loose mesenchyme that surrounds the developing neural tube gastritis long term purchase diarex pills in toronto, termed the meninx primitiva or primary meninx. Mesenchymal cells projecting from the rostral end of the notochord, and those in the region of the prechordal plate, extend rostrally into the mesencephalic flexure and form the earliest cells of the tentorium cerebelli; at the beginning of its development, the medial part of the tentorium is predominantly leptomeningeal. By stage 17 (41 days), dura mater can be seen in the basal areas where the future chondrocranium is also developing. Precursors of the venous sinuses lie within the pachymeninx at stage 19 (48 days), and by stage 20, cell populations in the region of the future falx cerebri are proliferating, although the dorsal regions of the brain are not yet covered with putative meninges. By stage 23 (57 days), the dura is almost complete over the rhombencephalon and mesencephalon but is present only laterally around the prosencephalon. Subarachnoid spaces and most of the cisternae are present from this time, after the arachnoid mater becomes separated from the primitive dura mater by the accumulation of cerebrospinal fluid (which now has a net movement out of the ventricular system). The earlier medial portion disappears, leaving an incomplete partition that separates a subarachnoid area containing the telencephalon and diencephalon from one containing the cerebellum and rhombencephalon. There is a very close relationship, during development, between the mesenchyme from which the cranial dura mater is formed and that which is chondrified and ossified, or ossified directly, to form the skull. The relationship between the developing skull and the underlying dura mater continues during postnatal life while the bones of the calvaria are still growing. Growth of the cranial vault is initiated from ossification centres within the desmocranial mesenchyme. A wave of osteodifferentiation moves radially outward from these centres, stopping when adjacent bones meet at regions where sutures are induced to form. Once sutures are formed, a second phase of development occurs in which growth of the cranial bones occurs at the sutural margins. A number of hypotheses have been generated to explain the process of suture morphogenesis. It has been suggested that the dura mater contains fibre tracts that extend from fixed positions in the cranial base to sites of dural reflection underlying each of the cranial sutures, and the tensional forces so generated dictate the position of the sutures and locally inhibit precocious ossification. Other hypotheses support the concept of local factors in the calvaria that regulate suture morphogenesis. Following removal of the entire calvaria, the skull regenerates and sutures and bones develop in anatomically correct positions, suggesting that the dura can dictate suture position at least in regeneration of the neonatal calvaria. In transplants of sutures in which the fetal dura mater was left intact, a continuous fibrous suture remained between developing vault bones, whereas in transplants in which the fetal dura mater was removed, bony fusion occurred (Opperman et al 1993). The presence of fetal dura is not required for initial suture morphogenesis, which appears to be controlled by mesenchymal cell proliferation and fibrous extracellular matrix synthesis induced by overlapping of the advancing osteoinductive fronts of the calvarial bones. It is thought that following overlap of the bone fronts, a signal is transferred to the underlying dura that induces changes in localized regions beneath the sutures. Once a suture has formed, it serves as a primary site for cranial bone growth, but constant interaction with the dura is required to avoid ossiferous obliteration. The internal carotid artery is formed progressively from the third arch artery, the dorsal aorta cranial to this and a further forward continuation that differentiates, at the time of regression of the first and second aortic arches, from the capillary plexus extending to the walls of the forebrain and midbrain. At its anterior extremity this primitive internal carotid artery divides into cranial and caudal divisions. The former terminates as the primitive olfactory artery and supplies the developing regions implied. The latter sweeps caudally to reach the ventral aspect of the midbrain; its terminal branches are the primitive mesencephalic arteries. Simultaneously, bilateral longitudinal channels differentiate along the ventral surface of the hindbrain from a plexus fed by intersegmental and transitory presegmental branches of the dorsal aorta and its forward continuation. The most important of the presegmental branches is closely related to the fifth nerve, the primitive trigeminal artery. The longitudinal channels later connect cranially with the caudal divisions of the internal carotid arteries (each of which gives rise to an anterior choroidal artery supplying branches to the diencephalon, including the telae choroideae and midbrain) and caudally with the vertebral arteries through the first cervical intersegmental arteries. Fusion of the longitudinal channels results in formation of the basilar artery, and the caudal division of the internal carotid artery becomes the posterior communicating artery and the stem of the posterior cerebral artery. The remainder of the posterior cerebral artery develops comparatively late, probably from the stem of the posterior choroidal artery, which is annexed by the caudally expanding cerebral hemisphere; its distal portion becomes a choroidal branch of the posterior cerebral artery. The posterior choroidal artery supplies the tela choroidea at the future temporal end of the choroidal fissure; its rami advance through the tela to become confluent with branches of the anterior choroidal artery. The cranial division of the internal carotid artery gives rise to anterior choroidal, middle cerebral and anterior cerebral arteries. The stem of the primitive olfactory artery remains as a small medial striate branch of the anterior cerebral artery. The cerebellar arteries, of which the superior is the first to differentiate, emerge from the capillary plexus on the wall of the rhombencephalon. The source of the blood supply to the territory of the trigeminal nerve varies at different stages of development. When the first and second aortic arch arteries begin to regress, the supply to the corresponding arches is derived from a transient ventral pharyngeal artery that grows from the aortic sac. An anular network of meningeal arteries originates, mainly from each middle cerebral artery, and passes over each developing cerebral hemisphere. The further development of the telencephalon somewhat obscures this early pattern over the cerebrum. The meningeal arteries so formed have been classified into three groups: paramedian, short circumferential and long circumferential arteries.
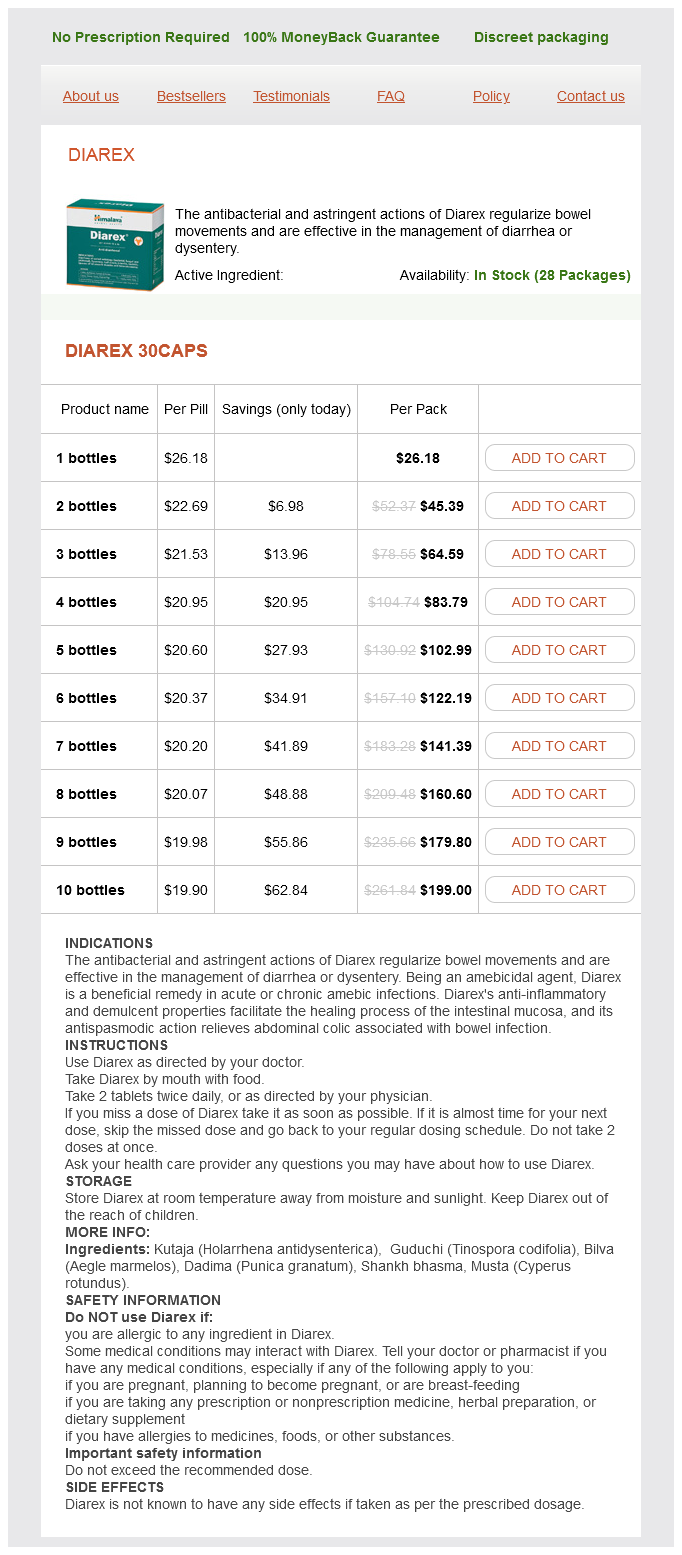
Diarex Dosage and Price
Diarex 30caps
- 1 bottles - $26.18
- 2 bottles - $45.39
- 3 bottles - $64.59
- 4 bottles - $83.79
- 5 bottles - $102.99
- 6 bottles - $122.19
- 7 bottles - $141.39
- 8 bottles - $160.60
- 9 bottles - $179.80
- 10 bottles - $199.00
The disease is clearly not confined to the cerebellar proprioceptive pathways acute gastritis symptoms uk diarex 30 caps fast delivery, given the widespread clinical deficits such as areflexia, extensor plantar responses, optic atrophy and occasional deafness, along with non-neurological issues such as scoliosis, pes cavus and cardiomyopathy. Myelin sheathstained section of spinal cord demonstrates marked symmetric degeneration in the posterior columns (solid arrow), with less prominent changes in the corticospinal tracts (dashed arrow). The tract begins in the upper lumbar region and ascends through the medulla oblongata to reach the upper pontine level; it then descends in the dorsal part of the superior cerebellar peduncle and terminates, mainly contralaterally, in the anterior cerebellar vermis. The spinocerebellar tracts are laminated, such that fibres from lower segments are superficial. Both tracts convey proprioceptive and exteroceptive information, but they are functionally different. The proprioceptive impulses often arise from a single muscle or from synergistic muscles acting at a common joint. Thus, the dorsal spinocerebellar tract transmits modalityspecific and space-specific information used in the fine coordination of individual limb muscles. In contrast, the cells of the ventral tract are activated monosynaptically by Ib afferents and transmit information from large receptive fields that include different segments of a limb. The ventral tract lacks subdivisions for different modalities and transmits information for the coordinated movement and posture of the entire lower limb. Proprioceptive and exteroceptive information from the upper limb travels in primary afferent fibres of the fasciculus cuneatus. These fibres end somatotopically in the accessory (external or lateral) cuneate nucleus and the adjoining part of the cuneate nucleus situated in the medulla oblongata. Cells of these nuclei give rise to the posterior external arcuate fibres that form the cuneocerebellar tract. The cuneocerebellar tract is therefore functionally allied to the dorsal spinocerebellar tract and is its upper limb equivalent. They end in the cerebellar cortex in a highly organized, somatotopic and functional pattern (Ch. Spinothalamic tracts - the spinothalamic tracts consist of second-order neurones that convey pain, temperature, coarse (non-discriminative) touch and pressure information to the somatosensory region of the thalamus. Pain and temperature fibres do so promptly, within about one segment of their origin, whereas fibres carrying other modalities may ascend for several segments before crossing. Spinothalamic fibres mostly ascend in the white matter ventrolateral to the ventral horn, partly intermingled with ascending spinoreticular fibres and descending reticulospinal fibres. Some authorities describe two spinothalamic tracts (lateral and ventral) with more or less distinct anatomical locations and functions. However, it should be noted that physiological studies in animals support the notion that these tracts are best considered a structural and functional continuum. On the basis of clinical evidence, it subserves coarse tactile and pressure modalities. A dorsolateral spinothalamic tract has been described in animals, arising mainly from lamina I neurones whose axons cross to ascend in the contralateral dorsolateral funiculus. These neurones respond maximally to noxious, mechanical and thermal cutaneous stimuli. That such a projection exists in humans is suggested by examples of clinical pain relief following dorsolateral cordotomy. There is clear somatotopic organization of the fibres in the spinothalamic tracts throughout their extent. Fibres crossing at any cord level join the deep aspect of those that have already crossed, which means that both tracts are segmentally laminated. In the midbrain, fibres in the spinal lemniscus conveying pain and temperature sensation from the lower limb extend dorsally, whereas those from the trunk and upper limb are more ventrally placed. The major spinothalamic projections in humans are to the ventral posterolateral nucleus and to the centrolateral intralaminar nucleus of the thalamus. In animal studies, about one third are localized to the upper three cervical segments, about 20% are located in lower cervical segments, 20% in the thoracic region (mostly segments T13), 20% in the lumbar region and 10% in the sacrococcygeal cord. Cell bodies giving rise to spinothalamic tract axons are predominantly contralateral. A relatively small number (10%) are ipsilateral, with the majority in the upper three cervical segments. The specificity of separate channels, which exists in the dorsal column nuclei, is absent in the laminae of the cord. Convergence of different functional types of afferent fibres onto an individual tract cell is a common feature in the cord. Lamina I cells that project to the thalamus respond maximally to noxious or thermal cutaneous stimulation and consist mainly of high-threshold units as well as some wide dynamic range units. Their receptive fields are usually small, representing a part of a digit or a small area of skin involving several digits. Lamina I spinothalamic tract neurones receive input from A and C Axon of neurone crossing in anterior white commissure to ascend in anterior spinothalamic tract. Spinothalamic tract cells in the thoracic cord display marked viscerosomatic convergence. Lamina I spinothalamic tract neurones project preferentially to the ventral posterolateral nucleus of the thalamus, with limited projections to the centrolateral and mediodorsal thalamic nuclei. In the lumbar cord their receptive fields are small or medium-sized-larger than the area of the foot but smaller than the entire leg. In the thoracic cord the fields of these laminar cells are larger and often include the entire upper limb plus part of the chest. Many of the deep dorsal column spinothalamic tract neurones in the thoracic segments receive convergent input from sympathetic afferent fibres. Specific sensory modalities mediated respectively by the two principle ascending pathways (spinothalmic and posterior columns) are labeled, as is the segmental distribution of motor fibers within the descending lateral corticospinal (pyramidal) tract. C: cervical; T: thoracic; L: lumbar; S: sacral (Modified from Brodal A: Neurological Anatomy, 2e.