Dilantin
General Information about Dilantin
Epilepsy is a neurological disorder that impacts the brain’s electrical exercise, resulting in recurrent seizures. These seizures can manifest in various forms, from transient moments of staring and confusion, to convulsions and lack of consciousness. People diagnosed with epilepsy usually face challenges of their daily lives and experience disruptions to their work, schooling, and relationships.
It is crucial to follow the prescribed dosage and any dosage adjustments really helpful by the doctor carefully. Abruptly stopping Dilantin or missing doses can result in a rebound impact, rising the danger of seizures. It can additionally be recommended to keep away from alcohol consumption while on Dilantin, as it can interfere with the medication’s effectiveness.
While Dilantin has proven to be effective in controlling seizures, it will not be suitable for everybody. People with a historical past of liver or kidney illness, coronary heart circumstances, or psychological health issues may have to be cautious while taking this treatment. Dilantin can also work together with different drugs, similar to birth control pills, anticoagulants, and some antibiotics. Therefore, it is crucial to inform your doctor about some other treatment you could be taking before starting Dilantin.
One of the most important benefits of Dilantin is that it might be used for long-term remedy. Unlike other anticonvulsants, Dilantin doesn't lose its effectiveness over time. It continues to provide relief to sufferers, even after extended use, and its dosage doesn't must be elevated continuously. This makes Dilantin a convenient and cost-effective option for long-term seizure administration.
Dilantin, also referred to as phenytoin, is a commonly prescribed anticonvulsant treatment used to regulate seizures in patients with epilepsy. This medicine has been around because the Nineteen Thirties and has proven to be efficient in decreasing the frequency and severity of seizures in those that undergo from them.
This is where Dilantin is out there in. It works by slowing down abnormal electrical activity within the mind, thereby stopping the onset of seizures and decreasing their severity. Dilantin is especially efficient in controlling partial seizures, the most common kind of epileptic seizure. It has additionally been found to be beneficial in treating tonic-clonic seizures, that are characterised by muscle contractions and loss of consciousness.
Dilantin is available in both pill and liquid forms, making it simple to administer for kids and sufferers with difficulty swallowing. The dosage is decided by several elements, similar to body weight, age, and different drugs the affected person may be taking. In the initial stages of treatment, patients are often required to bear blood checks to observe the levels of Dilantin of their system. This is as a outcome of Dilantin has a narrow therapeutic vary, which suggests a small distinction in dosage can have a big impression on its effectiveness.
In conclusion, Dilantin is a valuable medicine for sufferers affected by epilepsy. It has been the go-to treatment for controlling seizures for decades and continues to be a reliable possibility for long-term use. Dilantin’s effectiveness, convenience, and inexpensive cost make it an ideal selection for patients on the lookout for a method to handle their seizures and improve their high quality of life. If you or a loved one is battling seizures, consult a doctor to see if Dilantin may be the right choice for you. Always bear in mind to observe the dosage and any directions offered by your doctor to ensure the absolute best treatment outcome.
As with any medicine, there are potential side effects associated with Dilantin. The commonest side effects embody dizziness, drowsiness, headaches, and constipation. However, these unwanted effects are often delicate and have a tendency to go away as quickly as the physique adjusts to the medication. In uncommon cases, Dilantin could cause extra extreme unwanted side effects similar to liver injury, blood problems, and allergic reactions. Patients ought to pay attention to these potential unwanted aspect effects and seek medical attention if they experience any regarding signs.
Their exquisite specificity also makes them ideal guidance systems as carriers for cytotoxic agents (described subsequently) symptoms 0f ms best order for dilantin. Sensitive T cells die in response to complement activation; other T cells redistribute to non-lymphoid tissues and become significantly less responsive to antigenic challenge. In general, the drug is administered only twice; the first dose is infused intravenously within 2 hours before transplantation surgery, and the second is given 4 days later. The only adverse events attributable to basiliximab used in this manner are rare cases of allergic reactions and cytokine release syndrome. Daclizumab is a humanized variant of basiliximab in which the murine (mouse) content of the antibody has been reduced to 10%. A one-time five-dose regimen is used, with the first dose given within 24 hours before transplantation surgery and subsequent doses every 14 days thereafter. Few adverse reactions have been reported for this use of daclizumab; it apparently does not cause cytokine release syndrome. Immunotoxins have also been explored for their potential in cancer immunotherapy (including metastatic melanoma; colorectal, ovarian, and breast carcinomas; non-Hodgkin lymphoma; Hodgkin disease; B cell leukemia; and T cell lymphoma) and immunosuppression in steroid-resistant graft-versus-host disease. Although immunotoxins have been called "magic bullets" capable of pinpoint target destruction, it has become clear that most of these "bullets" are not as accurate as desired and have significant side effects, including vascular leak syndrome, myalgia, aphasia, paresthesia, encephalopathy, neuropathy, thrombocytopenia, liver destruction, renal insufficiency, proteinuria, hypoalbuminemia, dyspnea, hematuria, and tremors. The toxins themselves have proved quite antigenic, eliciting immune reactions in most cases. Immunotoxins have not been explored extensively as therapeutic agents delivered locally in the oral cavity. The syndrome usually begins within 30 minutes of drug injection, lasts for hours, and rarely may produce life-threatening cardiovascular and pulmonary disturbances. Radioimmunotherapy relies on a similar strategy to deliver radioactive substances in a selective manner for diagnostic or therapeutic purposes. In this case, the potential for tissue damage by the toxin has been replaced by the potential for radiation injury. Inasmuch as several radioimmunotherapeutic agents have been approved for human use, the tradeoff seems favorable. Tiuxetan contains a high-affinity binding site that can accommodate either indium-111 (used for diagnostic imaging) or yttrium-90 (used for target cell destruction). Infection, hemorrhage, allergic reactions, and new malignancies are potentially life-threatening reactions. Chemolabeled monoclonal antibodies constitute a third strategy for targeting therapeutic agents using monoclonal antibodies. In this case a substance that is not inherently toxic is directed to a specific site where it can produce the desired therapeutic effect. It now seems likely that the early promise to therapeutics represented by the concept of monoclonal antibodies will soon be realized. Cyclosporine, the first of these agents to gain approval for human use, revolutionized the field of organ transplantation. The cyclosporinecyclophylin complex interacts with calcineurin, a Ca++-dependent protein phosphatase. Already, monoclonal antibodies constitute the most widely used form of cancer immunotherapy. Cyclosporine is commonly used as an immunosuppressive agent to promote graft survival. It has proved successful in preventing rejections of non-matched kidney, liver, heart, heart-lung, bone marrow, and pancreas transplants. The first-year survival of liver transplants increased from 35% to 70% after the introduction of cyclosporine. Cyclosporine is also effective as a topical agent in the treatment of oral lichen planus, and it has been used systemically to treat other autoimmune diseases that may affect oral (bullous pemphigoid, pemphigus) and non-oral (psoriasis, rheumatoid arthritis) tissues. Cyclosporine has proved effective in the treatment of Behçet syndrome (a vasculitis that almost always includes oral aphthous ulcers and uveitis), nephrotic syndrome, inflammatory bowel disease, atopic dermatitis, and endogenous uveitis. The two major adverse side effects associated with long-term use are (1) dose-related renal toxicity, which, including mild forms, may occur in 75% of patients, and (2) hypertension, which is not apparently dose related and occurs in 50% of all renal transplant patients (and is especially common in children). Other side effects include central nervous system toxicity (headache, confusion, depression, seizures), gingival hyperplasia, hirsutism, mild tremor, and hepatotoxicity. A topical form of cyclosporine is available to promote tear production in patients with dry eyes due to keratoconjunctivitis sicca. The precise mechanism of cyclosporine-induced gingival hyperplasia is unknown; corrective procedures involve mainly drug titration and surgical intervention. Some studies indicate that cyclosporine therapy results in the selection of fibroblasts with cyclosporine receptors, and it has been proposed that there is an associated immunologic cytokine imbalance. Because interstitial fibrosis of the kidney has been associated with sustained high concentrations of cyclosporine, monitoring of plasma cyclosporine concentrations is necessary. A microemulsion form offers higher and more reliable absorption than the original product. Nonsteroidal antiinflammatory drugs, aminoglycosides, and other drugs that cause nephrotoxicity are contraindicated in patients receiving cyclosporine. Tacrolimus Tacrolimus is a macrolide antibiotic originally isolated from Streptomyces tsukubaensis. The resulting tacrolimusimmunophilin complex produces the same action and effects as described for cyclosporine. Tacrolimus is approved for prophylaxis against rejection of allogeneic liver transplants. Tacrolimus has been shown to exert profound antipsoriatic effects, probably by direct interaction with keratinocytes. Adverse effects of tacrolimus are qualitatively similar to those of cyclosporine except that gingival overgrowth and hirsutism are not observed. Tacrolimus ointment is a nonsteroidal topical immunomodulator used specially to treat atopic dermatitis.
Anticonvulsant Seizures that may require acute medical intervention may be associated with epilepsy symptoms of colon cancer cheap dilantin 100 mg, hyperventilation episodes, cerebrovascular accidents, hypoglycemic reactions, or vasodepressor syncope. Local anesthetic overdoses or accidental intravascular injection may also require the administration of an anticonvulsant. Current management of a seizure that interferes with ventilation or persists for longer than 5 minutes includes intravenous or intramuscular administration of benzodiazepines such as midazolam or diazepam. Glucose Glucose preparations are used to treat hypoglycemia that results either from fasting or insulin/carbohydrate imbalance in a patient with diabetes mellitus. Treatment may include commercially available oral glucose that can be placed in the buccal fold or other sources such as orange juice, a chocolate bar, cake icing, or carbonated glucose-containing soft drinks, which act rapidly to restore circulating blood glucose. If the patient is unconscious and acute hypoglycemia is suspected, intravenous administration of 50% dextrose solution or intravenous or intramuscular administration of glucagon (which increases blood glucose by its effects on liver glycogen) is the treatment of choice. The Corticosteroid Corticosteroids are used in the definitive management of acute allergic reactions and acute adrenal insufficiency. Even though the onset of even an intravenous corticosteroid, such as hydrocortisone sodium, is delayed, the drug can be useful in halting the progression of a major allergic or anaphylactoid reaction. The dentist may encounter what initially appears to be a syncopal episode but is actually the more serious problem of acute adrenal insufficiency in a patient taking longterm systemic corticosteroids to treat a chronic medical condition or a patient with primary adrenal insufficiency. In patients with myocardial ischemia and hypoxia, atropine should be used carefully because it increases oxygen demand of the heart and can worsen ischemia. Included in this training is the use of many antiarrhythmic and vasoactive drugs (Table 41-7). State regulations should be consulted to determine which of the drugs described here must be available in locations where sedation or anesthesia is administered. Additionally, there is increased emphasis on searching for and addressing the cause of the cardiac arrest. Drug therapy may be administered via intravenous, intraosseous, and endotracheal routes. Non-shockable pulseless arrest rhythms include asystole and pulseless electrical activity. Symptomatic bradycardia is defined as a heart rate less than 60 beats/min combined with symptoms such as hypotension, altered mental status, chest pain, syncope, or other signs of shock. Symptomatic tachycardia is defined as a heart rate greater than 100 beats/min combined with symptoms of shock. Treatment for stable patients is based on the classification of the rhythm into narrow-complex or wide-complex tachycardia. Vagal maneuvers, administration of adenosine, or administration of second-line drugs such as calcium channel blockers or blockers may be considered. Adenosine is recommended for wide-complex tachycardias that are believed to be supraventricular tachycardia. Vasopressin Norepinephrine Dopamine Dobutamine Isoproterenol Digoxin Inamrinone Milrinone Vasodilators/Antihypertensives Nitroprusside Hypertension, acute heart failure Nitroglycerin Hypertension, acute heart failure, angina pain Others Sodium bicarbonate Morphine Furosemide Thrombolytic agents. Amiodarone is a complex drug that acts on Na+, K+, and Ca++ channels and has -adrenergicblocking and -adrenergicblocking properties. In the emergency setting, it is administered as an intravenous bolus of 150 mg over 10 minutes followed by an initial maintenance infusion of 1 mg/min. Diltiazem is used for the same indications, but it seems to produce less myocardial depression than verapamil. Because of its narrow safety margin, digitalis has been largely superseded by Ca++ channel blockers and blockers to manage acute atrial fibrillation. Atropine inhibits cholinergic responses that decrease heart rate and systemic vascular resistance and is used to increase heart rate during periods of symptomatic sinus bradycardia resulting from excessive parasympathetic nervous system activity. Because atropine can increase myocardial oxygen demand, precipitate tachyarrhythmias, and expand the zone of infarction, it must be used carefully in patients with presumptive myocardial infarction. Typical infusions include epinephrine, dopamine, dobutamine, phenylephrine, norepinephrine, or vasopressin. These drugs are also used to control the ventricular rate in the presence of atrial tachyarrhythmias. Adverse effects of -adrenergic blockers relate to their actions on the cardiac conduction system and exacerbation of bronchospasm in patients with preexisting lung disease. Note: Amiodarone, lidocaine and magnesium can be administered by intraosseous administration in certain circumstances. This drug may cause severe hypotension when administered to a hypovolemic patient. Sodium nitroprusside is an extremely potent, rapidly acting, direct peripheral vasodilator. Vasoactive drugs In the absence of adequate circulation, vasoconstricting drugs such as catecholamines or vasopressin may enhance organ perfusion by increasing arterial and aortic pressures, resulting in desirable increases in cerebral and coronary perfusion pressures, while reducing blood flow to visceral and muscle tissues. Indications for their use include ischemic heart disease, acute heart failure, cardiogenic shock, and cardiac arrest. Vasopressin causes peripheral vasoconstriction by stimulation of vasopressin receptors located in skin and skeletal muscle and vasopressin receptors located in the mesenteric circulation, resulting in shunting of blood to vital organs. Hypotensive patients may require a continuous infusion of a powerful inotrope or vasopressor for hemodynamic support. Norepinephrine is indicated in patients with low peripheral resistance and severe hypotension.
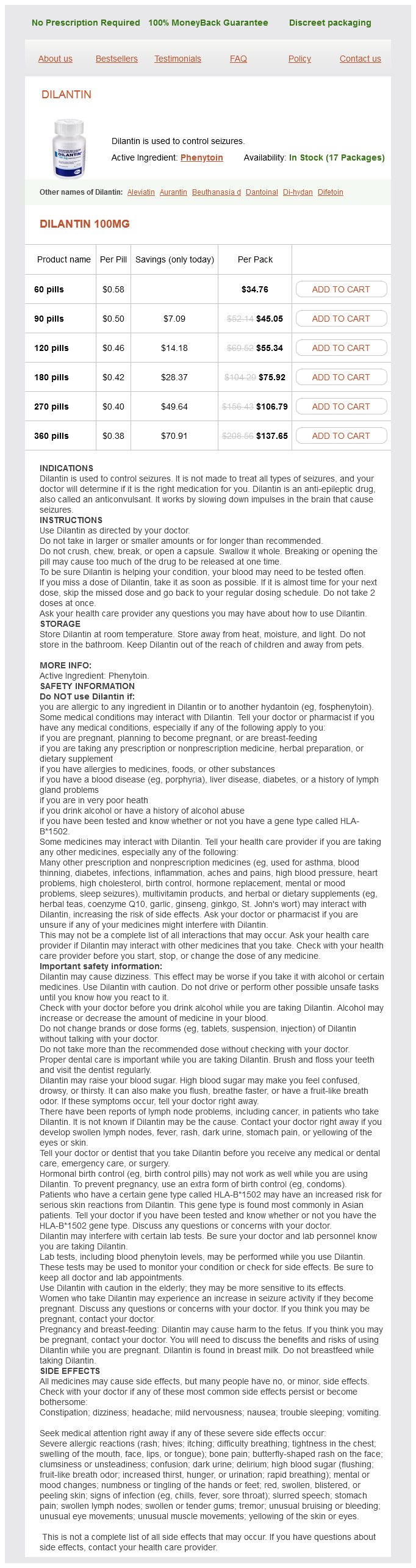
Dilantin Dosage and Price
Dilantin 100mg
- 60 pills - $34.76
- 90 pills - $45.05
- 120 pills - $55.34
- 180 pills - $75.92
- 270 pills - $106.79
- 360 pills - $137.65
Less frequent adverse effects are headache treatment 5th disease dilantin 100 mg without prescription, dizziness, anemia, rash, eosinophilia, and leukopenia. Gemfibrozil may also enhance the action of oral anticoagulants and may cause cholelithiasis. Fenofibrate is the first of the second-generation fibric acid derivatives to be tested in the United States. Side effects include the gastrointestinal disturbances common to all fibrates and the potential for causing cholelithiasis. Bile Acid Sequestrants Bile acid sequestrants are nonabsorbable anion exchange resins that bind bile acids in the intestinal lumen, prevent their reabsorption, and promote their excretion in the feces. Enterohepatic cycling of cholesterol is markedly reduced by this mechanism, which blocks reabsorption of bile acids from the jejunum and ileum, 90% of which are normally reabsorbed. Bile acids are synthesized in the liver from cholesterol by 7-hydroxylase, which is regulated through negative feedback by bile acids. Cholestyramine, colestipol, and colesevelam are the three clinically available drugs in this category. Cl- is released from the resin as bile acids bind to it, and the released Cl- is absorbed, but the resin itself is not absorbed. Because it is not absorbed, it has a high safety factor and absence of serious side effects, but the annoying gastrointestinal side effects (nausea, vomiting, abdominal distention, and constipation) limit the use of these drugs. Because these drugs exchange Cl- for other anions, hyperchloremic acidosis may develop when large doses are given to small patients. These resins also bind to anionic drugs in the intestine and decrease their absorption and their therapeutic effects. The newest bile acid sequestrant to be approved for use in the United States is colesevelam hydrochloride, which is available in tablet form. There are also somewhat fewer gastrointestinal side effects, and compliance is greater because of the tablet form. Nicotinic Acid Nicotinic acid (niacin) has been recognized since the late 1930s as a member of the vitamin B complex whose deficiency results in the disease pellagra. The action of niacin as a lipid-lowering drug is not related to its function as a vitamin. Nicotinamide, although interchangeable with nicotinic acid as vitamin B3, has no effect on plasma lipids and should not be used. It has been used alone or in combination with other lipid-lowering drugs primarily in patients with extremely high cardiovascular risk. Nicotinic acid has the broadest spectrum of activity of the lipid-lowering agents and is potentially useful in most forms of hyperlipidemia. The major disadvantage of nicotinic acid, which affects 50% or more of the patient population, has been its tendency to produce cutaneous flushing, pruritus, and gastrointestinal distress. An additional side effect in some diabetic patients is increased insulin resistance and hyperglycemia. Extended-release preparations of nicotinic acid marketed in the past few years have made this drug more tolerable to many patients, but they do not eliminate flushing in all patients. Nicotinic acid is absorbed rapidly, usually reaching a peak plasma concentration in less than 1 hour. The short half-life is primarily due to rapid excretion of unmetabolized nicotinic acid by the kidneys; this necessitates frequent administration of the drug, usually three times a day with meals. Because of the frequent lack of tolerance, doses are started at 100 mg three times per day and are gradually increased at 100-mg intervals until a dose of 1 to 1. Extended-release preparations are taken once each day, in the evening, and can be started at a higher dose. This class of drugs, called the statins, currently includes lovastatin, pravastatin, simvastatin, fluvastatin, atorva statin, rosuvastatin, and pitavastatin. Lomitapide inhibits the microsomal triglyceride transfer protein, thus inhibiting ApoB-100-containing lipoprotein production. Preliminary results suggest that they are effective in all patients including patients with homozygous familial hypercholesterolemia and those who have not responded to previous statin therapy. The incidence varies among the different agents, with blurred vision more frequent with lovastatin and pravastatin and impotence and insomnia more frequent with lovastatin. Lovastatin has been linked with severe myopathy (rhabdomyolysis) when administered in combination with erythromycin, cyclosporine, gemfibrozil, or nicotinic acid. Cerivastatin was removed from the market by its manufacturer because of rhabdomyolysis. Another side effect of statins that may be important in some patients is the potential for reduction in ubiquinone levels. Statins are rated category X in pregnancy, so they should be discontinued prior to conception. Data on the ability of these drugs to reduce cardiac Other Drugs for Homozygous Familial Hyperlipidemia Patients with homozygous familial hyperlipidemia develop coronary heart disease and may have heart attacks at a very early age (before puberty). Two drugs that decrease the ability of cells to synthesize and secrete lipoproteins have been approved for use in these patients. This oligonucleotide is synthesized with a modified structure that allows it to avoid metabolism by nucleases. It is administered weekly by injection and accumulates in the liver, where it has its major action to block lipoprotein secretion.