Duetact
General Information about Duetact
Duetact comes in pill type and is typically taken once a day, with or with out food. Dosage could differ relying on a affected person's particular person needs and response to the medicine.
In conclusion, Duetact is an effective treatment for the treatment of kind 2 diabetes. It combines the benefits of two active components, pioglitazone and glimepiride, to help management blood sugar ranges in patients with diabetes. Although it might trigger unwanted effects in some sufferers, the benefits of Duetact can tremendously enhance the standard of life for those battling sort 2 diabetes. If you've been identified with type 2 diabetes or are experiencing symptoms of excessive blood sugar, make positive to seek the advice of with your physician to see if Duetact is the right treatment possibility for you.
Pioglitazone is a member of the thiazolidinedione (TZD) class of medications. It works by increasing the body's sensitivity to insulin, the hormone that controls blood sugar levels. This helps the body to make use of insulin extra effectively and reduces the amount of glucose that's produced by the liver. Pioglitazone also reduces irritation in the body, which is a typical problem in patients with kind 2 diabetes.
Duetact is primarily used for patients who have not been capable of attain adequate control of their diabetes with diet and exercise alone. It can be generally prescribed for patients who haven't responded well to other medicines, corresponding to metformin or sulfonylureas.
In addition to taking Duetact, it is important for sufferers to maintain a wholesome lifestyle by consuming a balanced food regimen, partaking in common physical activity, and monitoring their blood sugar levels often. Patients also needs to comply with up with their physician regularly to monitor their progress and make any essential changes to their therapy plan.
Duetact, also identified by its generic name pioglitazone and glimepiride, is a medication commonly prescribed for the treatment of sort 2 diabetes. It is a mixture of two active elements, pioglitazone and glimepiride, which work collectively to help management blood sugar levels in patients with diabetes.
When taken together, pioglitazone and glimepiride work synergistically to regulate blood sugar ranges in patients with type 2 diabetes. This is very beneficial for patients who have not been able to achieve sufficient blood sugar control with different drugs.
Like another medicine, Duetact may trigger unwanted side effects in some patients. The most common unwanted effects reported include weight acquire, edema, and complications. In uncommon cases, Duetact may trigger critical side effects such as liver problems, heart failure, and bone fractures. It is essential for patients to discuss any potential danger factors with their physician before starting this treatment.
Glimepiride belongs to a class of medicines known as sulfonylureas. It works by stimulating the pancreas to supply extra insulin, serving to to manage high blood sugar levels in patients with diabetes. Glimepiride additionally helps the physique to use insulin extra effectively, just like pioglitazone.
Before prescribing Duetact, docs will keep in mind a patient's medical historical past, current drugs, and any potential dangers. This treatment will not be suitable for sufferers with heart problems, liver illness, or kidney illness, in addition to those that are pregnant or breastfeeding.
Microvesicular fat deposition can be missed if the tissue is fixed before examination diabetes symptoms hypoglycemia best 16 mg duetact, and Oil Red 0 or Sudan stains should be used on frozen tissue sections. Intrahepatic cholestasis is usual and, unlike in preeclampsia, cellular infiltration with lymphocytes is minimal. Due to decreased ammonia utilization by the urea cycle enzymes of the hepatocytes, serum ammonia is elevated, and associated with hepatic encephalopathy. Transaminase elevation is mild to moderate, usually less than 250 to 500 U/mL, but can be greater than 1000 U/mL. An elevated serum creatinine has been documented in some patients before the development of liver failure, although renal insufficiency may not be due to hepatorenal syndrome as has been postulated. Pancreatitis, associated with microvesicular fat deposition in the pancreas, results in elevated amylase and lipase in some patients. It has been proposed that more than 6 of 15 criteria must be present to make the diagnosis. There are some other drawbacks to these criteria, which include the inability of the criteria to aid in earlier diagnosis. Additionally, the criteria are not standardized among researchers; some have used 9 versus 6 criteria for diagnosis. Swansea Criteria for Diagnosis of Acute Fatty Uver Disease Vomiting Abdominal pain Polydlpsla/polyuria Enoephalopathy Blllrubln >0. Features in common to these entities include elevated transaminases, thrombocytopenia, and frequently, an elevated serum creatinine. Risk factors may be identified for hepatitis, including drug exposure or known hepatitis exposure. There is no clear benefit to immediate cesarean versus vaginal delivery with meticulous supportive care. However, factors such as known fetal growth restriction and uteroplacental insufficiency, nonreassuring fetal status by fetal heart rate monitoring, and early gestational age with a markedly unfavorable cervix should influence a decision to choose cesarean section over vaginal delivery. Coagulation parameters should be corrected prior to surgical delivery, and consideration given to a vertical midline incision, avoiding the dissection associated with a Pfannenstiel incision. The use of an intraperitoneal, closed suction drain, as well as a similar subcutaneous drain (or delayed secondary closure) can also be considered. If vaginal delivery can be accomplished, avoidance of episiotomy in the presence of a coagulopathy is suggested. Anesthesia should be carefully planned, and regional anesthesia considered if coagulation abnormalities can be corrected. If not and general anesthesia is chosen; inhalation agents with the potential for hepatotoxicity (such as halothane) should be avoided. In addition, the dose of narcotics, which are metabolized by the liver, should be adjusted. Worsening of liver and renal function can be seen for up to 2 to 3 days after delivery, as well as the development of pancreatitis. Additional therapies which have been reported empirically in very small numbers of patients with uncertain benefit have included plasma exchange and albumin dialysis. Plasma exchange was used for 6 patients who continued to worsen from 2 to 9 days after delivery. Although there are several reported cases of liver transplantation for patients with ongoing liver failure in the immediate postpartum period, it has been argued that with ongoing supportive care, all surviving patients will ultimately experience complete resolution of liver failure. Management Cornerstones for Acute Fatty Uver of Pregnancy by Affected System based on 28 consecutive cases. How accurate are the Swansea criteria to diagnose acute fatty liver of pregnancy in predicting hepatic microvesicular steatosis~ Gut. Acute fatty liver of pregnancy: an update on pathogenesis and clinical implications. Prenatal predictors in postpartum recovery for acute fatty liver of pregnancy: experiences at a tertiary referral center. Acute fatty liver of pregnancy associated with pancreatitis: a life threatening complication. Liver injury in acute fatty liver of pregnancy: possible link to placental mitochondrial dysfunction and oxidative stress. Acute fatty liver of pregnancy: an experience in the diagnosis and management of fourteen cases. Prospective screening for pediatric mitochondrial trifunctional protein defects in pregnancies complicated by liver disease. This page intentionally left blank Neurologic Emergencies During Pregnancy · Loralei L. Pregnancy physiology and concern for the fetus can additionally makt the evaluation and treatment more complex because ofchanging maternal physiology. The focus will be on acute, life-threatening events as opposed to the management of known chronic neurological conditions. Using this approach will provide a more "real life" approach-one of evaluating the pregnant women with a complaint and moving forward to a diagnosis. Care should not be delayed to the mother for fetal evaluation or delivery, but often fetal evaluation including monitoring and ultrasound can be accomplished simultaneously and provide valuable clinical information to aid in decision making. However, the utilization of gadolinium contrast may be justified depending on the diagnosis in questions and if the benefits outweigh the risks of exposure. However, a large study of first trimester exposure to date did not show an increased risk for congenital anomalies or stillbirth with exposure in the first trimester, but did show an increased risk for rheumatologic/inflammatory conditions, stillbirth, and neonatal death with exposures in any trimester, suggesting that later exposures may be risker.
Accurate discernment requires careful attention to physical examination does diabetes in dogs cause hair loss order duetact on line amex, timing of symptoms, and associated laboratory abnormalities. Pregnancy is associated with a higher incidence of bladder infections and pyelonephritis. Increased incidents of upper and lower urinary tract infections, estimated to complicate approximately 2% of all pregnancies, are believed to result from hormonal and mechanical changes that result in stasis (category 3) within the urinary collecting system. Moreover, aminoglycoside antibiotics, not infrequently used for treating pyelonephritis, may further compromise renal function. Urine output is usually at its lowest during this phase, which typically lasts 1 to 2 weeks, although it may persist up to 11 months, depending on etiology. The recovery phase is frequently accompanied by marked diuresis that results in profound electrolyte disturbances, unless closely monitored and corrected Whereas some patients with preeclampsia/ eclampsia-induced A1N may temporarily require dialytic support, even these patients usually experience complete recovery and have excellent long-term prognoses. As the name suggests, it is a complication which partially or completely destroys the renal cortex while sparing the medulla. Renal cortical necrosis is heralded by abrupt onset of oliguria or anuria, sometimes accompanied by flank pain, gross hematuria, and hypotension. The triad of anuria, gross hematuria, and flank pain is unusual in other causes of renal failure in pregnancy. Characteristic imaging findings include hypoechoic and/or hypodense areas in the renal cortex. No specific therapy has been uniformly effective for renal cortical necrosis; many women require chronic hemodialysis, although approximately from 30% to 40% of patients will experience partial recovery. Although tranexamic acid is sometimes used to manage obstetric hemorrhage and to reduce risk of subsequent development of renal cortical necrosis, published data has not been supportive. Some investigators group these disease processes, including preeclampsia/ eclampsia, under the rubric of "microangiopathic hemolytic processes of pregnancy," because they share common features of maternal anemia with evidence of red blood cell destruction on peripheral smears. Clinical manifestations and nomenclature of a given disease reflect primary target organs, although they appear to share a common pathophysiologic process which involves profound arteriolar vasoconstriction due to unidentified processes which likely involve maternal vascular endothelium. Hypovolemia caused by hemorrhage, for example, is ideally corrected with packed red blood cells. Accordingly, isotonic saline is usually appropriate replacement for plasma losses. Pulmonary artery catheterization has been advocated as an alternative to tailoring fluid management in these patients, as central venous pressure is often inaccurate in this situation. But this modality has largely fallen out of favor, as the risk outweighs the benefits with many acute disease processes. Additionally, measurements of urinary indices may not accurately reflect volume status of the patient. The single most important factor in management of intrinsic renal azotemia is optimization of both cardiovascular function and intravascular volume. In certain instances, insulin and glucose replacement may be necessary to manage hyperkalemia. Alternative therapies include sodium polystyrene sulfonate (Kayexalate), orally or as an enema; also, dialysis may sometimes be considered. Dialysis has been shown to decrease maternal mortality and accelerate recovery of renal function. For women requiring dialysis for renal failure during gestation, reported pregnancy outcomes have been generally poor. Counseling women with end-stage renal disease, whether pregnant or considering pregnancy is critically important. Within this context, it is worth noting that: · One report found that only 15% of women had return to baseline renal function 6 months postpregnancy termination. There was no difference in outcome between women receiving hemodialysis versus peritoneal dialysis, although the investigators advised against switching from one modality to another during pregnancy. If improvement is not noted after several treatments of plasma exchange, use of anticomplementdirected monoclonal antibodies (eculizumab) may be indicated. Renal biopsy is valuable when indicated in nonpregnant patients, where it plays a critical role in establishing specific renal pathology. However, renal biopsy during pregnancy risks significant complications, particularly with thrombocytopenic mothers; normally increased pregnancy-associated blood flow to the kidneys compounds the risk. Pregnancy-associated hemolytic uremic syndrome revisited in the era of complement gene mutations. Urinary diagnostic indices in preeclampsia-associated oliguria: correlation with invasive hemodynamic monitoring. Renal hemodynamics in normal and hypertensive pregnancy: lessons from micropuncture. Effect of hypotonic expansion on sodiwn, water and urea excretion in late pregnancy: the influence of posture on these results. Pregnancy related acute kidney injury: a single center experience from the Kashmir Valley. The first case New proposed diagnostic criteria fur the case definition of report of. Approximate maternal fatality rate and based studies ha:ve reported a decreased case fatality rate perinatal mortality associated with. Sudden onset of cardiorespiratory arrest, or both hypotension (systolic blood pressure <90 mmHg) and respiratory compromise (dyspnea, cyanosis, or peripheral capillary oxygen saturation [Sp02] <90%) 2. Coaguloapthy must be detected prior to loss of sufficient blood to itself account for dilutional or shock-related consumptive coagulopathy 4. Proposed diagnostic crtterta for the case definition of amniotic ftuld embolism In research studies.
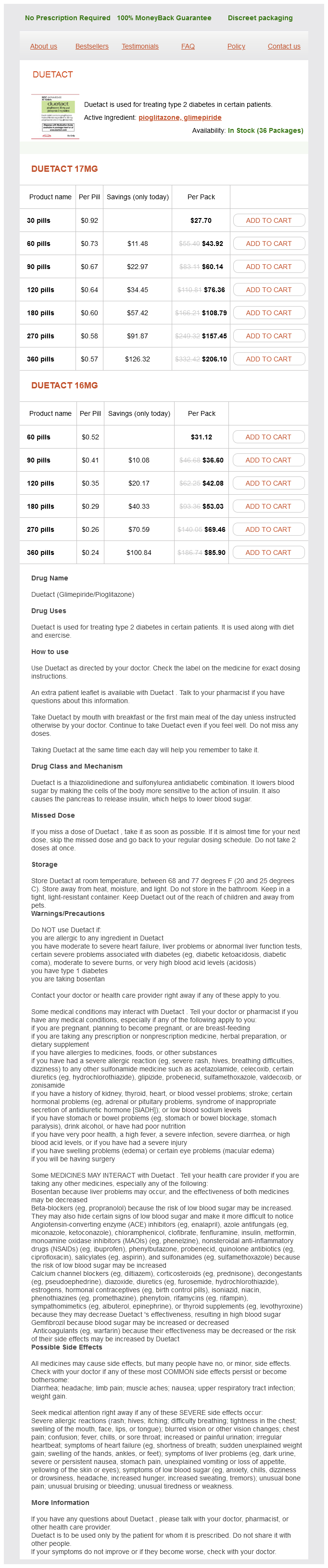
Duetact Dosage and Price
Duetact 17mg
- 30 pills - $27.70
- 60 pills - $43.92
- 90 pills - $60.14
- 120 pills - $76.36
- 180 pills - $108.79
- 270 pills - $157.45
- 360 pills - $206.10
Duetact 16mg
- 60 pills - $31.12
- 90 pills - $36.60
- 120 pills - $42.08
- 180 pills - $53.03
- 270 pills - $69.46
- 360 pills - $85.90
With the sympathetic-induced lipolytic metabolism diabetic diet quiz 16 mg duetact with mastercard, increases in free fatty acids and lactate produce relative maternal acidosis. Increased sympathetic activity increases metabolism and oxygen consumption, and decreases gastrointestinal and urinary bladder motility. Diminished PaC02 levels below 25 to 27 mm Hg may result in increased uteroplacental resistance and reduced oxygen delivery to the fetus. During peak contractions, there is a reduction in intervillous blood flow leading to a significant decrease in placental gas exchange. This exaggerates the already dramatic reduction in uterine blood flow, secondary to the increases in norepinephrine and cortisol (see Table 20-1). Cautious epidural analgesia has been reported to provide a vasomotor blocking effect that increases intervillous blood flow and oxygen delivery to the fetus. The first stage of labor refers to the beginning of cervical dilation and effacement until its completion. The second stage of labor extends from complete cervical dilation until delivery of the infant. It is important for the care provider to understand the differences between the pain conduction (spinal levels) during the first stage oflabor, as compared with the second and third stage, in order to provide appropriately directed analgesia. Left ventricular stroke work Fetal effects Nonnal gastrointestinal function Nonnal urinary function t Uterine blood flow More stability in fatal heart rate tracing consider that pain may also be due to the pathology of the gestation, such as abruptio placenta, infection. Only segments necessary for the spedftc pain of labor should be blocked (Table 20-3). Relatively decreased fetal perfusion has been reported to occur both in the presence and absence of overt maternal hypotension secondary to a sympathectomy-mediated reduction in uterine blood flow. These drugs prevent the development of an action potential in a nerve by blocking sodium channels responsible for propagating a Stage one T1. The uncharged state of the drug crosses the lipid nerve membrane and enters the cell. Once in the cell, it re-equilibrates into the charged form that is readily dissolved in water. This charged form now reaches the sodium channels and blocks them from inside (see Table 20-3). Ionization the capacity for an uncharged species to assume a charged form is the essential property of all local anesthetics. Uncharged (1) local anesthetic passes through the nerve membrane (2) into the cell (3) where the local anesthetic gains a W (hydrogen ion) to become charged. Innervation of Pelvlc Viscera Uterus Tubes/ovaries Broad ligament Cervix Vagina Vestibule/hymen Labia ClitOris Perineum Bladder Anus Motor fibers from parasympathetic pelvic nerves from 5 2, 5 3, 5 4, and sympathetic sensory Motor fibers from parasympathetic pelvic nerves from 5 2, 5 3, 5 4, and sympathetic sensory fibers via the ovarian plexus from T12, Li. Motor fibers from parasympathetic pelvic nerves from 5 2, 5 3, 5 4, and sympathetic sensory fibers via the hypogastric plexus from T12, L1 Motor fibers from parasympathetic pelvic nerves from 5 2, 5 3, S4, and sympathetic sensory fibers via the hypogastric plexus from T12, L1 Motor fibers from parasympathetic pelvic nerves from 5 2, 8 3, 8 4, and sympathetic sensory fibers via the hypogastric plexus from T12, L1 Erectile vasodilator fibers from parasympathetic pelvic nerves from 8 2, 8 3, 8 4 Posterior labial nerve 5 2, 8 3, and perinea! Comparative properties of lidocaine, ropivacaine, and bupivacaine are outlined in Table 20-4. The addition ofa vasoconstrictor (epinephrine) to the local anesthetic can decrease the absorption and, therefore, toxicity of the drug used (see Table 20-4). Local anesthetic bind and inhibit cardiac Na+, Ca2+, and K+ channels as concentrations increase causing cardiac arrest Treatment of adverse reactions depends on the severity oftheir effects from spontaneous recovery, t. This is produced solely as the S-enantiomer, whereas bupivacaine is a mixture of the S and R forms. This S-form has less ability to bind Nachannels in the myocardial conduction system. As seen in Table 20-4, ropivacaine and bupivacaine have very similar physical properties except for the margin of safety, in ropivacaine, which produc. There also appears to be less ofa motor block compared to bupivacaine, which theoretically should improve patient satisfaction during the laboring process. Caution has been used in administering this agent as it has several side effects that occur in a significantly high occurrence (>10% of patients). These include cardiovascular: hypotension (dose-related and age-related: 32%-69%), maternal bradycardia (6%-20%), gastrointestinal: nausea (11 %-29%), vomiting 7%-14%), and neuromuscular and skeletal: back pain (7%-10%) of patients. Lidocaine ~ 5 mg/kg · 1% lidocaine = 10 mg lidocaine/cc Maximum dose 35 cc · 2% lidocaine = 20 mg lidocaine/cc Maximum dose 17. Lidocaine with epinephrine ~ 7 mg/kg · 1% lidocaine with = 10 mg lidocaine/cc 1: 200,000 epi plus lntersplnous. Bo1il llgament 5 iig epinephrine/cc Maximum dose 49 cc · 2% lidocaine with = l: 100,000 epi 20 mg lidocaine/cc plus 10 iig epi/cc Maximum dose 24. Lumbosacral anatomy showing needle depth for epidural and subarachnold Injections. Epldural Analga&la/Anesthesia Lumbar epidural block is the most common form ofanalgemo used to provide relief from the nociceptive pathways during the stages oflabor. The epidural space is the interval superiorly bounded by the foramen magnum, inferiorly by the lower end of the dural sac, anteriorly by the posterior longitudinal ligament, and posteriorly by the ligamentum flavum. The approach to the epidural space is posteriorly through the skin, subcutaneous fat. The size of the epidural space varies along its course with the largest diameter existing at the ~ interspace with a range of 4 to 9 mm. In pregnancy, with the increase in intra-abdominal pressure, the venous plexus becomes distended. When patient Is fixed, the interlaminar space enlarges, increasing the ability to enter the eplduraljsubarachnold space.