Dulcolax
General Information about Dulcolax
Speaking of unwanted facet effects, it is crucial to concentrate on the potential antagonistic reactions which will occur when taking Dulcolax. The most typical aspect effect is abdominal discomfort, which may vary from gentle cramping to severe ache. In some circumstances, it may possibly additionally trigger electrolyte imbalances, dehydration, and nutrient deficiencies because of excessive bowel movements. It is suggested to drink loads of water and maintain a balanced food regimen whereas taking this treatment to prevent these points. Additionally, pregnant or breastfeeding women, as well as people with certain medical situations, ought to consult their healthcare provider earlier than utilizing Dulcolax.
Stomach discomfort and irregularity can affect people of all ages and backgrounds. Bowel movement points may be attributable to a wide range of factors similar to food regimen, stress, or underlying health situations. To address this frequent problem, many people flip to over-the-counter laxatives like Dulcolax to provide relief. In this text, we'll delve into what Dulcolax is and the consequences it has on our our bodies.
Dulcolax is a well known brand of stimulant laxatives that's used to deal with constipation. It comes in numerous forms similar to tablets, suppositories, and liquid drops. The active ingredient in Dulcolax is called Bisacodyl, which acts specifically on the bowels to stimulate the muscular tissues and promote bowel motion. This medication is permitted by the Food and Drug Administration (FDA) and is well accessible with no prescription.
Stimulant laxatives like Dulcolax work by increasing the motion of intestinal muscular tissues, which helps to maneuver waste merchandise through the colon and out of the body. This results in a laxative effect that may produce bowel actions within 6 to 12 hours after taking the treatment. However, the exact time frame might differ relying on the person's metabolism and the dosage taken.
Another important level to note is that Dulcolax may interact with certain medications, together with antacids, different laxatives, and antibiotics. Therefore, it is important to tell your physician of all the medications you are taking, together with natural supplements, earlier than beginning Dulcolax.
One of the benefits of using Dulcolax is its fast-acting nature, making it an efficient possibility for those seeking immediate reduction from constipation or irregular bowel actions. It may also be useful for individuals who have undergone certain medical procedures that require the bowel to be empty. Dulcolax is mostly really helpful for short-term use and should not be used as a long-term solution for constipation. Long-term use of this treatment can result in dependence on laxatives and should trigger unwanted side effects.
In conclusion, Dulcolax is a widely used stimulant laxative that may successfully relieve constipation and promote bowel movement. Its fast-acting nature and straightforward accessibility make it an attractive choice for these in search of reduction from digestive issues. However, like all treatment, it is essential to make use of Dulcolax responsibly and seek the advice of a healthcare supplier in case you have any concerns or underlying well being circumstances. A healthy way of life, including a balanced diet and common train, can even assist prevent constipation and cut back the necessity for laxatives.
Delivery of gastroschisis patients before 37 weeks of gestation is associated with increased morbidities medicine 2000 generic dulcolax 5 mg with mastercard. The bowel bag: a sterile, transportable method for warming infants with skin defects. Is routine preoperative 2-dimensional echocardiography necessary for infants with esophageal atresia, omphalocele, or anorectal malformations Canadian Pediatric Surgical Network: a population-based pediatric surgery network and database for analyzing surgical birth defects. Factors affecting the outcome in patients with gastroschisis: how important is immediate repair Gastroschisis wringer clamp: a safe, simplified method for delayed primary closure. Routine insertion of a silastic spring-loaded silo for infants with gastroschisis. Method to our madness: an 18-year retrospective analysis on gastroschisis closure. The relative merits of various methods of indirect measurement of intraabdominal pressure as a guide to closure of abdominal wall defects. Prediction of successful primary closure of congenital abdominal wall defects using intraoperative measurements. Splanchnic perfusion pressure: a better predictor of safe primary closure than intraabdominal pressure in neonatal gastroschisis. Component separation for complex congenital abdominal wall defects: not just for adults anymore. Successful management of short gut due to vanishing gastroschisis-case report and review of the literature. A multicenter, randomized, double-blind, placebo-controlled trial of the prokinetic agent erythromycin in the postoperative recovery of infants with gastroschisis. Development and validation of a risk stratification index to predict death in gastroschisis. Vacuum-assisted closure: a new method for treating patients with giant omphalocele. Iatrogenic neonatal mercury poisoning from Mercurochrome treatment of a large omphalocele. Conservative management of giant omphalocele with topical povidone-iodine and its effect on thyroid function. Delayed management of giant omphalocele using silver sulfadiazine cream: an 18-year experience. Initial nonoperative management and delayed closure for treatment of giant omphaloceles. Bipedicled skin flaps for reconstruction of the abdominal wall in newborn omphalocele. Closure of giant omphaloceles by the abdominal wall component separation technique in infants. Functional, motor developmental, and long-term outcome after the component separation technique in children with giant omphalocele: a case control study. Use of surgisis for abdominal wall reconstruction in children with abdominal wall defects. The development of necrotizing enterocolitis following repair of gastroschisis: a surprisingly high incidence. Small-bowel continuity: a crucial factor in determining survival in gastroschisis. Longitudinal growth and late morbidity of survivors of gastroschisis and omphalocele. Morbidity and quality of life in adult patients with a congenital abdominal wall defect: a questionnaire survey. Cardiopulmonary performances in young children and adolescents born with large abdominal wall defects. Creation of a stoma may be required for numer ous congenital or acquired diseases of the gastrointestinal tract. Intestinal stomas are used to divert fecal flow, for decompression of the proximal bowel, to reduce stool contamination of a diseased area, to protect a tenuous anastomosis during healing, and to reduce the risk of infection, obstruction and incontinence in various com plex disorders of the gastrointestinal tract. There are considerable differences between children and adults in terms of ongoing physical and cognitive development, and these factors should be considered as part of the decisionmaking process in creation and management of stomas. Amussat described a lumbar and ventral colostomy to divert the fecal stream in a case of colorectal obstruction 100 years later. Although intestinal stomas are often used alone, they have also become an important part of some complex operations such as abdominoperineal resection. In the pediatric surgery literature, creation of a colostomy was first performed in 1783 for a patient with anal atresia. Bishop and Koop21 described a RouxenY anastomosis proximal to an end ileostomy, which allows for irrigation of the bowel segment for the treatment of meconium ileus in patients with cystic fibrosis. Kock introduced the continent ileostomy as an intraabdominal reservoir for patients who required a permanent ileostomy. There is specific stoma equipment for pediatric patients of varying types and sizes. In addi tion to advances in surgical technique, stoma appliances have also evolved.
These features are externally visible and help in the diagnosis of a perineal fistula treatment interventions purchase dulcolax 5 mg online. Less than 10% of these children have Imperforate Anus Without Fistula In imperforate anus without fistula, the rectum ends blindly, without a fistula, approximately 1 to 2 cm above the perineum, usually at the level of the bulbar urethra. These patients with very high defects have a flat bottom, no perineal groove, and frequently have a bifid scrotum. Conversely, 95% of patients with Down syndrome who have anorectal malformations have this specific type. This malformation can be repaired primarily at birth, without a colostomy, provided the surgeon has enough experience and the baby is in good condition. Although not connected to the distal rectum, the urinary tract is intimately attached to the urethra, and great care must be taken not to injure the urethra. Rectal Atresia/Stenosis In this rare defect, the patient is born with a normallooking anus externally, but an attempt to take the rectal temperature discloses an obstruction located 1 to 2 cm above the mucocutaneous junction of the anus. Associated defects are almost nonexistent except for presacral mass, which must be screened for. The prognosis is excellent, when there is no presacral mass, and 100% of these patients achieve bowel control. During surgical repair, it is important to be aware of the proximity between the rectum and vagina. After repair, patients should be screened and followed because of a high incidence of constipation. Vestibular Fistula the vestibular fistula is the most common defect in female patients. Approximately 95% of these patients achieve bowel control after surgery,1,2,14 and 30% of them have associated urologic defects. Approximately 5% have an associated gynecologic anomaly, either a vaginal septum or absence of the vagina, and a vaginoscopy is performed at the time of the planned reconstruction to assess this. Less than 10% of these children have an associated urologic defect, and gynecologic anomalies are rare. One hundred percent of patients with these defects achieve bowel control after proper treatment, provided they have a normal sacrum and no tethered cord. The prognosis varies depending on the quality of the sacrum and spine and the length of the common channel. Thirty percent of cloacas also have hydrocolpos, which is a very distended, tense, giant vagina that may compress the opening of the ureters at the trigone, provoking bilateral megaureters. At birth, these patients require the opening of a colostomy and drainage of the hydrocolpos when present. Rarely, some sort of urinary diversion is needed to address the obstructive uropathy. After 2 to 4 months of life, they undergo a complex operation during which the three main structures (the rectum, vagina, and urethra) are separated and placed in their normal location. On the other hand, a cloaca with a common channel longer than 3 cm requires not only the posterior-sagittal approach but also a laparotomy and a series of decisionmaking steps that require a significant amount of experience. The frequency of these associations varies with each defect, as has already been described. The quality of the spine and sacrum has a direct impact on the prognosis for bowel and urinary control. A very hypoplastic sacrum, absent sacrum, or associated spinal problem, such as tethered cord or myelomeningocele, correlate directly with poor fecal and urinary continence. Chapter 55 - Imperforate Anus 635 Another subgroup of patients has gastrointestinal defects, including esophageal atresia, duodenal atresia, or other kinds of atresia in the intestinal tract. Approximately 30% of all patients have some sort of cardiovascular defect, but only 10% require surgery. The other 20% usually represent patent ductus arteriosus, atrial or ventricular septal defects, or defects with no hemodynamic implications. The perineum must be meticulously evaluated, because it provides a series of clues that help to answer the second question. One should always look for the presence of a perineal fistula, which sometimes is extremely small. Does the infant need a colostomy, or can the malformation be repaired in a primary way without a colostomy The higher in the pelvis, the location of the rectum and more complex the anorectal defect, the greater the chance of a dangerous associated defect. All infants with anorectal malformations should have abdominal and pelvic ultrasound examination during the first hours of life. If the patient has any of these conditions, further urologic evaluation may be required. Prone position with the pelvis elevated and radiopaque marker at the anal impression. An ultrasound of the lower spine done in the first few days of life can rule out the presence of tethered cord, or other spinal problems that are associated with a higher type of anorectal malformation with poor prognosis. During the following 18 to 24 hours, the abdomen becomes distended and the intraluminal pressure of the bowel increases significantly, thereby forcing the meconium through the lowest part of the rectum, which is surrounded by the sphincter mechanism. One can expect that the meconium will pass through a fistula, usually after 18 to 24 hours. The golden rule in the early diagnosis of these children is to wait at least 18 to 24 hours before making a decision. A piece of gauze placed on the tip of the penis may filter the meconium when the infant voids, making the diagnosis of a rectourinary fistula, which is an indication to open a colostomy in most cases.
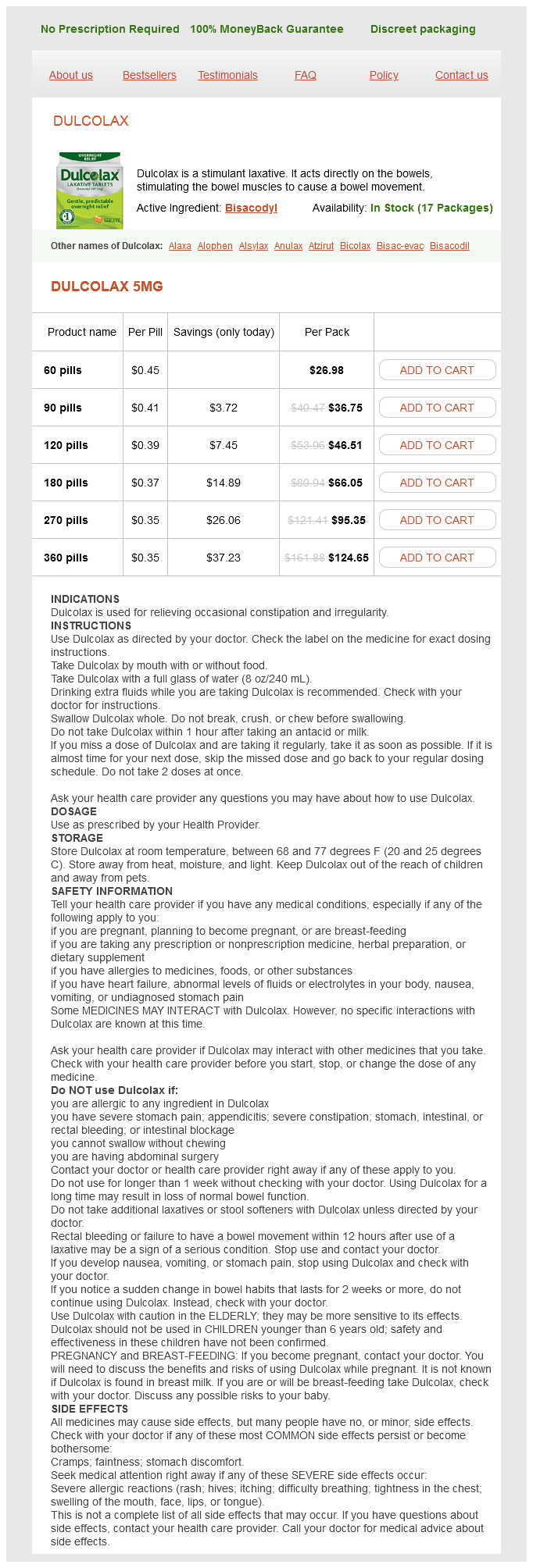
Dulcolax Dosage and Price
Dulcolax 5mg
- 60 pills - $26.98
- 90 pills - $36.75
- 120 pills - $46.51
- 180 pills - $66.05
- 270 pills - $95.35
- 360 pills - $124.65
Association of apnea and nonacid gastroesophageal reflux in infants: investigations with the intraluminal impedance technique treatment tracker buy generic dulcolax pills. Adverse outcomes associated with gastroesophageal reflux disease are rare following an apparent life-threatening event. The frequency of apneas in very preterm infants is increased after non-acid gastroesophageal reflux. Involvement of autonomic nervous activity changes in gastroesophageal reflux in neonates during sleep and wakefulness. Characteristics of gastroesophageal reflux and potential risk of gastric content aspiration in children with cystic fibrosis. Bile acids in sputum and increased airway inflammation in patients with cystic fibrosis. Children with cystic fibrosis have prolonged chemical clearance of acid reflux compared to symptomatic children without cystic fibrosis. Clinical evaluation of pepsin for laryngopharyngeal reflux in children with otitis media with effusion. Bile acids identified in middle ear effusions of children with otitis media with effusion. Correlation of findings at direct laryngoscopy and bronchoscopy with gastroesophageal reflux disease in children: a prospective study. Lack of association between esophageal biopsy, bronchoalveolar lavage, and endoscopy findings in hoarse children. Comparison of pediatric voice outcome survey, reflux symptom index, reflux finding score, and esophageal biopsy results. Proton pump inhibitor therapy for chronic laryngo-pharyngitis: a randomized placebocontrol trial. Gastroesophageal reflux disease and tooth erosion: a cross-sectional observational study. Gastroesophageal reflux, dental erosion, and halitosis in epidemiological surveys: a systematic review. The natural history of the partial thoracic stomach ("hiatal hernia") in children. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. Does the incidence of adenocarcinoma of the esophagus and gastric cardia continue to rise in the twenty-first century Challenges in the diagnosis of gastroesophageal reflux disease in infants and children. Comparison of gastroesophageal reflux disease questionnaire (GerdQ) and multi-channel intraluminal impedancepH monitoring in identifying patients with chronic cough responsive to anti-reflux therapy. The infant gastroesophageal reflux questionnaire revised: development and validation as an evaluative instrument. Infant gastroesophageal reflux disease score: reproducibility and validity in a developing country. Gastroesophageal reflux disease in infants: how much is predictable with questionnaires, pH-metry, endoscopy and histology Comparison of upper gastrointestinal contrast studies and pH/impedance tests for the diagnosis of childhood gastro-oesophageal reflux. Oesophageal mucosal intercellular space diameter and reflux pattern in childhood erosive and non-erosive reflux disease. Dilated intercellular space diameter as marker of reflux-related mucosal injury in children with chronic cough and gastro-oesophageal reflux disease. Treatment of oesophageal bile reflux in children: the results of a prospective study with omeprazole. Prognostic values of multichannel intraluminal impedance and pH monitoring in newborns with symptoms of gastroesophageal reflux disease. The sensitivity of multichannel intraluminal impedance and the pH probe in the evaluation of gastroesophageal reflux in children. The role of baseline impedance as a marker of mucosal integrity in children with gastro esophageal reflux disease. Relationship between baseline impedance levels and esophageal mucosal integrity in children with erosive and non-erosive reflux disease. Esophageal impedance baselines in infants before and after placebo and proton pump inhibitor therapy. Natural history of infant reflux esophagitis: symptoms and morphometric histology during one year without pharmacotherapy. The effect of thickenedfeed interventions on gastroesophageal reflux in infants: systematic review and meta-analysis of randomized, controlled trials. Natural evolution of infantile regurgitation versus the efficacy of thickened formula. Effect of body position changes on postprandial gastroesophageal reflux and gastric emptying in the healthy premature neonate. Risk factors for sudden infant death syndrome following the prevention campaign in New Zealand: a prospective study. Effect of Gaviscon Infant on gastro-oesophageal reflux in infants assessed by combined intraluminal impedance/pH. Sodium alginate (Gaviscon) does not reduce apnoeas related to gastrooesophageal reflux in preterm infants. The efficacy of sodium alginate (Gaviscon) for the treatment of gastro-oesophageal reflux in preterm infants.