Duloxetine
General Information about Duloxetine
Moreover, duloxetine has additionally been discovered to enhance total functioning and high quality of life in people with depression and neuropathic ache. This is as a result of of its capability to not solely cut back signs but additionally enhance mood and energy levels, permitting people to engage in day by day actions extra effectively.
However, like most drugs, duloxetine also comes with a couple of side effects, together with nausea, dry mouth, constipation, dizziness, and sleep disturbances. These side effects are often gentle and could be managed by adjusting the dosage or with the assistance of other medicines. It is essential to consult a well being care provider earlier than starting any new treatment and to report any critical unwanted effects immediately.
Duloxetine, generally identified by the brand name Cymbalta, is a drugs that has been found to be effective in treating melancholy and relieving peripheral neuropathic pains related to diabetes. This drug has been a lifesaver for many people who are suffering from these conditions, providing them with much-needed aid and bettering their overall quality of life.
Duloxetine belongs to a class of medicines known as selective serotonin and norepinephrine reuptake inhibitors (SNRIs). This means that it works by increasing the degrees of two necessary neurotransmitters, serotonin and norepinephrine, in the mind. These neurotransmitters play an important position in regulating mood, emotions, and pain sensations.
In conclusion, duloxetine, also called Cymbalta, is a highly efficient treatment for treating depression and relieving peripheral neuropathic pains associated with diabetes. It has been proven to be well-tolerated and has helped countless people regain control of their lives. However, it is very important notice that this treatment ought to only be taken underneath the guidance of a healthcare professional and is not appropriate for everyone. With that stated, duloxetine remains a valuable and life-changing medication for those affected by melancholy and neuropathic pain related to diabetes.
Depression is a typical mental health dysfunction that impacts millions of people worldwide. It is characterized by emotions of disappointment, hopelessness, loss of interest in daily actions, and might even result in ideas of self-harm or suicide. While there are heaps of several types of antidepressants obtainable, not all of them are effective for everybody. This is where duloxetine comes in, because it has been found to be effective in treating several kinds of depression, including major depressive disorder, generalized nervousness disorder, and social nervousness dysfunction.
One of the unique options of duloxetine is its capability to alleviate peripheral neuropathic pains associated with diabetes. Peripheral neuropathy is a sort of nerve damage that may occur as a outcome of excessive blood sugar ranges in people with diabetes. This may cause numbness, tingling, and burning pains within the hands and ft, making it difficult for folks to carry out daily activities. Duloxetine works by modulating the transmission of pain signals by way of the nerves, providing much-needed reduction to these suffering from this condition.
Numerous research have been performed to assess the efficacy and security of duloxetine in treating despair and neuropathic ache related to diabetes. These studies have constantly shown that duloxetine is a well-tolerated and efficient treatment. In reality, in one study, 61% of patients with despair who had been treated with duloxetine reported a significant discount in their signs.
If too much correction is attempted anxiety symptoms uk purchase duloxetine 40 mg with amex, the kyphotic deforming forces can be translated into the new end vertebra and a compensatory curve can even develop. Patient had to undergo a revision due to decompensation in the coronal and sagittal plane. Once corrected, rod-to-rod connectors are used to attach the new rods to the existing ones. Both of these were successfully treated by extending the posterior fusion several levels superiorly. Although revisions are uncommon, both of these studies highlight the fact that revision spine surgery for junctional kyphosis in the neuromuscular patient is technically demanding, but successful outcomes are possible with careful planning. The authors concluded that cervical deformity correction should be offered to patients with Duchenne muscular dystrophy with significant neck deformities at the same time as undergoing thoracolumbar curve correction as these patients are vulnerable to repeat anesthesia and surgery. All patients had stable arthrodesis with significant clinical improvement in posture and were able to maintain horizontal gaze compensatory postures through 10. Although the technique of Giannini does not typically use instrumentation, posteriorly based instrumentation and extension to the occiput has been described with success in addition to posterior releases and bone graft in the treatment of these rare and challenging deformities. This muscle imbalance, especially in the setting of remaining growth, leads to poor head control in extension and often to progressive cervical lordosis and fixed hyperextension contractures. Giannini et al described a technique to address cervical spine hyperextension that has been successfully applied to patients with various underlying myopathies. Next the interspinous spaces are freed using a rongeur, as they are typically very narrow, and then the neck is then forward flexed, correcting the deformity. Finally, wedge-shaped autograft bone without instrumentation is placed between the spinous processes posteriorly to maintain the correction and facilitate arthrodesis. This technique was applied to seven patients with Duchenne muscular dystrophy with rigid neck hyperextension or poor head control in extension in addition to a significant thoracolumbar spinal deformity. Both deformities were corrected in the same operative setting with the cervical extension deformity addressed by the Giannini technique after posterior fusion from T1 to sacrum was complete. All of the patients achieved significant deformity correction, improved posture, and head References [1] Sarwark J, Sarwahi V. Spinal fusion augmented by Luque-rod segmental instrumentation for neuromuscular scoliosis. Results and complications after spinal fusion for neuromuscular scoliosis in cerebral palsy and static encephalopathy using Luque Galveston instrumentation: experience in 93 patients. Maintenance of sagittal plane alignment after surgical correction of spinal deformity in patients with cerebral palsy. Results and morbidity in a consecutive series of patients undergoing spinal fusion with iliac screws for neuromuscular scoliosis. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Complications of the Luque-Galveston scoliosis correction technique in paediatric cerebral palsy. Proximal junctional kyphosis following spinal deformity surgery in the pediatric patient. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Mechanisms of curve progression following sublaminar (Luque) spinal instrumentation. Nontraumatic proximal junctional kyphosis with catastrophic neurologic deficits after instrumented arthrodesis in an adolescent with cerebral palsy: case report and review of the literature. Surgical treatment of neck hyperextension in Duchenne muscular dystrophy by posterior interspinous fusion. The development of validated disease-specific metrics for neuromuscular scoliosis and their use in prospective studies will further help guide decision-making to maximize patient quality of life. Keywords: cerebral palsy, Duchenne muscular dystrophy, flaccid neuromuscular disease, health-related quality of life, myelomeningocele, neuromuscular scoliosis, spinal cord injury, spinal muscular atrophy. However, such motor disorders are often accompanied by disturbances of sensation, perception, cognition, and communication. Despite the static nature of the original insult, patients may also go on to develop secondary musculoskeletal problems, which may be progressive throughout life. Hip displacement usually precedes the onset of scoliosis, but this is not always the case. Children are dependent on their caregivers for much of their care and activities of daily living. These comorbidities may include seizure disorder, hydrocephalus, bowel and bladder 173 Postoperative Management and Complications incontinence, urinary tract infection, gastroesophageal reflux, malnutrition, constipation, aspiration pneumonia, and cardiopulmonary issues. They also experience distressing gastroesophageal reflux, which can be exacerbated in certain positions. Gastric tube feeding is often necessary both to overcome the malnutrition associated with feeding difficulties and to protect against aspiration. Children may develop pressure sores as their spinal deformity worsens, especially if they are thin. Any intervention should progress from a clear understanding of the natural history of the disease.
The authors have found the Shilla procedure to be a viable option in treating early-onset neuromuscular scoliosis anxiety books purchase duloxetine no prescription. However, the indications have continued to evolve to include patients with absent ribs, thoracic constriction related to rib fusion, thoracic hypoplasia, and progressive scoliosis. All patients had at least three expansions with an average of five expansions per child. Complications occurred in 6 of 14 patients: 3 rod fractures, 1 superficial infection treated with antibiotics, 1 superficial infection treated with local debridement, and 1 deep infection requiring a local advancement flap after multiple recurrences and rod removal. However, they do warn that regardless of the system used, a high complication rate persists with multiple procedures in a growing child. Flynn et al reported on 16 patients with myelomeningocele as part of a multicenter investigational device exemption study. In this study, five patients developed a superficial softtissue wound infection treated with local debridement and antibiotics and two patients developed deep wound infections that required removal of implants. They cited that by avoiding midline incisions there were no cases of incisional necrosis. Therefore, it can be used to manage both spinal deformity and respiratory function while maintaining spinal growth in the immature nonambulatory child with myelodysplasia. Careful technique is required in this patient population secondary to the increased risk of infection. In addition, one must be careful to avoid periosteal stripping of the ribs not involved in the proximal rib fixation to minimize rib autofusion. When fusing a skeletally immature patient with neuromuscular scoliosis, there are many factors to consider including pulmonary function, remaining spinal growth, crankshaft phenomenon, and nutritional status. In addition, there are multiple technical options including the use of the Galveston technique with a unit rod and Luque wires, hybrid constructs, and all pedicle screw constructs. Karol et al pointed out the importance of spinal growth and its relationship to pulmonary function. Twenty patients had congenital scoliosis, 3 had idiopathic scoliosis, 3 had neurofibromatosis, and 1 had syndromic scoliosis. In this non-neuromuscular population, 12 of 28 patients were found to have severe restrictive pulmonary disease. They concluded that patients with a proximal thoracic deformity requiring fusion of greater than four levels, especially with rib anomalies, are at the highest risk of restrictive pulmonary disease. Although this cohort is representative of a non-neuromuscular population, it is reasonable to extrapolate these data to the neuromuscular population, as they are frequently unable to perform pulmonary function tests and routinely have worse pulmonary function than patients with non-neuromuscular deformity. Diagnoses included myelomeningocele, spinal cord injury, cerebral palsy, and other myopathies. From this study, they concluded that anterior instrumentation and fusion is a viable option in the management of neuromuscular scoliosis in select patients. Anterior fusion for the "crankshaft phenomenon" is not necessary, even in young patients, when rigid, segmental instrumentation to the pelvis is utilized such as a unit rod. It is our practice to perform both procedures on the same day in relatively healthy patients, provided the time under anesthesia and blood loss are not too substantial after anterior release. When a thoracolumbar curve is greater than 80 degrees and the child is skeletally immature, one technique we utilize is to perform a limited anterior instrumented fusion at the apex of the curve to improve sitting balance and allow for continued pulmonary development and spinal growth. The advantage of this approach is it allows continued spinal growth proximal and distal to the apical fusion without having to undergo multiple procedures under anesthesia. However, it is not without complications including progressive deformity cephalad and caudal to the fusion and the complications associated with an anterior fusion. Tokala et al published their results on a cohort of nine patients with neuromuscular scoliosis that underwent selective anterior single-rod instrumentation for correction of thoracolumbar and lumbar scoliosis. Their group included one patient each with myotonic dystrophy, arthrogryposis, prune belly syndrome, and muscle eye brain syndrome. They concluded that there is a role for anterior instrumentation in carefully selected, ambulatory patients with an idiopathic-like neuromuscular scoliosis. In this study, eight patients showed evidence of major curve progression as defined by progression of the curve of 10 degrees or more. They found that 36% of patients under 8 years of age and those fused short of the pelvis were more likely to progress. However, not every patient must wait until the age of 11 years to undergo this procedure. The mean preoperative curve magnitude and pelvic obliquity was 87 and 28 degrees, respectively. Fourteen patients underwent posterior-only surgery and 1 a combined anterior/posterior fusion. At the most recent follow-up, the curves averaged 29 degrees with a 68% correction rate and pelvic obliquity of 8 degrees with a 71% correction rate. There were 2 complications reported including 1 deep infection and 1 broken rod that did not require any further intervention. In addition, a definitive fusion in a skeletally immature patient with curves measuring 90 degrees results in significant radiographic and quality-of-life improvement. They found the magnitude of curve correction was significantly greater in the pedicle screw group than in the hybrid cohort (p = 0. They also found the mean operative time and estimated blood loss to be significantly lower in the pedicle screw cohort (p < 0. They may return to school in 3 to 4 weeks when their pain is controlled, sitting tolerance is attained, incisional wounds have healed, and no postoperative restrictions are required. The incidence of postoperative complications has been documented to range from 18 to 68%. Respiratory complications are frequent, ranging from atelectasis to more severe problems that require prolonged intubation and ventilator support. Postoperative ileus, pancreatitis, superior mesenteric artery syndrome, and cholelithiasis can occur, and the physician and multidisciplinary team must be vigilant in evaluating any clinical abnormalities.
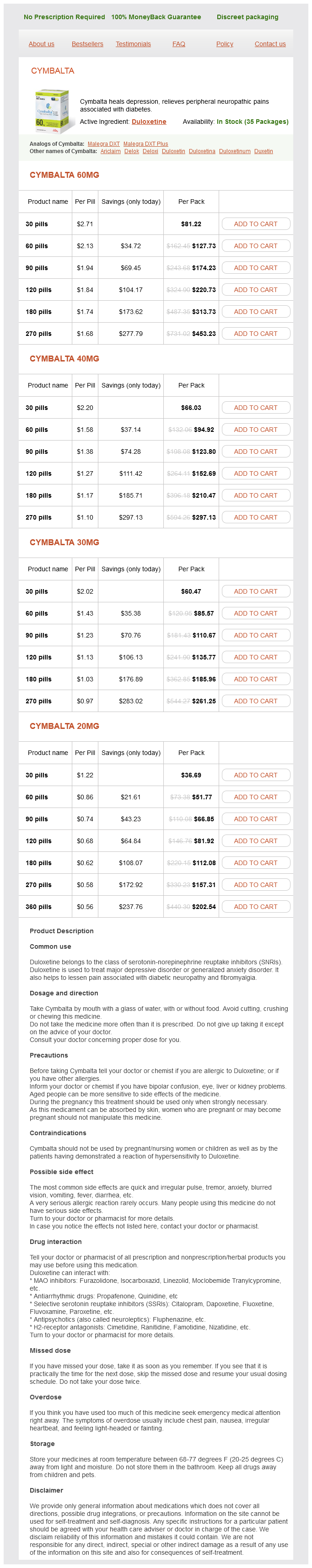
Duloxetine Dosage and Price
Cymbalta 60mg
- 30 pills - $81.22
- 60 pills - $127.73
- 90 pills - $174.23
- 120 pills - $220.73
- 180 pills - $313.73
- 270 pills - $453.23
Cymbalta 40mg
- 30 pills - $66.03
- 60 pills - $94.92
- 90 pills - $123.80
- 120 pills - $152.69
- 180 pills - $210.47
- 270 pills - $297.13
Cymbalta 30mg
- 30 pills - $60.47
- 60 pills - $85.57
- 90 pills - $110.67
- 120 pills - $135.77
- 180 pills - $185.96
- 270 pills - $261.25
Cymbalta 20mg
- 30 pills - $36.69
- 60 pills - $51.77
- 90 pills - $66.85
- 120 pills - $81.92
- 180 pills - $112.08
- 270 pills - $157.31
- 360 pills - $202.54
Documentation about use of contraception and advice about it anxiety symptoms breathing cheap duloxetine 40 mg amex, with assessment of risks including diabetes complications, smoking status, and weight. Glycemic Targets Optimizing glycemic control reduces the risk of congenital abnormalities, and women Table 10. Optimize glucose control 1) Aim HbA1c as close to normal range as possible without significant hypoglycemia. Diet, exercise, and structured education 6) Refer to dietician for education on regular, but small to moderate portions of lowglycemicindex carbohydrates. Screen for diabetic complications 12) Assess for retinopathy at initial visit (unless it has been assessed in previous 6 months) and then annually. Screen for rubella immunity Counsel on risks of pregnancy with diabetes and obesity 15) To fetus: miscarriage, malformation, stillbirth, neonatal death, macrosomia 16) To pregnancy: eclampsia, premature delivery, cesarean section 17) Progression of diabetic complications Consider referral to obstetrician or diabetes specialist midwife 18) Assessment of obstetric risk 19) Further education and support Pre-Pregnancy Care in Type 1 and Type 2 Diabetes 135 should be encouraged and supported to reduce their HbA1c prior to pregnancy. However, this should always be balanced against the risk of severe hypoglycemia for the mother. In agreeing a target HbA1c, women should be advised that any reduction in HbA1c reduces malformation risk to her baby. A recent study (31) demonstrates the risk of malformation is around 10% with a periconceptual HbA1C above 90 mmol/mol (10. A metaanalysis of studies of glycosylated hemoglobin and congenital malformation also showed a stepwise fall in risk with fall in HbA1c, with a 12% risk of malformation for an HbA1c of 108 mmol/ mol (12%), a 6% risk for an HbA1c of 75 mmol/mol (9. However, women should also be aware that the risk of congenital abnormality in the general population without diabetes is around 3%. In contrast, the American Diabetes Association recommends an HbA1c below 53 mmol/mol (7. In order to achieve these targets, women should be encouraged to test intensively, with daily fasting, pre and postprandial blood glucose measurements, and recording results in a home blood glucosemonitoring diary or with a memory meter. Downloading glucose meters at clinic visits or remotely is helpful to verify glucose monitoring. Continuous glucose monitoring systems can be extremely helpful in some patients, particularly for identifying erratic overnight or high postprandial blood glucose levels, or for identifying high postprandial glucose levels in women with suboptimal HbA1c values. Hypoglycemia For women with longstanding type 1 diabetes, a target HbA1c below 48 mmol/mol may not be achievable without the risk of severe hypoglycemia. For these women in particular, the choice of words when expressing risk is important in order to give more meaningful information about an uncommon, albeit serious, outcome. Women may find the concept of individual risk ratios more helpful, in particular when these are related to women with and without diabetes. So, for example, in women without diabetes 1 in 33 pregnancies may have a malformation, while in women with diabetes, the odds are 1 in 33 All women, but especially those with type 1 diabetes, must be advised that they may lose their usual warning signs of hypoglycemia or these may be reduced. Women should always test their blood glucose before driving and should be advised to discontinue driving if there is loss of hypoglycemic awareness. Although there is no human evidence to show hypoglycemia is damaging to the fetus, it is potentially harmful to the mother and can often limit her success in achieving optimum glycemic control. Evers and colleagues showed risk of severe hypoglycemia is increased in women with lower HbA1c and increased duration of diabetes (34). Additional Factors with Pre Pregnancy Care in Women with Type 2 Diabetes Generally, women can be reassured that pregnancy is not associated with an increased risk of microvascular complications (35). Risk of progression of retinopathy is increased by both pregnancy and intensification of glycemic control. It is important that retinal imaging is performed before pregnancy and that any retinopathy is assessed and treated, if necessary, before initiation of tight glycemic control and conception (see Chapter 21). Women with longer duration diabetes or retinopathy present in early pregnancy are most at risk of deterioration in retinopathy during pregnancy (36). Pregnancy outcome in women with mild renal disease should be optimized by optimum control of glycemia and blood pressure, but women need to be advised they are at increased risk of preeclampsia or deterioration of their nephropathy, and premature delivery. These risks can probably be reduced with early and aggressive antihypertensive treatment (37). All women should have an assessment of albumin and creatinine excretion before conception. Women with ischemic heart disease should be referred for assessment by a cardiologist. Factors Other than Blood Glucose Control the specific issues contributing to poor outcomes in type 2 diabetes are complex and include other medical comorbidities, obesity, suboptimal glucose control, potentially teratogenic drugs, older age, greater socioeconomic deprivation, and ethnicity. In particular, tight glycemic control can usually be more easily achieved in women with type 2 diabetes than in women who have type 1. Women must be advised of the wideranging increased risks of pregnancy with obesity, including congenital malformations, perinatal mortality, preeclampsia, prematurity, cesarean section, and thromboembolic disorders. This requires studies in different populations and will also probably require indepth interviews to deepen our understanding of this problem. Women with diabetes have an increased incidence of having a baby with congenital abnormalities, particularly congenital heart defects and neural tube defects. Women should be advised that prepregnancy care will reduce their risk of which of the following pregnancy complications A From higher socioeconomic class B Have a history of retinopathy C Older D To be from an ethnic minority group E To be an exsmoker the correct answer is C. To date, studies have shown no relationship between pre pregnancy care and any of the other complications. Several studies have shown women from an ethnic minority group are less likely to access prepregnancy care.