Eldepryl
General Information about Eldepryl
In conclusion, Eldepryl has been serving to folks with Parkinson's disease to manage their condition effectively for many years. When used in mixture with levodopa, it could possibly help to control symptoms, prolong the consequences of levodopa, and potentially slow down the progression of the illness. If you or someone you understand has been identified with Parkinson's, it is value discussing Eldepryl with your physician to see if it could be an appropriate treatment option. By effectively managing symptoms, patients can keep their independence and continue to guide fulfilling lives despite their situation.
Eldepryl is on the market in tablet form and is usually taken twice a day. Your physician will determine the suitable dosage primarily based on your particular person situation and response to therapy. It is necessary to observe your physician's instructions and to not change the dosage or stop taking the treatment with out consulting them first. Abruptly stopping Eldepryl can result in serious side effects, together with a sudden worsening of Parkinson's symptoms.
Eldepryl isn't appropriate for everyone, and your physician will fastidiously consider your medical history and any other medicines you are taking earlier than prescribing it. For instance, it shouldn't be taken by people with a history of bipolar disorder, extreme liver or kidney illness, or uncontrolled hypertension.
Like any medication, Eldepryl could trigger unwanted effects in some sufferers. These can embody dizziness, headache, dry mouth, constipation, and nausea. In rare cases, it may additionally cause more serious unwanted aspect effects corresponding to hallucinations, confusion, and elevated blood strain. It is important to inform your doctor when you expertise any unwanted facet effects while taking Eldepryl.
Eldepryl is an FDA-approved treatment that's used in combination with levodopa or levodopa and carbidopa mixture to treat Parkinson's illness. It belongs to a class of medication referred to as monoamine oxidase inhibitors (MAOIs) and works by rising the degrees of sure chemical compounds within the mind which are responsible for controlling motion. This, in flip, helps to reduce the symptoms of Parkinson's and enhance motor perform.
Parkinson's illness is a progressive, neurodegenerative disorder that affects greater than 10 million individuals worldwide. It is a movement disorder that is characterised by tremors, rigidity, and issues with balance and coordination. As the disease worsens, it could significantly impact an individual's ability to perform daily actions and lead a traditional life. However, thanks to advances in medical science, there is now a big selection of therapies obtainable to handle Parkinson's and improve the standard of life for those affected by this condition. One such medication is Eldepryl, also recognized as selegiline.
One of the principle advantages of Eldepryl is that it could help to increase the effects of levodopa, which is probably the most commonly prescribed treatment for Parkinson's. Levodopa works by rising the levels of dopamine within the mind, a neurotransmitter that is essential for controlling movement. However, because the illness progresses, the consequences of levodopa are most likely to wear off and turn out to be less efficient. This is identified as the “wearing-off” phenomenon, and it is a main concern for individuals with Parkinson's. By combining Eldepryl with levodopa, patients might experience longer-lasting and more consistent aid from their symptoms.
Furthermore, there's evidence to counsel that Eldepryl may have a neuroprotective impact, which signifies that it could possibly help decelerate the progression of Parkinson's disease. This is because MAOIs like Eldepryl can protect the brain cells that produce dopamine from harm and degeneration. While this isn't a cure for Parkinson's, it could significantly enhance the quality of life for sufferers by delaying the onset of more severe symptoms.
A variety of pathologic conditions medications beta blockers buy generic eldepryl line, physiologic alterations, and medications also can lower plasma pseudocholinesterase activity. Cisatracurium 3 90 Vagolytic (increased heart rate) Pancuronium 3 86 Rocuronium 1 43 Postoperative muscle pain is common; hyperkalemia and increased intraocular and intragastric pressure may occur. Rapid onset makes succinylcholine useful for tracheal intubation in patients with gastric contents. Therapeutic uses: Because of its rapid onset of action, succinylcholine is useful when rapid endotracheal intubation is required. Its brief duration of action results from redistribution and rapid hydrolysis by plasma cholinesterase. Hyperthermia: Succinylcholine can potentially induce malignant hyperthermia in susceptible patients (see Chapter 13). In patients with electrolyte imbalances receiving digoxin or diuretics (such as heart failure patients), succinylcholine should be used cautiously or not at all. Hyperkalemia: Succinylcholine increases potassium release from intracellular stores. This may be particularly dangerous in burn patients, in patients with massive tissue damage in which potassium has been rapidly lost, or in patients with renal failure. Succinylcholine - - - ++ + Na + - - - Depolarized Nicotinic receptor at a neuromuscular junction + ++ Na + c. Most symptoms of cholinergic crisis are mediated by muscarinic receptors and, therefore, the muscarinic antagonist atropine is used as an antidote for sarin poisoning. Cholinergic agonists such as pilocarpine, carbachol, and physostigmine (indirect agonists) worsen symptoms of sarin poisoning. Trospium is a quaternary ammonium compound that minimally crosses the blood brain barrier. Major receptors present in the bronchial tissues are muscarinic and adrenergic-2 receptors. Muscarinic activation causes bronchoconstriction, and 2 receptor activation causes bronchodilation. Therefore, direct or indirect (physostigmine) muscarinic agonists worsen bronchospasm. Ipratropium is a muscarinic antagonist that can relax bronchial smooth muscles and relieve bronchospasm in patients who are not responsive to 2 agonists. Benztropine is used in the treatment of Parkinson disease or relief of extrapyramidal symptoms from antipsychotics. His physician would like to prescribe an inhaled anticholinergic that is dosed once or twice daily. All muscarinic antagonists (anticholinergic drugs) listed above are theoretically useful as antimotion sickness drugs; however, scopolamine is the most effective in preventing motion sickness. Selective blockade (in theory) of the sympathetic ganglion causes reduction in norepinephrine release and, therefore, reduction in heart rate and blood pressure. Receptors at both sympathetic and parasympathetic ganglia are of the nicotinic type. Nicotine is an agonist at nicotinic receptors and produces a depolarizing block in the ganglia. Atropine is a muscarinic antagonist and has no effect on the nicotinic receptors found in the ganglia. A muscarinic antagonist such as atropine is useful in this situation to bring the heart rate back to normal. Vecuronium and rocuronium are hepatically metabolized and the patient has liver disease. Following administration of a neuromuscular blocker, the facial muscles are impacted first, but the pupils are not controlled by skeletal muscle and are not affected. Function returns in the opposite order, so function of the diaphragm returns first. Some sympathomimetics directly activate adrenergic receptors (direct-acting agonists), while others act indirectly by enhancing release or blocking reuptake of norepinephrine (indirect-acting agonists). Neurotransmission at adrenergic neurons Epinephrine released into the blood Norepinephrine Adrenergic receptor Adrenergic receptor Neurotransmission in adrenergic neurons closely resembles that described for the cholinergic neurons (see Chapter 4), except that norepinephrine is the neurotransmitter instead of acetylcholine. Next, dopamine is hydroxylated to form norepinephrine by the enzyme dopamine -hydroxylase. Release of norepinephrine: An action potential arriving at the nerve junction triggers an influx of calcium ions from the extracellular fluid into the cytoplasm of the neuron. The increase in calcium causes synaptic vesicles to fuse with the cell membrane and to undergo exocytosis and expel their contents into the synapse. Binding of norepinephrine to receptors triggers a cascade of events within the cell, resulting in the formation of intracellular second messengers that act as links (transducers) in the communication between the neurotransmitter and the action generated within the effector cell. Norepinephrine also binds to presynaptic receptors (mainly 2 subtype) that modulate the release of the neurotransmitter. Reuptake of norepinephrine into the presynaptic neuron is the primary mechanism for termination of its effects. Potential fates of recaptured norepinephrine: Once norepinephrine re-enters the adrenergic neuron, it may be taken up into synaptic vesicles via the amine transporter system and be sequestered for 150 6. Adrenergic Agonists A -Adrenoceptors Epinephrine Norepinephrine Isoproterenol release by another action potential, or it may persist in a protected pool in the cytoplasm. Two main families of receptors, designated and, are classified based on response to the adrenergic agonists epinephrine, norepinephrine, and isoproterenol. Alterations in the primary structure of the receptors influence their affinity for various agents. For receptors, the rank order of potency and affinity is epinephrine norepinephrine >> isoproterenol.
This medication has a warning for serious psychiatric and behavioral reactions including aggression 4 medications list at walmart buy generic eldepryl 5 mg on line, hostility, irritability, anger, and homicidal ideation. Phenobarbital is a first-line established treatment for focal and tonic clonic seizures but is seldom currently used in developed countries due to its effect on cognition, mood, and behavior. It can produce fatigue, listlessness, and tiredness in adults and insomnia, hyperactivity, and aggression in children (and sometimes in the elderly). Phenobarbital is an enzyme inducer and can accelerate the metabolism of many lipid-soluble drugs and has an impact on bone health. To minimize sedation, it should be started in a low dose (30 mg in adolescents and adults) and increased gradually (15 mg) according to clinical requirements (usual therapeutic daily dose is 60 to 120 mg). The value of measuring drug levels is limited, as it has a relatively wider therapeutic range (15 to 45 mg/L), and the concentration associated with seizure control varies considerably. It is effective for treatment of focal and generalized tonic clonic seizures and in the treatment of status epilepticus. Phenytoin is one of the few examples of switching from first order to saturation kinetics at therapeutic dosage. Accordingly, at higher levels a moderate increment in dose can produce an unexpectedly large rise in the level with accompanying neurotoxicity. Conversely, levels can fall precipitously when the dose is reduced modestly, sometimes resulting in unexpected deterioration in seizure control. The dosage producing the same levels, therefore, varies substantially among different individuals. Reversible cosmetic changes include gum hyperplasia, acne, hirsutism, and facial coarsening. Long-term use may lead to development of peripheral neuropathies and osteoporosis. Although phenytoin is advantageous due to its low cost, it exhibits a narrow therapeutic range (10 to 20 mmol/L). Symptoms of neurotoxicity (drowsiness, dysarthria, tremor, ataxia, cognitive difficulties) become increasingly likely with higher levels, but the diagnosis of phenytoin toxicity should be made on clinical grounds and not assumed from a high level of dosage. Permanent cerebellar damage may be a consequence of chronic toxicity (mental slowing and unsteadiness, and neurological examination may show cerebellar signs). A paradoxical increase in seizure frequency may also occur with marked phenytoin toxicity. Phenytoin can accelerate the metabolism of a number of lipid-soluble drugs, including carbamazepine, sodium valproate, ethosuximide, anticoagulants, steroids, and cyclosporin. Phenytoin and fosphenytoin When the hepatic hydroxylation system becomes saturated, small increases in the dose of phenytoin cause a large increase in the 30 plasma concentration of the drug. It is approved for the adjunctive treatment of seizures associated with Lennox Gastaut syndrome in children over age 4 years and in adults. Carbamazepine and phenytoin can reduce, and valproate can increase the serum concentrations of rufinamide. In postmarketing surveillance, seizures have occurred in patients using tiagabine who did not have epilepsy. Renal stones, glaucoma, oligohidrosis (decreased sweating), and hyperthermia have also been reported. Status Epilepticus 251 All of the available salt forms are equivalent in efficacy (valproic acid and sodium valproate). Commercial products are available in multiplesalt dosage forms and extended-release formulations. The dose should be increased by 5 to 10 mg/kg per week according to the clinical need to achieve optimal clinical response. Frequent dosage adjustments shortly after initiating therapy may be unwarranted as the drug can take several weeks to become fully effective. Rare hepatotoxicity may cause a rise in liver enzymes, which should be monitored frequently. Side effects of sodium valproate include dose-related tremor, weight gain due to appetite stimulation, thinning or loss of hair (usually temporary), and menstrual irregularities including amenorrhea. Sodium valproate can inhibit a range of hepatic metabolic processes, including oxidation, conjugation, and epoxidation reactions. Aspirin displaces sodium valproate from its binding sites on plasma protein and inhibits its metabolism. Valproic acid does not interfere with the hormonal components of the oral contraceptive pill. Its use in women of childbearing potential is not recommended in view of its potential teratogenicity. Several antiseizure medications increase the metabolism of hormonal contraceptives, potentially rendering them ineffective. Pregnancy planning is vital, as many antiseizure medications have the potential to affect fetal development and cause birth defects. Hence, not recommended for primary treatment Hyponatremia, drowsiness, fatigue, dizziness, and blurred vision. Broad spectrum of antiseizure activity Paresthesia, weight loss, nervousness, depression, anorexia, anxiety, tremor, cognitive complaints, headache, and oligohidrosis. Broad spectrum of antiseizure activity Topiramate Gabapentin Unknown Mono/adjunctive therapy in partial seizures Adjunctive for partial seizure ± secondary generalization Adjunctive for partial seizure ± secondary generalization Adjunctive for partial seizures Adjunctive for partial onset seizures ± secondary generalization Adjunctive for all seizure types Mild drowsiness, dizziness, ataxia, weight gain, and diarrhea. One hundred percent renal elimination Weight gain, somnolence, dizziness, headache, diplopia, and ataxia. One hundred percent renal elimination Sedation, weight gain, fatigue, headache, tremor, dizziness, and anorexia. Multiple drug interactions Vision loss, anemia, somnolence, fatigue, peripheral neuropathy, weight gain. Broad spectrum of antiseizure activity Insomnia, dizziness, headache, ataxia, weight gain, and irritability.
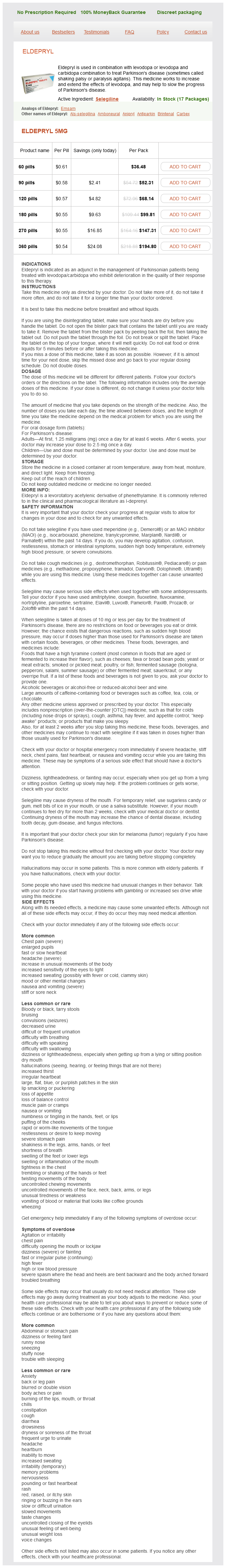
Eldepryl Dosage and Price
Eldepryl 5mg
- 60 pills - $36.48
- 90 pills - $52.31
- 120 pills - $68.14
- 180 pills - $99.81
- 270 pills - $147.31
- 360 pills - $194.80
It delays gastric emptying medications requiring central line eldepryl 5 mg buy visa, decreases postprandial glucagon secretion, and improves satiety. Pramlintide may not be mixed in the same syringe with insulin, and it should be avoided in patients with diabetic gastroparesis (delayed stomach emptying), cresol hypersensitivity, or hypoglycemic unawareness. Liraglutide is also approved to reduce the risk of cardiovascular events and cardiovascular mortality in patients with type 2 diabetes and cardiovascular disease. Consequently, postprandial hyperglycemia is reduced, HbA1c levels decline, and weight loss may occur. Examples of three regimens that provide both prandial and basal insulin replacement. Albiglutide, du/aglutide, and semaglutide are dosed once weekly, while liraglutide is available as a once-daily injection. Exenatide is available as both a short-acting (dosed twice daily) and extended-release preparation (dosed once weekly). Oral Agents 317 lntenshNt th·rapy rasults In a threefold Increase In the frequency of hypoglycemia. Many clinicians believe the Increased risk of hypoglycemia that accompanies intensive therapy is justified by the substantial decrease in the incidence of long-term complications, such as diabetic retinopathy and nephropathy. Effect of tight glucose control on hypoglycemic episodes in a population of patients with type 1 diabetes receiving intensive or standard therapy. Patients who developed diabetes after age 40 and have had diabetes less than 5 years are most likely to respond well to oral glucose-lowering agents. Sulfonylureas these agents are classified as insulin secretagogues, because they promote insulin release from the ~ cells of the pancreas. Mechanism of action: these agents stimulate insulin release from the ~cells of the pancreas. In addition, sulfonylureas may reduce hepatic glucose production and increase peripheral insulin sensitivity. They should be used with caution in hepatic or renal insufficiency, since accumulation of sulfonylureas may cause hypoglycemia. Renal impairment is a particular problem for glyburide, as it may increase the duration of action and increase the risk of hypoglycemia significantly. Glipizide or glimepiride are safer options in renal dysfunction and in elderly patients. In contrast to the sulfonylureas, the glinides have a rapid onset and a short duration of action. Glinides should not be used in combination with sulfonylureas due to overlapping mechanisms of action and increased risk of serious hypoglycemia. Adverse effects: these are largely gastrointestinal, including diarrhea, nausea, and vomiting. These effects can be alleviated by titrating the dose of metformin slowly and administering doses with meals. It should be discontinued in cases of acute myocardial infarction, exacerbation of heart failure, sepsis, or other disorders that can cause acute renal failure. Long-term use may be associated with vitamin 8 12 deficiency, and periodic measurement of vitamin B12 1evels is recommended, especially in patients with anemia or peripheral neuropathy. The dose of insulin may have to be lowered when used in combination with these agents. Rosiglitazone is less utilized due to concerns regarding cardiovascular adverse effects. Renal elimination of pioglitazone is negligible, with the majority of active drug and metabolites excreted in the bile and eliminated in the feces. Adverse effects: Liver toxicity has occasionally been reported with these drugs, and baseline and periodic monitoring of liver function is recommended. Additionally, rosiglitazone carries a boxed warning about the potential increased risk of myocardial infarction and angina with the use of this agent. Mechanism of action: Located in the intestinal brush border, a-glucosidase enzymes break down carbohydrates into glucose and other simple sugars that can be absorbed. When taken at the start of a meal, these drugs delay the digestion of carbohydrates, resulting in lower postprandial glucose levels. However, when used with insulin secretagogues or insulin, hypoglycemia may develop. Bfguanldes M«<ommin Thiazolidinediones Plogllttlzone RoslglltDzone Binds to peroxisome prollferator-actlvated rec:eptor-y In musde. E:xenotlde Is dosed twlc:e dally and extended-release U~~notldels dosed once -ekly. Other agents Both the dopamine agonist bromocriptine and the bile acid sequestrant co/eseve/am produce modest reductions in HbA1c. Although bromocriptine and colesevelam are indicated for the treatment of type 2 diabetes, their modest efficacy, adverse effects, and pill burden limit their use in clinical practice. The prolonged duration Is due to Its low pH, which leads to precipitation at the Injection site and resultant extended action. Insulin lispro is a rapid-acting insulin that has an onset of action within 15 to 30 minutes. Rapidacting insulins are administered to mimic the pranclal (mealtime) release of insulin and control postprandial glu· cose levels. Metformin contains a boxed warning due to the potential for increased risk of myocardial infarction. Sulfonylureas work primarily by increasing insulin secretion through stimulation of the I cells in the pancreas. The primary adverse effects associat~ with metformin are gastrointestinal and in rare cases, lactiC acidosis.