Epitol
General Information about Epitol
Epitol is a prescription drug that is primarily used for the therapy of epilepsy (except for petit mal seizures). It can also be used to handle maniacal conditions, stop maniac-depressive frustration, and likewise within the therapy of alcohol withdrawal. Additionally, this treatment can effectively treat neuralgia of the trigeminal and glossopalatine nerves, and diabetic neuropathy.
Epitol is also seen as a beneficial medicine for the remedy of neuralgia of the trigeminal and glossopalatine nerves. Neuralgia is a pointy, taking pictures pain that happens because of irritation or harm to a nerve. When the trigeminal nerve (which is answerable for sensation within the face) or the glossopalatine nerve (which supplies sensation to components of the mouth) is affected, it could trigger severe and debilitating ache. Epitol helps to alleviate this pain by lowering the overactivity of the nerves.
In addition to epilepsy, Epitol is also used to handle bipolar problems and forestall maniac-depressive episodes. Bipolar dysfunction is a condition that affects an individual's mood, leading to excessive highs (mania) and lows (depression). Epitol helps to steadiness the mood swings and stop extreme episodes of mania or melancholy. This medication is also used in mixture with different medication for the treatment of alcohol withdrawal signs. The calming impact of Epitol can help reduce agitation and anxiousness which are generally experienced throughout alcohol withdrawal.
One of the primary uses of Epitol is within the treatment of epilepsy. Epilepsy is a neurological disorder that results in recurrent seizures or episodes of uncontrolled electrical activity in the mind. These seizures may cause a variety of physical, emotional, and psychological disturbances, making it troublesome for individuals to hold out their day-to-day actions. Epitol works by stabilizing the electrical activity in the mind, which helps in reducing the frequency and severity of seizures.
Another use of Epitol is within the treatment of diabetic neuropathy. Diabetic neuropathy is harm to nerves caused by uncontrolled diabetes. Symptoms include numbness, tingling, and ache within the hands and feet. Epitol may help enhance these symptoms by rising blood circulate and decreasing nerve harm within the affected areas.
It is crucial to note that Epitol can cause some unwanted facet effects, particularly when taken together with other drugs. The commonest side effects noticed include drowsiness, dizziness, nausea, and vomiting. In uncommon cases, it could also trigger extreme allergic reactions, liver harm, and low ranges of blood cells. Therefore, it is very important seek the assistance of a doctor before beginning any new treatment and follow the recommended dosage carefully.
In conclusion, Epitol is a highly efficient medicine for the treatment of assorted neurological problems. Its versatility and effectiveness in treating epilepsy, bipolar disorder, alcoholic abstinence, neuralgia, and diabetic neuropathy make it a popular alternative among medical doctors and patients. However, like some other medicine, it's essential to observe the prescribed dosage and search medical advice earlier than beginning treatment. With correct use, Epitol can significantly enhance the standard of life for individuals with neurological problems.
Epitol, also recognized as Carbamazepine, is a extensively used treatment for treating various neurological problems. It falls beneath the class of temper stabilizing brokers and antiepileptic medicines and is seen as a extremely efficient drug for each treating and preventing neurological issues. In this article, we will take a extra in-depth look at what Epitol is, the means it works, and its numerous uses within the medical field.
Grade I Low grade chondrosarcoma Distinguished from enchondromas by location (long bones/pelvis/scapula and ribs) symptoms 8 days after iui epitol 100 mg buy with visa, and microscopic evidence of Haversian invasion Rarely metastatic 5-year survival 90%. Benign cartilaginous tumours Enchondroma Common, solitary, asymptomatic, intramedullary, cartilaginous tumours 50% occur in the hands When present in long bones, difficult to distinguish from low grade chondrosarcoma Malignant transformation is rare, usually in large lesions in long bones Often present after pathological fracture, particularly in the small bones of the hands and feet X-ray shows a well defined lucent lesion (short zone of transition) with stippled calcification Treatment is by curettage with or without grafting. Dedifferentiated chondrosarcoma characteristically presents as a pathological fracture in the elderly. Prognosis is poor Other rare variants include: Mesenchymal chondrosarcoma Clear cell chondrosarcoma. Chordoma Arises from remnants of the notochord, so almost exclusively arise in the midline/axial skeleton (50% sacrococcygeal, 35% cranial) Slow growing neoplasm, presenting in fifth decade Lytic lesion with bony destruction and focal calcification Systemic metastases in 50% to lymph nodes, lung, liver and bone Treatment is usually surgical excision. Bone-forming tumours15 Reactive or post-traumatic lesions Subungual exostosis Osteocartilaginous lesion of the distal phalanx Treatment is by excision and recurrence is common if incomplete. Small area of increased density within an area of cancellous bone Usually only 12 mm diameter Osteopoikilosis ¼ multiple bone islands. Sometimes seen with cutaneous nodules suggesting a generalized mesenchymal defect. Non-matrix-producing tumours15 Reactive or post-traumatic lesions Unicameral bone cyst Solitary, cystic bone lesions found in the metaphyses of long bones in childhood and adolescence. Options described include minimally invasive decompression and curettage (our preferred option), curettage and grafting, surgical fixation through the cyst with an intramedullary nail or corticosteroid injection. Benign tumours Osteofibrous dysplasia Painless swelling of the tibia/fibula of young children affecting the metaphysis/diaphysis but not the epiphysis X-ray shows intracortical, multiloculated lesion with osteolysis and thinning often with anterior bowing. Malignant tumours Fibrosarcoma Rare, malignant spindle cell tumour affecting the ends of long bones (50% around the knee), in the third to sixth decades X-rays show lucent lesions with cortical destruction and extension in to the soft tissues, a mottled appearance of the bone and indistinct margins Treatment is by wide excision and reconstruction. Aneurysmal bone cyst Solitary, expansile, multiloculated, eccentrically placed, cystic lesion, usually of the long bones or spine (15%) Presents with pain and swelling usually before the third decade X-rays show an expansile lesion with a trabeculated appearance. Malignant transformation and metastasis is a rare but well recognized complication. Locally recurrent tumours are associated with a higher risk of metastatic disease. Developmental or hamartomatous tumours Haemangioma of bone Solitary, asymptomatic lesions, usually affecting the vertebral bodies or skull (lower thoracic most common), comprising thin-walled cavernous blood vessels X-rays show accentuated, thickened vertical trabeculae No treatment is usually required but pathological fracture can occur Widespread disease can occur (skeletal haemangiomatosis/ lymphangiomatosis), but has no known familial tendency and is self-limiting. Bone marrow involvement is associated with a poorer prognosis Reciprocal translation between chromosomes 11 and 22 is seen (t(11;22)(q24;q12)) Chemotherapy is with vincristine, doxorubicin, cyclophosphamide, iphosphamide and etoposide Local treatment is with radiation, surgery or both Overall 5-year survival is 66% (75% with a good response to chemotherapy and 20% in those with a poor response). Benign tumours Eosinophilic granuloma Solitary (80%) bony lesions of unknown aetiology (possibly reactive or inflammatory) classically seen in males in the first decade, usually in the proximal femur, spine, skull or ribs Can be multifocal and include soft tissues, including skin, lymph nodes and lung X-rays show one, or more, well defined lucencies. Immunohaematopoietic tumours Plasmacytoma and multiple myeloma Most common primary bone tumour Multiple myeloma invariably presents in the spine, but may also present in the sternum, ribs, pelvis and skull and limbs Generally presents in or after sixth decade. Classically do not show up on isotope bone scans so skeletal survey is needed Treatment is with steroids and chemotherapy Æ bone marrow transplant. This generally only improves survival rather than effecting a cure A diagnosis of plasmacytoma depends on: 1. No significant protein or immunoglobulin abnormality on urine or serum assays X-rays show a solitary, expansile, lytic lesion Treatment is with radiotherapy or en bloc excision Giant cell tumour of bone Rare (12 per million of population per year) solitary, locally aggressive lesion seen at the epiphyseal ends of long bones (typically distal femur 25%, proximal tibia 25% and distal radius 10%) in the third decade X-ray shows an aggressive lytic lesion in the metaphyseal/ diaphyseal part of the bone, usually juxta-articular. There is often complete cortical destruction and an associated soft-tissue mass Histologically, the tumour comprises spindle-shaped tumour cells and multinucleated giant cells which are indistinguishable from osteoclasts. This lesion needs to be distinguished from giant cell-rich osteosarcoma Treatment is by curettage and grafting and the use of a surgical adjuvant. Local recurrence rates can be high, particularly in difficult sites such as the pelvis, spine and distal radius 290 Chapter 18: Orthopaedic oncology oral core topics the diagnosis of solitary myeloma is debated, as 70% develop disease at multiple sites. Aim for: Immediate stability Immediate weightbearing A durable reconstruction that will outlive the patient and will remain stable if there is local recurrence Radiotherapy may reduce the risk of local recurrence. Leukaemia Haematopoietic disease widely affecting the bone marrow Bone pain is present in 25% of children and 5% of adults with the disease but radiographic changes are present in up to 90% X-rays show: 1. Focal sclerosis Treatment varies with subtype but includes chemotherapy, radiotherapy and, in some cases, bone marrow transplant. Vascular neoplasms Angiosarcoma Usually present with a rapidly enlarging mass in the lower limb in males. Benign fibrous lesions Fibroma of tendon sheath Small, well circumscribed lesions affecting tendons in the hands and feet Treatment is by excision if symptomatic. The natural history is unpredictable in that recurrent nodules can remain dormant for many years, or grow rapidly for some time and then plateau the pathologist will need clinical information when examining a surgical specimen of fibromatosis, as differentiating it from low grade fibrosarcoma can be difficult Radiotherapy may be helpful for recurrent disease. Radiotherapy is sometimes used for recalcitrant disease and recent use of chromic phosphate (p32) has shown some encouraging results. Nodular fasciitis A proliferation of fibroblasts most commonly seen on the volar aspect of the forearm from the second to fifth decades It can be mistaken for a malignant condition because of the hypercellularity, atypia and mitotic rate seen within the rapidly growing lesion Despite the aggressive microscopic features, the condition is self-limiting and can be treated with local excision. Unlike simple lipomas they carry a risk of local recurrence but have almost no malignant potential unless dedifferentiation occurs. Benign schwannoma Encapsulated nerve sheath tumour with a highly ordered cellular component (Antoni A area) and a loose myxoid component (Antoni B area) Usually solitary, fusiform lesions on flexor surfaces of limbs Treatment by marginal excision to spare nerve fibres which are usually splayed over the surface of the lesion. Even with intralesional excision ( to spare nerve function), local control is usually good. Neurofibroma Most occur as solitary lesions in the third decade Non-encapsulated lesions although usually well circumscribed Treatment is by marginal excision. Nf-1 1 in 4000 incidence of which up to 50% are new mutations affecting gene on chromosome 17 Diagnosed by two or more of the following: five or more cafe-au-lait spots two or more neurofibromas or one plexiform neurofibroma Tumour of the optic nerve (optic glioma) Benign growth on the iris (Lisch nodule) Scoliosis Deformity of other bone (especially tibial bowing) Freckling of groin or armpit Parent, sibling or child with Nf-1 Patients are kept under observation and treatment aims at symptomatic control. Malignant transformation occurs in up to 5% and should be treated as per sarcomatous lesions. Myositis ossificans circumscripta Solitary, non-progressive, benign ossification of the soft tissues Usually present as a painful lump within a muscle, often following trauma X-ray shows calcification within the lesion after maturation but may be negative in early presentation Treatment is by surgical excision. Myositis ossificans progressiva Very rare genetic (autosomal dominant), progressive disease affecting groups of muscles, tendons and ligaments 293 Section 4: the adult elective orthopaedics oral usually in the spine and upper limb, leading to progressive fibrosis, calcification and ossification, resulting in deformity.
Some candidates prefer to stick to a surgical approaches book and learn both the approach and the anatomy from it treatment hemorrhoids epitol 100mg purchase free shipping. There is usually a part of a chapter that concentrates on the relevant applied surgical anatomy. The logic is that the only importance of anatomy is to apply it to the safe use of a surgical approach that you will utilize in surgical practice. Practice and rehearse the various surgical approaches to the hip joint, preferably with a colleague about to sit the exam. Colour atlas pictures Candidates may be asked to identify structures labelled in a blank manner on a colour atlas picture. Examination corner Basic science oral 1 Second question after initial discussion on the position a leg assumes after a traumatic posterior and anterior dislocation of the hip. Ascending cervical arteries are given off this ring, which then branch in to retinacular arteries, which form a subsynovial intracapsular arterial ring. Although the two examiners were business-like in their approach and examined well, I was left with the impression that they would have failed me fairly quickly if I had said anything ropy. Basic science oral 2: Anatomy of the posterior thigh the examiner had a colour laminated photocopy of the whole of the posterior thigh from an atlas. All muscles had to be identified with attachments and nerve supply Identification and surface anatomy of the sciatic nerve Popliteal fossa: anatomy, approaches and the neurovascular structure arrangement Posterior approach of the hip: structures going above and below the piriformis muscle, anatomy of the superior and inferior gluteal nerves and arteries. Identification of pudendal nerve and nerve to obturatus internus beneath the piriformis muscle Safe zones for acetabular screws Femoral head blood supply. Basic science oral 3 Anatomy of posterior hip and thigh Surface markings of the sciatic nerve Causes of superior gluteal artery injury the candidate was stopped in mid sentence by the examiner, who was satisfied with the answer and wanted to move on to another question. Basic science oral 6 Anatomy of the gluteal muscles and pelvis Surgical approaches to the hip joint; complications of the direct lateral approach. Basic science oral 7 Blood supply to the femoral head Anterior approach to the hip. The examiners asked me what the diagnosis was and I told them that the radiograph demonstrated a traumatic dislocation of the hip but that I would like to have a lateral view to find out whether the dislocation was anterior or posterior. The examiners asked me what I would do and I said I would take the patient to theatre as soon as possible and attempt a closed manipulated hip reduction. They then told me that the manipulation had failed and asked me to describe the anterior approach to the hip, going through all the various layers and the structures at risk. They then gave me another scenario that the hip was reduced closed but that you suspect there to be loose bodies inside the hip. Extraosseous arterial factors: Blood supply can be interupted by trauma (fractured neck of femur, hip disloation), vasculitis or vasospasm. Intraosseous arterial factors: Block the microcirculation of the femoral head through circulating microemboli. Intraosseous extravascular factors: Increases the hip pressure resulting in a femoral head compartment syndrome. Extraosseus extravascular (capsular) factors: Involve the tamponade of the lateral epiphyseal vessels located within the synovial membrane. This results in intraosseous coagulation that leads to generalized venous thrombosis and retrograde arterial occlusion. Other researchers believe that the condition is caused by a direct cytotoxic effect on osteocytes (alcohol). The crescent sign is a late ficat stage 2 finding, a linear subcortical lucency representing a fracture line and impending femoral head collapse. Many mechanisms are overlapping and mutually supportive and all eventually lead to a final common pathway of vascular occlusion and ischaemia, leading to both marrow cell and osteocyte necrosis. Clinical features Usually non-specific with insidious-onset hip pain which is worse with weightbearing, often present at rest and eventually at night. It is associated with a decreased or painful range of hip movement, limp, muscle weakness and antalgic gait. Flattening of the femoral head without joint narrowing or acetabular involvement 5. Flattening of the femoral head with joint narrowing and/or acetabular involvement 6. Plus Area of femoral head involvement: A, minimal (<15%); B, moderate (1530%); C, extensive (>30%) Surface collapse and dome depression: 2 mm, 24 mm, >4 mm Location: medial, central and lateral Radiology Radiographs. On T2 sequences, the inner border of the peripheral band shows a high signal in 80% of cases. The Mitchell classification may be useful in grading lesion acuity, as infarcted bone will tend to progress through the classes of signal intensity over time. However, this progression is not always consistent, and more than one class of signal abnormality may be found in a single lesion. Small lesions confined to the medial anterosuperior portion of the femoral head tend not to collapse. Electrical stimulation Only a few short-term studies have been published in peerreviewed journals and, whilst they report encouraging early results, most orthopaedic surgeons remain sceptical and this management option has not proved widely acceptable. More long-term studies are required and therefore it remains experimental and requires further evaluation as part of a randomized controlled clinical trial. Joint preserving methods Prevention Identification and elimination of risk factors. Adherence to established guidelines for divers and those working under hyperbaric conditions. Patients with a Kerboull angle >200° more commonly have poor results with certain joint preserving procedures. Mesenchymal stem cells Cultured stem cells are injected under fluoroscopic guidance in to the necrotic lesion following percutaneous core decompression. The stem cells stimulate neogenesis and new bone formation using the necrotic tissue as a scaffold.
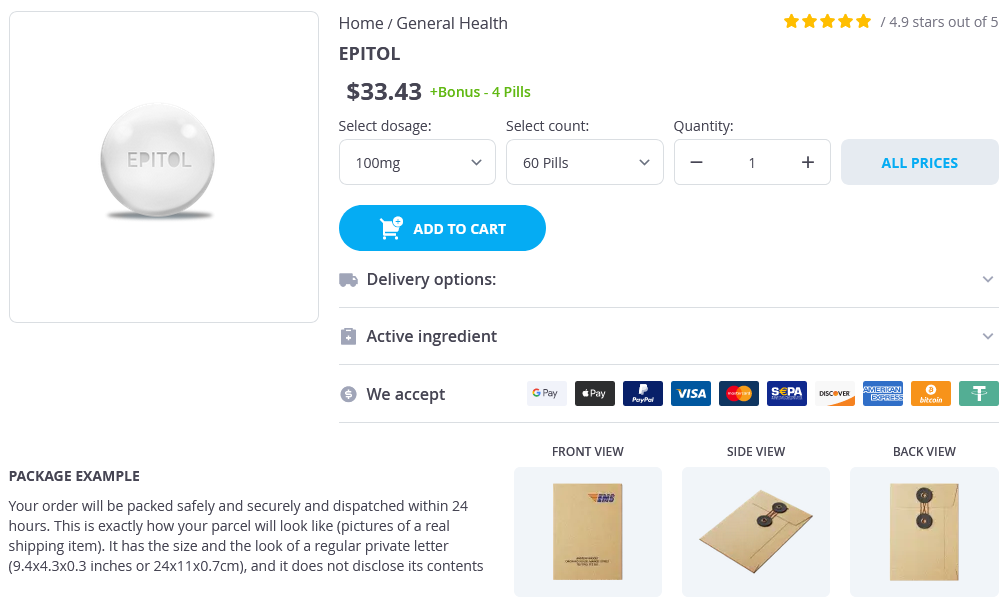
Epitol Dosage and Price
Epitol 100mg
- 60 pills - $37.14
- 90 pills - $47.91
Airway compromise can occur via extrinsic compression or intrinsic involvement of the tongue symptoms zoloft withdrawal epitol 100 mg order line, larynx, or other structures in the airway. Airway compromise is most likely to present in infancy or following infection or trauma. Treatment the goal in treating lymphatic malformations should be preservation or, when necessary, restoration of functional and aesthetic integrity. If there is no significant functional deficit, treatment may be delayed to allow the patient to grow. Macrocystic lesions, especially those in the posterior neck, may be observed and even spontaneously regress. Microcystic lesions can be treated with sclerosing agents with a complete response rate of 14% and partial response rate of 50%. Complication rates for some lesions, including large mixed suprahyoid lesions, are high. Complications include cranial nerve injury, bleeding due to great vessel injury, infection, and airway compromise. Complete excision should be performed whenever possible, but extensive lesions may require subtotal excision to protect vital structures. Infiltrative microcystic lesions are much less easily resected, especially if they are bilateral or suprahyoid, or compromise the aerodigestive tract. Diffuse port-wine stain and venous varicosities are typical of patients with Klippel-Trenaunay syndrome. Klippel-Trenaunay syndrome is usually treated with sclerotherapy, surgery, or a combination of the two. Parkes-Weber Syndrome Parkes-Weber syndrome is a high-flow lesion that consists of a capillaryarterial-venous malformation. A placental chorionic villous mesenchymal core cellular origin for infantile haemangioma. Immunosuppressive effects in infants treated with corticosteroids for infantile hemangiomas. Pelvic Pain: Causes, Symptoms, and Treatments Augus to Pereira-Sanchez, Tirso Perez-Medina, Arantxa Martin Arias and David Abejon Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Spain Pain, is a common health problem that impacts in the quality of life of patient more than other symptom. Chronic pain affect an important number of daily activities of patients such work, sleep or sex life and cause a socio-economic problem of big magnitude. People with chronic pain use a high number of health care resources such emergency, diagnostics and outpatient services and generate a high cost of prescriptions for analgesia and anti-inflammatory drugs. The 25% of people with chronic pain lose their jobs, decrease their work opportunities and is the second reason for claiming incapacity benefits1. Between 2007-2008 the National Center for Health Statistics in United States estimated a 7,0 million emergency visits, in which abdominal pain were the primary reason for the visit. Pain in gynecological disease can be classified from different points of view, depending on anatomical location, cause, duration, severity and characteristics. The current knowledge of the pathophysiology of pain, classified the pain, avoiding the psychogenic pain as: - Neuropathic pain results from injury of peripheral or central nervous system. Neuropathic pain is caused by inappropriate behavior of the nervous system due to damage, disease or trauma. The characteristics of pain are: - - - Sharp, intense, shocking or penetrating pain. Lumbar nerves and innervations area Nerve T12-L1: iliohypogastric: genital branch L1: ilioinguinal: genital branch. L1-L2: Genitofemoral: genital branch L2-L3: Lateral femoral cutaneous L2-L4: Obturator Sensitivity Suprapubic region extending to genitals Pubic mound, pubis and labia majora Pubis, labia majora and round ligament of uterus Lateral thigh to the knee Inner thigh and knee. Pelvic Pain: Causes, Symptoms and Treatments b) Perineal Sensitivity at Sacral Plexus 3 Table 2. Sacral nerves and innervations area Nerve S1-S3: Posterior femoral cutaneous: Perineal branch S2-S3: Sacral S2 and S3: cutaneous perforant branch S2-S4: Pudendal: 3 branches Dorsal nerve of clitoris Clitoris branch Pubic branch Perineal Superficial perineal branch Deep perineal or muscle urethral branch. Inferior anal S4-S5: Anococcygeus Sensitivity Skin on gluteus, adjacent perineum and labia majora Skin on gluteus and adjacent perineum. Skin side of the perineum, labia majora and minora, lower third of the vagina and urethra. Levator ani, superficial and deep transverse perineal, bulbocavernous, ischiocavernosus and coccygeal muscles. We identified other lumbar nerve that can be damaged in gynaecologic surgery: the lateral femoral cutaneous nerve (L2-L3). Causes of Neuropathy in the Lumbar Region a) Direct trauma to nerve: Pfannenstiel incision extended beyond the lateral border of the lower rectus abdominis muscle with a: · · · Direct surgical trauma. Iliohypogastric Neuralgia [6] Iliohypogastric nerve penetrates in transverse abdominal muscle near the iliac crest, standing between it and the internal oblique muscle, crosses and reaches the skin through an opening of 2-3 cm in the fascia of external oblique muscle above the superficial inguinal ring. Location: lower abdominal incisions (Pfannenstiel) Clinical and physical examination · · · Burning sensation or pain in the inguinal surgical incision or suprapubic area, may radiate to the external genitalia. Symptoms are similar to trochanteric bursitis, but are refractory to the conventional treatment. Ilioinguinal Neuralgia [6] Ilioinguinal nerve emerges from the lateral border of psoas muscle; it traverses the anterior abdominal wall to the iliac crest just inferior to the hypogastric nerve. Pelvic Pain: Causes, Symptoms and Treatments Causes · · · · · · Inguinal hernia repair or appendectomy. Clinical and physical examination · Paresthesias, pain, burning sensation and numbness in the lower abdomen. The pain irradiation is to the external genitalia, sometimes at the upper-inner thigh and never below the knee. The weakness of the abdominal wall muscles, creates a bulge in the front of the abdomen (differential diagnosis with inguinal hernia).