Estradiol
General Information about Estradiol
In conclusion, Estradiol, also referred to as Estrace, is a synthetic form of estrogen that plays an important position in the feminine reproductive system. It is commonly prescribed as a hormone alternative remedy to deal with menopause symptoms, corresponding to sizzling flashes, vaginal dryness, burning, and irritation. It can even have other well being advantages, corresponding to maintaining strong bones and enhancing pores and skin elasticity. Despite its potential unwanted side effects, Estradiol has confirmed to be an effective remedy for menopause signs, helping ladies to navigate this pure biological course of with extra ease and comfort.
Another widespread menopause symptom that Estradiol may help with is vaginal dryness. As estrogen levels lower, the vaginal tissues turn out to be thinner, drier, and fewer elastic. This can result in uncomfortable symptoms such as vaginal dryness, burning, and irritation. These symptoms could make sexual activity painful and can even enhance the danger of vaginal infections. Estradiol helps to reverse these adjustments by restoring the estrogen levels, thus bettering vaginal elasticity and moisture. This can help to alleviate signs and improve a woman’s overall sexual health.
Like any medicine, Estradiol has some potential unwanted facet effects that girls ought to pay consideration to. These can include breast tenderness, nausea, headache, and mood adjustments. It is essential to seek the advice of a well being care provider before beginning any hormone substitute remedy to discuss the advantages and potential dangers.
Apart from treating menopause signs, Estradiol has additionally been found to produce other health benefits. It helps to take care of strong bones by growing bone density, which might lower as a girl ages. This can forestall the development of osteoporosis, a condition where the bones become weak and brittle, making them more susceptible to fractures. Estradiol additionally performs a job in maintaining wholesome skin by promoting collagen manufacturing, which might help reduce the appearance of wrinkles and improve skin elasticity.
One of the most common menopause signs that Estradiol helps to enhance is sizzling flashes. Hot flashes are sudden emotions of heat that may cause sweating, flushing, and chills. They can happen at any time, making it difficult to hold out day-to-day actions. Estradiol helps to manage the body’s temperature by changing the estrogen levels that have decreased throughout menopause. This helps to scale back the frequency and intensity of scorching flashes, making menopause extra manageable.
Estradiol is commonly prescribed as a hormone replacement therapy (HRT) to treat menopause symptoms. Menopause, which often occurs between the ages of 45 and fifty five, is a natural biological course of that marks the top of a woman’s reproductive years. However, the drop in estrogen levels during menopause may find yourself in uncomfortable symptoms that may intrude with a woman’s high quality of life. Estradiol works by replacing the misplaced estrogen, thus assuaging these signs.
Estradiol, also recognized as Estrace, is a synthetic type of the feminine hormone estrogen. It plays a vital position in sustaining the normal functioning of the feminine reproductive system. As women age, their estrogen ranges decrease, causing numerous symptoms corresponding to sizzling flashes, vaginal dryness, burning, and irritation.
Grossly women's health vs fitness magazine order line estradiol, adenomas are sharply demarcated from the normal parenchyma and appear light in color. Microscopically, adenomas consist of cords of cells that closely resemble normal hepatocytes; indeed, histologic differentiation between adenoma and normal liver tissue can be di cult. However, adenoma cells are larger than normal hepatocytes and may contain large amounts of glycogen and lipid. Hepatocellular adenomas are often rst detected by ultrasonography during evaluation for right upper quadrant abdominal symptoms. Other ndings may include signi cant heterogeneity due to intratumoral hemorrhage, or calci cations due to hemorrhage and necrosis. Areas of old hemorrhage and necrosis will appear as discrete foci of hypoattenuation on nonenhanced imaging. Arterial phase contrast images may show some degree of peripheral enhancement due to the larger peripheral feeding vessels. Inconsistency is also reported for T2-weighted imaging, but the majority of adenomas will be hyperintense relative to the liver on T2 imaging. Since adenomas have a scarcity of Kup er cells, Kup er cellspeci c agents will result in decreased signal intensity on T2-weighted imaging. Note the rapid homogenous contrast enhancement seen on arterial phase images and rapid contrast washout seen on delayed images. Pathologically, these appear as well-di erentiated bile ductular structures surrounded by a brous stroma. As a group, malignant tumors of the liver present major diagnostic and therapeutic challenges. Although surgery can be potentially curative, most hepatobiliary cancers are discovered at a stage too advanced to permit complete resection. Over the last two decades, considerable advances have been made in the diagnosis and treatment of these tumors. Enhancements in imaging have permitted earlier detection and more accurate staging of disease. Contemporary surgical therapy is guided by improved imaging techniques and a better understanding of disease biology. Furthermore, novel palliative treatments such as radiotherapy and ablative techniques have extended the limits of tumor eradication and treatment. Nodular regenerative hyperplasia is an uncommon lesion associated with conditions of chronic liver disease. Percutaneous biopsy can be obtained to con rm the diagnosis of nodular regenerative hyperplasia, which should be managed nonoperatively. As this is a di use condition of the liver resulting from identi able causes, ultimate treatment should be directed toward the speci c etiology. Because of this anatomic con guration, these are easily excised with minimal loss of functional hepatic parenchyma. Because the liver is relatively hidden behind the right costal cartilages, tumors can reach a substantial size before becoming palpable. Furthermore, the large functional reserve of the liver generally masks any small impairment resulting from local parenchymal disturbances by tumor. Patients usually complain of a dull and vague right upper quadrant pain that is sometimes attributable to the shoulder. Patients with bleeding esophageal varices have an extraordinarily poor prognosis, with a median survival measurable in weeks. Symptoms of tumor rupture include acute abdominal pain and swelling, and signs include abdominal distension, guarding, rebound tenderness, and ileus. Patients also commonly have signs of hemodynamic instability or overt hypovolemic shock. Diagnosis is con rmed by ndings of tumor mass and peritoneal blood through imaging, laparotomy, or paracentesis. Porphyria cutanea tarda, virilization and feminization syndromes, carcinoid syndrome, hypertrophic osteoarthropathy, hyperthyroidism, and osteoporosis can also occur. Note the acute extravasation of contrast seen on early arterial phase images with pooling of blood seen on delayed images. Hemorrhage or tumor rupture can occur, and there is also a risk of tumor spillage and seeding of the needle biopsy tract. Indeed, in this clinical scenario, the histologic appearance of the non-neoplastic liver may have a greater impact on surgical planning; if the presence of advanced cirrhosis will preclude safe resection, we will biopsy the nontumoral liver for histologic evaluation. In such cases, ne-needle aspirate for cytologic evaluation has been shown to yield a higher percentage of correct diagnoses compared with microhistology of core needle biopsy specimens (86 vs 66%). Many centers consider bone scans to be mandatory prior to liver resection; this should certainly be performed for patients with pain that could be attributable to bony metastases. Scans should therefore be scrutinized for evidence of vascular invasion, since therapy and prognosis can be signi cantly altered by the presence of such ndings. Generally, partial hepatectomy is o ered only to patients who are Child A and the most favorable class B patients. Investigators have used the elimination of certain dyes that are exclusively cleared by the liver, such as bromosulphthalein or indocyanine green, as measures of hepatic function. Galactose clearance and [14C] aminopyrine clearance have also been used to evaluate the metabolic capacity of the liver.
If the point of obstruction is not obvious menopause insomnia order estradiol pills in toronto, decompressed bowel distal to the obstruction can be identi ed and followed proximally to the point of obstruction. Care should be taken when handling the obstructed bowel at or near the point of obstruction when acutely obstructed, especially if it is xed at an apparent site of obstruction or if it is ischemic. After the o ending obstruction has been corrected, a thorough exploration of all four quadrants should always be undertaken to ensure that all intestinal injuries are repaired, nonviable segments are resected, and a second site of obstruction or xation is not overlooked; this concept is especially true for volvulated segments of small bowel where two points of xation are often present. Sometimes obstructing bands traversing a sizeable part of the peritoneum can a ect more than one loop of bowel. When a small bowel resection is necessary, intestinal continuity of the small bowel can be accomplished generally with a primary anastomosis unless there is generalized peritonitis and the edges of the remnant bowel are of questionable viability. When an intestinal anastomosis is performed, the discrepancy in bowel diameter and wall thickness between the obstructed proximal bowel and decompressed distal bowel are important factors in choosing anastomotic techniques. In addition, a stapled anastomosis may be less safe in cases where a large discrepancy in bowel wall thickness exists or when there is bowel wall edema, because uniform approximation of the tissue for a given staple height may not be possible. Abdominal closure may be di cult to achieve when the small bowel is massively dilated. Techniques described for intraoperative decompression include manual retrograde decompression into the stomach (with careful handling of the obstructed bowel), intraoperative passage of a long nasointestinal tube, and, rarely, performance of a controlled enterotomy with passage of a decompressing tube; the latter technique is strongly discouraged except under very select circumstances, such as tremendous intestinal distention preventing abdominal closure or distention threatening bowel 604 Part V Intestine and Colon viability. Manual retrograde decompression of luminal contents around the ligament of Treitz, through the pylorus, and into the stomach allows for aspiration through the nasogastric tube by the anesthetist. When decompressing the bowel, care must be taken to handle the in amed and distended bowel gently, because experimental studies have demonstrated an increased rate of bacteremia after extensive manipulation of obstructed bowel. Although intraoperative decompression has not been shown to decrease the rate of postoperative complications or the speed of return of bowel function, it certainly does make the closure easier, faster, and safer. Resection should be undertaken with caution, especially in patients with a limited length of bowel from a previous resection or those with large sections of ischemia. In patients who would otherwise be left with less than two-thirds of their original bowel length after resection of all bowel of questionable ischemia, consideration may be given to resecting all the grossly necrotic or obviously nonviable bowel, but preserving bowel of questionable viability and performing an end ostomy or a second-look procedure 1224 hours later, particularly if the viability of the ends to be anastomosed is in question. Many series compare patients treated laparoscopically to those who failed initial laparoscopic treatment. Operative intervention in these patients would be more involved and complex whether done open or laparoscopically. One would expect these patients to have greater hospital stays, greater complication rates, and slower return of bowel function independent of the method of abdominal access. In addition, the skill and con dence level of the surgeon should weigh in the decision to approach the obstruction laparoscopically. First, if the surgeon lacks skill in using moderately advanced laparoscopic techniques, an open operation may be a better choice. Similarly, if the patient is known to have a frozen abdomen or has either a severely distended, tense abdomen with markedly distended bowel or multiple dense adhesions at the time of insertion of the laparoscope, conversion to an open procedure is wise. Initial access for creating the pneumoperitoneum in a patient with a small bowel obstruction is achieved best by a fully open approach under total visual control, but limited data support this concept. Bypass relieves the obstruction while reestablishing intestinal continuity and preventing a closed-loop obstruction; however, the advisability of a bypass procedure should be considered. For instance, in the presence of carcinomatosis, a bypass may prove fastest and safest, because patient survival will be short. Laparoscopy is known to cause fewer adhesions than open laparotomy77 and in that regard may be superior to laparotomy for the treatment of adhesive small bowel obstruction. Several studies have shown laparoscopy to be a safe and e ective means of access for the operative treatment of small bowel obstruction. Recurrent obstruction is more common in patients with multiple adhesions, matted adhesions, previous admissions for small bowel obstruction, and previous pelvic, colonic, and rectal surgery. A simple technique to prevent adherence of the bowel to the undersurface of the fascial incision is to interpose the omentum between the bowel and the incision. Other more intricate techniques, such as the Noble plication and the Childs-Phillips transmesenteric placation, have been described in the more distant past. Attempts to "plicate" the bowel with a long intestinal tube, so-called intraluminal plication, are also of questionable e cacy. In some patients, it will become evident during the course of the operation that complete or adequate adhesiolysis is not possible or may risk vascular injury to a substantial segment of bowel because of the acute in ammatory nature or tenacity of the adhesions. In such situations, it may be important to control any bowel injuries present, end any further dissection, and conclude the operation to prevent further bowel injury and its potential sequelae. In some situations, the mature decision might be to provide proximal diversion with a proximal enterostomy if the obstruction has no chance for resolution (eg, due to malignancy or radiation) or if a more distal bowel repair is tenuous, or to place a tube gastrostomy for diversion and patient comfort. Pursuing a futile attempt to complete the adhesiolysis puts the patient at risk for serious bowel injury or devascularization injury necessitating resection of otherwise normal bowel with the risk of enterocutaneous stulation or subsequent short bowel syndrome. Some authors have placed a Silastic sheet between two injured peritoneal surfaces; when left in place for 36 hours, no adhesions formed between these surfaces thereafter. Furthermore, if the membrane is wrapped around an intestinal anastomosis, the leak rate is increased. Initial concerns that were raised over the safety of hyaluronate barriers appear unfounded, with the exception of iron cross-lined hyaluronate that was withdrawn from the market. A prospective, randomized, controlled trial showed that hyaluronate barriers did not increase the risk of intra-abdominal abscess or pulmonary embolism83; however, in a post-hoc subgroup analysis of 289 patients in whom the hyaluronate membrane was wrapped around a fresh anastomosis, the rates of leak, stula formation, peritonitis, abscess, and sepsis were increased. Based on these studies and assumptions, the use of hyaluronate membranes in elective abdominal surgery does decrease the amount of postoperative adhesions at the site of application but does not decrease the incidence of intestinal obstruction or the need for future reoperation for obstruction. Use of these products requires careful consideration, because they are expensive and their clinical bene t appears to be relatively low.
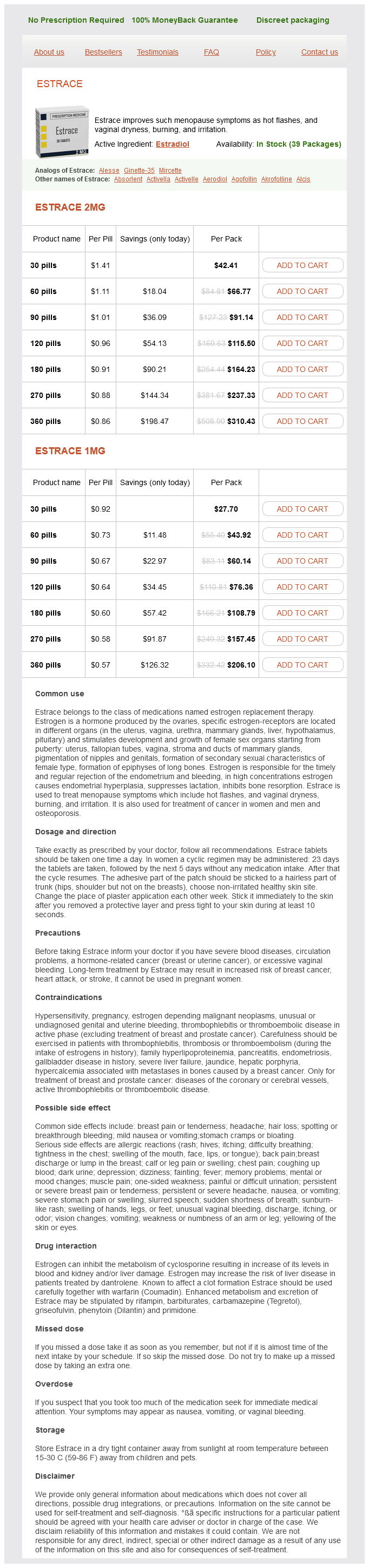
Estradiol Dosage and Price
Estrace 2mg
- 30 pills - $42.41
- 60 pills - $66.77
- 90 pills - $91.14
- 120 pills - $115.50
- 180 pills - $164.23
- 270 pills - $237.33
- 360 pills - $310.43
Estrace 1mg
- 30 pills - $27.70
- 60 pills - $43.92
- 90 pills - $60.14
- 120 pills - $76.36
- 180 pills - $108.79
- 270 pills - $157.45
- 360 pills - $206.10
Global genomic analysis of intraductal papillary mucinous neoplasms of the pancreas reveals signi cant molecular differences compared to ductal adenocarcinoma menstruation excessive bleeding estradiol 1 mg purchase line. Clinical fate of branch duct and mixed forms of intraductal papillary mucinous neoplasia of the pancreas. Do consensus indications for resection in branch duct Intraductal papillary mucinous neoplasm predict malignancy Intraductal papillary mucinous neoplasms: predictors of malignancy and invasive pathology. Natural history of branch duct Intraductal papillary mucinous neoplasms of the pancreas without mural nodules: long-term follow-up results. Cyst size indicates malignant transformation in branch duct intraductal papillary mucinous neoplasms of the pancreas without mural nodules. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate Experience with 208 resections for intraductal papillary mucinous neoplasms of the pancreas. Adjuvant chemoradiotherapy after pancreatic resection for invasive carcinoma associated with intraductal papillary mucinous neoplasms of the pancreas. Clinical signi cance of frozen section analysis during resection of intraductal papillary mucinous neoplasm: should a positive pancreatic margin for adenoma or borderline lesion be resected additionally Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. Solid and pseudopapillary tumor of the pancreas: review and new insights into pathogenesis. Solid and pseudopapillary tumor of the pancreas: a case series of 26 consecutive patients. Cystic pancreatic endocrine tumors: an endoscopic ultrasound-guided ne-needle aspiration biopsy study with histologic correlation. Acinar cell carcinoma of the pancreas in the United States: prognostic factors and comparison to ductal adenocarcinoma. Acinar cell carcinoma with a prominent intraductal growth pattern: case report with review of the literature. Pancreatic cysts caused by carcinoma of the pancreas: a pitfall in the diagnosis of pancreatic carcinoma. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Pancreatic ductal adenocarcinomas in long-term followup patients with branch duct intraductal papillary mucinous neoplasms. Predictors of the presence of concomitant invasive ductal carcinoma in intraductal papillary mucinous neoplasm of the pancreas. Synchronous and metachronous extrapancreatic malignant neoplasms in patients with intraductal papillary-mucinous neoplasm of the pancreas. Frequency of extrapancreatic neoplasms in intraductal papillary mucinous neoplasm of the pancreas: implications for management. Intraductal papillary mucinous tumors of the pancreas: imaging studies and treatment strategies. Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor. Mucin-hypersecreting tumors of the panceas: assessing the grade of malignancy preoperatively. Predictive factors for malignancy in intraductal papillary-mucinous tumors of the pancreas. Intraductal papillary mucinous neoplasms of the pancreas with multifocal involvement of branch ducts. Intraductal papillary mucinous neoplasms of the pancreas: di erentiation of malignant and benign tumors by endoscopic ultrasonography nding of mural nodules. Intraductal papillary mucinous neoplasms of the pancreas: performance of pancreatic uid analysis for positive diagnosis and the prediction of malignancy. Cameron Periampullary cancers are composed of a group of malignant neoplasms arising in the region of the ampulla of Vater. Less commonly, acinar cell carcinomas or pancreatic endocrine neoplasms occur in the periampullary region of the pancreas. Periampullary cancers are often discussed as a group based on their similar presentation, workup, and surgical management. In addition, pancreas cancer is also discussed with this group since the natural history for both proximal and distal pancreatic lesions is similar-di ering mainly in the type of resection performed. He described a local ampullary resection with reanastomosis of the pancreatic and bile ducts to the duodenum in a patient who presented with obstructive jaundice. Codivilla is often credited with performing the rst en bloc resection of the head of the pancreas and duodenum for periampullary carcinoma, but this patient did not survive beyond the early postoperative period. Currently, the resection of periampullary cancer with a pancreaticoduodenectomy is performed routinely at many 59 referral centers and carries a mortality of approximately 2%. Moreover, signi cant advances have been made in understanding of the pathogenesis, biology, and staging of periampullary carcinoma in the past two decades. Pancreatic cancer is the fourth leading cause of cancer death in the United States. In 2009, there were an estimated 35,240 deaths in the United States compared to 159,390 deaths for lung cancer, 49,920 for colorectal cancer, and 40,610 for breast cancer. Since 1973, the incidence in the United States has remained stable at about 89 per 100,000 of population. In Japan, however, a dramatic increase has been observed during the last three decades, although the overall incidence is still less than that observed in the West. Review of pancreaticoduodenectomy specimens from high-volume centers reveals that 4060% are adenocarcinomas of the head of the pancreas, 1020% are adenocarcinomas of the ampulla of Vater, 10% are distal bile duct adenocarcinomas, and 510% are duodenal adenocarcinomas. Because these data represent resected specimens and because the resectability rate of the nonpancreatic periampullary cancers is much higher, it is likely that pancreas cancer is the site of origin in up to 90% of cases.