Etodolac
General Information about Etodolac
One of the widespread side effects of Etodolac is abdomen upset, which can be minimized by taking the medicine with food or milk. Some sufferers may also experience dizziness, headache, or drowsiness. These unwanted effects are normally gentle and go away with time, but when they persist or worsen, it is essential to consult a physician.
Etodolac is out there in the type of tablets and extended-release tablets, with doses starting from 200 mg to 600 mg. The dosage and duration of therapy might vary depending on the patient's age, medical history, and the severity of their situation. It is crucial to comply with the prescribed dosage and to not exceed the really helpful period of therapy, as it could lead to opposed results.
Etodolac is a non-steroidal anti-inflammatory drug (NSAID) that is commonly used to treat pain and irritation caused by conditions such as arthritis or osteoarthritis. It belongs to the propionic acid class of NSAIDs and is available underneath numerous brand names corresponding to Lodine, Lodine XL, and Etogesic.
Etodolac works by inhibiting the synthesis of prostaglandins, which are substances within the body that cause ache and irritation. It does this by blocking the motion of the enzyme cyclooxygenase (COX), liable for producing prostaglandins. By lowering the levels of prostaglandins, it helps to alleviate pain and inflammation, providing aid to sufferers suffering from arthritis or osteoarthritis.
Etodolac should not be taken by patients with a history of allergic reactions to NSAIDs or those who have had asthma, hives, or different allergic reactions after taking aspirin or other NSAIDs. It is also not really helpful to be used in patients with extreme coronary heart, liver, or kidney diseases. It is crucial to inform the physician about any pre-existing medical circumstances and other medications being taken to keep away from potential interactions.
One of the numerous advantages of Etodolac is that it has an extended duration of action compared to other NSAIDs. This means that it could be taken much less incessantly, normally a couple of times a day, and still provide effective ache relief. It also has a greater security profile in comparability with different NSAIDs, making it a super choice for long-term use in persistent circumstances.
In conclusion, Etodolac is an effective and safe NSAID that is broadly used within the treatment of continual ache and inflammation brought on by conditions such as arthritis or osteoarthritis. Its longer period of motion, higher safety profile, and fewer unwanted effects make it a most well-liked choice for lots of sufferers. However, it's essential to use this treatment as prescribed and to seek the assistance of a physician if any antagonistic effects are skilled. With correct usage, Etodolac can present significant relief to these suffering from arthritis or osteoarthritis, permitting them to live a extra comfortable and energetic life.
Arthritis is a persistent condition that causes irritation and ache in the joints. Osteoarthritis, however, is a degenerative joint disease that occurs as a outcome of wear and tear of the joints over time. Both of those situations can considerably impression an individual's high quality of life, making it difficult to perform every day actions.
Sclerotherapy of varicose veins in patients with documented thrombophilia: a prospective controlled randomized study of 105 cases arthritis pain in hip purchase generic etodolac canada. Polidocanol foam 3% versus 1% in the great saphenous vein: early results [in French]. Outcomes and side effects of duplex-guided sclerotherapy in the treatment of great saphenous veins with 1% versus 3% polidocanol foam: results of a randomized controlled trial with1-year follow-up. Comparison of 1% and 3% polidocanol foam in ultrasound guided sclerotherapy of the great saphenous vein: a randomised, double-blind trial with 2 year-follow-up: "the 3/1 study. Randomized clinical trial of different bandage regimens after foam sclerotherapy for varicose veins. Foam sclerotherapy of the saphenous veins: randomized controlled trial with or without compression. First human use of cyanoacrylate adhesive for treatment of saphenous vein incompetence. Endovenous mechanochemical ablation of great saphenous vein incompetence using the ClariVein device: a safety study. Mechanochemical endovenous ablation of small saphenous vein insufficiency using the ClariVein device: one-year results of a prospective series. Revision of the venous clinical severity score: venous outcomes consensus statement. Venous clinical severity score and quality-of-life assessment tools: application to vein practice. A study to compare disease-specific quality of life with clinical anatomical and hemodynamic assessments in patients with varicose veins. Cure and reappearance of symptoms of varicose veins after stripping operation: a 34 year follow-up. Recurrence after varicose vein surgery: a prospective long-term clinical study with duplex ultrasound scanning and air plethysmography. Recurrent varicose veins after surgery: a new appraisal of a common and complex problem in vascular surgery. Long-term outcomes of endovenous radiofrequency obliteration of saphenous reflux as a treatment for superficial venous insufficiency. Endovenous ablation (radiofrequency and laser) and foam sclerotherapy versus conventional surgery for great saphenous vein varices. Surgery and endovenous techniques for the treatment of small saphenous varicose veins: a review of the literature. A systematic review and metaanalysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Recurrent varicose veins and primary deep venous insufficiency: relationship and therapeutic implications. Saphenous surgery does not correct perforator incompetence in the presence of deep venous reflux. Surgical correction of main stem reflux in the superficial venoussystem: does it improve the blood flow of incompetent perforating veins Treatment of superficial and perforator venous incompetence without deep venous insufficiency: is routine perforator ligation necessary Effectiveness and safety of ultrasound-guided foam sclerotherapy for recurrent varicose veins: immediate results. Duplex ultrasound outcomes following ultrasound-guided foam sclerotherapy of symptomatic recurrent great saphenous varicose veins. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. Review and comment of the 2011 clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. Management of chronic venous disorders of the lower limbsguidelines according to scientific evidence. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians Task Force. When the obstruction occurs in the iliofemoral segment, postthrombotic morbidity is often severe. In a recent study, the intraluminal contents of chronically occluded postthrombotic common femoral veins were analyzed. In fact, randomized trials, registries, and large observational experiences have demonstrated a reduction in the incidence of postthrombotic syndrome after successful thrombus removal. Ambulatory venous hypertension is the underlying pathophysiology resulting from venous valvular incompetence and postthrombotic luminal obstruction. In this setting, compartment pressures can be used as a surrogate for venous pressures. Labropoulos et al5 measured arm-foot pressure gradients in patients with chronic postthrombotic venous disease. Patients with iliofemoral venous disease had the highest resting and postocclusive hyperemic pressures compared with patients with infra-inguinal postthrombotic disease. Unfortunately, a thrombus in the iliofemoral venous system frequently persists, causing central venous obstruction. This is largely due to persistent obstruction of the major venous outflow tract of the lower extremities. Antibodies to four biomarkers were used to examine the specific function of these endothelial cells. Luminal obstruction Based on ultrasound findings and phlebography, the obstructive nature of the thrombus in the vein lumen has been variously described as chronic thrombus, intraluminal fibrosis, or scar tissue. Until recently, no definitive description of the human tissue that chronically obstructs postthrombotic veins has been provided. In an attempt to resolve the extreme morbidity of these patients, those presenting with incapacitating postthrombotic syndrome due to chronic iliofemoral and inferior vena cava occlusion are fully evaluated. If the common femoral vein is obstructed, it is recommended to perform a common femoral vein endophlebectomy followed by transluminal recanalization of the occluded iliac veins and inferior vena cava (if involved).
Single administration of the other drugs mentioned does not require any limitation of breastfeeding arthritis in dogs remedies discount etodolac online visa. However, a critical look at the indications, and in some cases a change in therapy, should be undertaken. Bisacodyl and osmotic agents such as lactulose, or saline agents such as sodium sulfate, are also scarcely absorbed. Although there is no documented experience available on macrogol, it seems acceptable because of low intestinal resorption. The inhibition of the absorption of fat-soluble vitamins with castor oil, and the possible drastic action of sodium picosulfate, argue against their use. If a change in dietary habits is not successful, bulking agents, senna preparations, bisacodyl, and both saline and osmotic agents 4. A single administration of another laxative does not require any limitation of breastfeeding, but use of the laxative should be stopped. The sulfonamide salazosulfapyridine (sulfasalazine) was, for a long time, the standard medication for treating ulcerative colitis. With a maternal daily dosage of 3 g, up to 10% of the weight-related portion can reach the infant. One case report mentioned bloody diarrhea in a breastfed baby whose plasma concentration was 5. Mesalazine consists of 5-aminosalicylic acid, the anti-inflammatory portion of sulfasalazine. However, taking into consideration the metabolite, acetyl-5-aminosalicylic acid (about 12 mg/l of milk), it would be 7. A further publication also reports 15 mg active ingredient per liter (Christensen 1994). Silverman (2005) found very low levels of 5-aminosalicylic acid in the milk of four lactating mothers; however, the content of the relatively inactive metabolite N-acetyl-5-aminosalicylic acid was 1000-fold higher. A case report described an infant who developed diarrhea following repeated rectal administration of mesalazine to his mother. In a further group of eight breastfeeding women, there was also a report of a child with diarrhea (Ito 1993). However, the authors of this book have found no symptoms in the overwhelming majority of the infants observed, regardless of the dosage. Olsalazine, which consists of two mesalazine molecules, has an intestinal absorption rate of about 2% and can only be detected 654 4. Considering its very widespread use, the absence of further publications regarding the toxic effects of these antidiarrheal medications on the infant argues for good tolerance of these drugs during breastfeeding. If the sulfonamide effect of sulfasalazine is particularly desirable, this drug may also be used. Corticoids may be administered both rectally and systemically during breastfeeding. For immunosuppressive medications used for chronic inflammatory bowel disease, see Chapter 4. When dietary measures are really insufficient, loperamide may be taken temporarily during breastfeeding. However, the essential oil could, in individual instances, affect the taste of the milk and lead to a (temporary) nursing strike. Dimeticon or simeticon and vegetable preparations can be given for flatulence without reservation. Lipid reducers should not be used during breastfeeding because their safety is not established, and there would seem to be no disadvantage for the mother when therapy is stopped during pregnancy and breastfeeding. Taking the medication, however, does not require any limitation of breastfeeding, although, with the exception of colestipol, cholestyramine, and pravastatin, the continuation of treatment should be critically reviewed. Chenodeoxycholic acid and ursodeoxycholic acid should not be used while breastfeeding. Only limited amounts of ursodeoxycholic acid appear in the blood circulation, where they are overwhelmingly bound to albumin. Lactation Pravastatin appears only in negligible amounts in the milk (less than 0. No toxic effects on the infant have been reported as yet in connection with maternal intake of lipid reducers. However, the documented experience with acipimox, atorvastatin, bezafibrate, cerivastatin, clofibrate, colestipol, cholestyramine, etofibrate, etofyllinclofibrate, ezetimibe, fenofibrate, fluvastatin, gemfibrozil, inositol nicotinate, lovastatin, pitavastatin, pravastatin, probucol, rosuvastatin, simvastatin, -sitosterin, and xantinol nicotinate is insufficient for a risk assessment. Due to the way they work, the lipid-binding resins colestipol and cholestyramine, which are not absorbed in significant amounts, are not considered to pose a risk to the breastfed infant. The accidental intake of a single dose does not require limitation of breastfeeding. Very rarely, mild restlessness, sedation or weak sucking none of which require treatment have been described in the breastfed infant (see, for example, Moretti 1995). The brief half-life of 23 hours and the long effectiveness of up to 24 hours argue for good tolerance of meclizine during pregnancy. Even with the other, older antiemetics, including the phenothiazine-neuroleptics which are used for this purpose, severe intolerance in the infant especially after single dosages would not be expected. If a serotonin antagonist such as ondansetron is indicated during lactation, the child should be observed for unexpected symptoms.
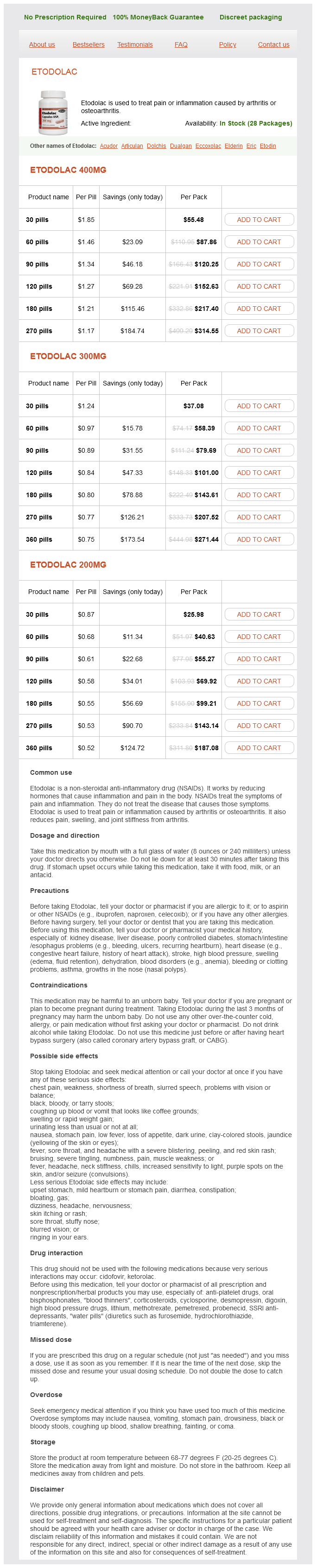
Etodolac Dosage and Price
Etodolac 400mg
- 30 pills - $55.48
- 60 pills - $87.86
- 90 pills - $120.25
- 120 pills - $152.63
- 180 pills - $217.40
- 270 pills - $314.55
Etodolac 300mg
- 30 pills - $37.08
- 60 pills - $58.39
- 90 pills - $79.69
- 120 pills - $101.00
- 180 pills - $143.61
- 270 pills - $207.52
- 360 pills - $271.44
Etodolac 200mg
- 30 pills - $25.98
- 60 pills - $40.63
- 90 pills - $55.27
- 120 pills - $69.92
- 180 pills - $99.21
- 270 pills - $143.14
- 360 pills - $187.08
Hansen (2005) arthritis treatment for dogs order generic etodolac on line, in a randomized double-blind study, investigated more than 60 mothers of preterm newborns, who received either metoclopramid or placebo. There were no significant differences with respect to the amount of milk and duration of lactation period. Other reports observed its successful use in, for example, the context of lactation stimulation in a woman with agenesis of the uterus. Although her pregnancy was carried by another woman, she wanted to breastfeed her child. Therefore, she started with 3 10 mg metoclopramide from week 28 until delivery (of the host-mother), and stimulated the nipples with an electric milk pump. The effect of this method was confirmed by serum prolactin and estradiol measures. She was ultimately able to breastfeed her child until 3 months of age; however formula was used as a supplement because of insufficient milk production (Biervliet 2001). A double-blind study of mothers of preterm babies, 7 on domperidone and 9 on placebo, found an average 4. A high molecular mass of about 426 and protein binding of 90% are grounds for a low relative dose to the breastfed child. In comparison to metoclopramid, domperidone is less able to cross the bloodbrain barrier. A recent discussion on cardiac arrest associated with domperidone was based on events following high intravenous dosages, which is not comparable with the drug transfer to a breastfed child. Domperidone, metoclopramide, and cisapride may be used for appropriate indications. The short-term use of other medications does not require limitation of breastfeeding. When using pyridostigmine, with a half-life of about 4 hours, the infant receives a maximum of 0. In the case of two unremarkable infants described, there was no active ingredient found in their serum (detection level 2 g/l). Maternal serum concentrations were 25 and 80 g/l; a maximum of 25 g/l was found in the milk with intravenous application of 300 mg/day pyridostigmine (Hardell 1982). The usual short-term therapy for (postoperative) atony of the intestine or bladder, or treatment of myasthenia with cholinergics, is permissible while breastfeeding. However, there have been no publications, as yet, in which negative effects on the baby have been described as a result of giving atropine-like drugs to a breastfeeding mother. Butylscopolamine appears to be well-tolerated by the breastfed infant, either as a single parenteral dose or with repeated oral or rectal administration. Experience with other anticholinergics such as butinolin, denaverin, glycopyrrolate bromide, hymecromon, mebeverine, methanthelinium, oxybutynin, phenamazide, pipenzolate, pipoxolan, tiropramide, tolterodine, trospium chloride, and valethamate bromide is insufficient with respect to breastfeeding. In the case of bladder incontinence, oxybutynin, which is equally widely used, also seems to be acceptable. Induction of lactation in the intended mother of a surrogate pregnancy: case report. Disposition of 5-aminosalicylic acid and N-acetyl-5-aminosalicylic acid preparations. Effect of domperidone on milk production in mothers of premature newborns: a randomized, double-blind, placebo-controlled trial. Prospective follow-up of adverse reactions in breast-fed infants exposed to maternal infection. Metoclopramide and breast-feeding: efficacy and anterior pituitary responses of the mother and the child. Omeprazole for refractory gastroesophageal reflux disease during pregnancy and lactation. Thus, in any case, only minimal concentrations are reached in the infant plasma, and in no case is a concentration reached that would inhibit bacterial growth. The following risks have been discussed repeatedly in the literature: Effects on the intestinal flora (with diarrhea as a possible consequence) Effects on bacteriological studies which might be necessary in case the infant falls ill Development of bacterial resistance Sensitization. The likeliest possibility in rare cases would be a temporary loosening of the stool consistency, which does not require any therapy (Ito 1993). As a rule, the exclusively breastfed infant receives considerably less than 1% of a therapeutic dosage (survey in Bennett 1996). This applies similarly to cephalosporins, which are, to some extent, inactivated in the intestine (survey in Bennett 1996). Benyamini and co-workers asked 67 mothers who were taking amoxicillin plus the enzyme inhibitor clavulanic acid, as well as 38 who were taking cefuroxim, about side effects in their breastfed children (Benyamini 2005). With cefuroxim and cefalexin, only moderate side effects were reported and in scarcely 3% of cases. With sulbactam, the relative daily dosage transmitted was a maximum of 1% (Foulds 1985). This provides additional support for limited bioavailability to the breastfed child. Other -lactam antibiotics have not as yet been shown to be toxic for the breastfed infant. Penicillin derivatives and cephalosporins are the antibiotics of choice during breastfeeding. With 500 mg/daily of clarithromycin, used to treat a puerperal infection, a maximum of 1. There are no reports of specific intolerance during breastfeeding to any of the macrolides mentioned here.