Eurax
General Information about Eurax
Like all drugs, Eurax comes with a threat of unwanted effects, though they do not appear to be very common. The commonest unwanted effects embody pores and skin irritation, redness, or a burning sensation at the application website. In very rare cases, it can trigger an allergic response, so it is important to discontinue use and search medical attention if any surprising signs occur.
Eurax is classed as a scabicidal and antipruritic medicine, which means it kills scabies mites and relieves itchiness. It works by affecting the nervous system of the mites, paralyzing and killing them. It additionally has an area anesthetic effect, which helps to soothe the itchy pores and skin.
In common, Eurax is taken into account a protected and effective therapy for scabies and other skin circumstances. However, it's important to use it as directed and observe good hygiene practices, similar to washing clothes, bedding, and towels in sizzling water, to forestall the spread of scabies and recurrence of the condition.
Aside from treating scabies, Eurax is also used as a secondary treatment for different pores and skin conditions, such as eczema, dermatitis, and bug bites, to alleviate itching and irritation. It is on the market over-the-counter in most pharmacies, and a well being care provider's prescription just isn't required to buy it.
Scabies is very contagious, and it could possibly spread shortly through shut physical contact. It is often acquired by way of skin-to-skin contact with an infected particular person or by sharing bedding, towels, or clothing. The first signs of scabies typically seem within a couple of weeks of preliminary publicity, and the most typical symptom is intense itching, particularly at night time. Other signs may embody a rash, tiny blisters, or sores on the pores and skin.
Eurax, also identified by its generic name Crotamiton, is a topical medication commonly used for treating scabies and relieving itching. Scabies is a skin condition brought on by tiny mites that burrow into the skin and lay eggs, causing intense itching and irritation.
In conclusion, Eurax is an antipruritic and scabicidal medicine extensively used for treating scabies and relieving itching. It works by killing scabies mites and soothing the pores and skin. It is out there over-the-counter, and whereas it's usually protected and effective, it is essential to comply with correct utility and hygiene guidelines. If you think you have scabies, consult a healthcare professional for correct analysis and remedy, together with the use of Eurax.
If left untreated, scabies can result in a secondary infection, similar to impetigo or cellulitis, which could be more extreme. Therefore, it is crucial to hunt prompt remedy as quickly as scabies is suspected. European pointers advocate utilizing Eurax because the first-line therapy for scabies, as a outcome of its effectiveness and low risk of unwanted effects.
Eurax is available in a lotion or cream form and is utilized to the complete body, from the neck down, excluding the face. It is important to wash the medication off after 24 hours and repeat the applying in seven days to ensure all the mites are killed. The medicine is not recommended to be used in kids underneath three years old, pregnant or breastfeeding ladies, or folks with known allergy symptoms to any of its components.
The most accurate way to correct hyponatremia entails a detailed registry matching total solute and water output with desired input skin care 30s discount generic eurax uk. This formula does not account for ongoing electrolyte or water losses and is only a rough guide. Dividing the desired rate of correction (mEq/L/h) by [Na+] (mEq/L/L of fluid) gives you the appropriate rate of administration (liter of fluid per hour). Because this equation does not account for ongoing losses, one must recheck laboratory data and adjust fluid rates to make sure the patient is improving appropriately. Rate of correction: She has symptomatic hyponatremia requiring an acute correction (1-2 mEq/L/h for the first 3-4 hours) but no more than 12 mEq/L corrected over 24 hours. Means of correction: Given the acuity, the patient should be given hypertonic saline, which has 513 mEq of Na+ per liter. Rate = (2 mEq/L/h) ÷ (10 mEq/L per 1 L of saline) To prevent a change of >10-12 mEq/L over 24 hours, no more than 1 L of fluid should be given. In patients with asymptomatic hypovolemic hyponatremia, isotonic saline can be used to restore the intravascular volume. Restoration of a euvolemic state will reduce the impetus toward renal water retention, leading to normalization of [Na+]. If the duration of hyponatremia is unknown, the process described earlier can be used to calculate the expected change from 1 L of 0. Although effective circulating volume is decreased, the administration of fluid P. Definitive treatment requires management of the underlying condition, although restriction of water intake and increasing water diuresis may help to attenuate the degree of hyponatremia. Urinary excretion of water can be promoted through the use of loop diuretics, which reduce the concentration gradient necessary to reabsorb water in the distal nephron. When using medications to promote water loss, laboratory data and volume status must be followed extremely closely, because the effect on water and electrolyte loss cannot be accurately predicted. The standard first-line therapy is water restriction and correction of any contributing factors (nausea, pneumonia, drugs, etc. If this fails or if the patient is symptomatic, the following can be attempted to promote water excretion. The amount of fluid restriction necessary depends on the extent of water elimination. A useful guide to the necessary degree of fluid restriction is as follows: If (Urine Na+ + Urine K+)/Serum Na+ <0. If (Urine Na+ + Urine K+)/Serum Na+ is >1, the patient has a negative renal free water clearance and is actively reabsorbing water. Any amount of water given may be retained, and clinicians should consider the following options to enhance free water excretion. The volume of water excreted as urine is governed by a relatively fixed urine osmolality. Thus, increasing solute intake with a high-salt, high-protein diet or administration of oral urea (30-60 g) may increase the capacity for water excretion and improve the hyponatremia. Loop diuretics impair the urinary concentrating mechanism and can enhance free water excretion. However, given the risks of overcorrection, these agents should be initiated in a closely monitored inpatient setting. They should only be considered in severe hyponatremia that is unresponsive to more conservative measures. Hypernatremia may be caused by a primary Na+ gain or a water deficit, the latter being much more common. Normally, this hyperosmolar state stimulates thirst and the excretion of a maximally concentrated urine. For hypernatremia to persist, one or both of these compensatory mechanisms must be impaired. Impaired thirst response may occur in situations where access to water is limited, often due to physical restrictions (institutionalized, handicapped, postoperative, or intubated patients) or mental impairment (delirium, dementia). The loss of water must occur in excess of electrolyte losses in order to raise [Na+]. Osmotic diarrhea (induced by lactulose, sorbitol, or malabsorption of carbohydrate) and viral gastroenteritis, in particular, result in disproportional water loss. In addition, increased urea generation from accelerated catabolism, high-protein feeds, and stress-dose steroids can also result in an osmotic diuresis. The latter often results from a disruption to the renal concentrating mechanism due to drugs (lithium, demeclocycline, amphotericin), electrolyte disorders (hypercalcemia, hypokalemia), medullary washout (loop diuretics), and intrinsic renal diseases. However, it can rarely occur after repetitive hypertonic saline administration or chronic mineralocorticoid excess. Thus, the most severe symptoms of hypernatremia are neurologic, including altered mental status, weakness, neuromuscular irritability, focal neurologic deficits, and, occasionally, coma or seizures. As with hyponatremia, the severity of the clinical manifestations is related to the acuity and magnitude of the rise in plasma [Na+]. Chronic hypernatremia is generally less symptomatic as a result of adaptive mechanisms designed to defend cell volume. Signs of volume depletion or neurologic dysfunction are generally absent unless the patient has an associated thirst abnormality. The appropriate renal response to hypernatremia is a small volume of concentrated (urine osmolality >800 mOsm/L) urine.
Haemosiderin is an insoluble proteiniron complex of varying composition containing approximately 37% iron by weight acne around chin discount eurax 20 gm online. A coppercontaining enzyme, caeruloplasmin, catalyses oxidation of the iron to the ferric form for binding to plasma transferrin. Iron is also present in muscle as myoglobin and in most cells of the body in ironcontaining enzymes. This tissue iron is less likely to become depleted than haemosiderin, ferritin and haemoglobin in states of iron deficiency, but some reduction of these haemcontain ing enzymes may occur. Amount of iron in average adult Haemoglobin Ferritin and haemosiderin Myoglobin Haem enzymes. Most of the iron in the body is contained in circulating haemoglobin (see Table 3. Iron is transferred from macrophages to plasma transferrin and so to bone marrow erythroblasts. When plasma iron is raised and transferrin is saturated, the amount of iron transferred to parenchymal cells. There may also be free iron in plasma which is toxic to different organs (see Chapter 4). In iron defi ciency, increased matriptase activity therefore results in decreased hepcidin synthesis. Iron is present in food as ferric hydroxides, ferricprotein and haemprotein complexes. Both the iron content and the pro portion of iron absorbed differ from food to food; in general meat, in particular liver, is a better source than vegetables, eggs or dairy foods. The average Western diet contains 1015 mg iron daily from which only 510% is normally absorbed. The proportion can be increased to 2030% in iron deficiency or pregnancy (Table 3. Iron absorption Organic dietary iron is partly absorbed as haem and partly broken down in the gut to inorganic iron. Haem is absorbed through a receptor, yet to be identified, on the apical membrane of the duodenal enterocyte. Inorganic iron absorption is favoured by factors such as acid and reducing agents that keep iron in the gut lumen in the Fe2+ rather than the Fe3+ state (Table 3. Raised hepcidin levels therefore profoundly affect iron metabolism by reducing its absorption and release from macrophages. Its synthesis is increased by transferrin saturation and inflammation but reduced by increased erythropoiesis, erythropoietin, hypoxia and matriptase. Ferroportin at the basolateral surface con trols exit of iron from the cell into portal plasma. Ferrireductase present at the apical surface converts iron from the Fe3+ to Fe2+ state and another enzyme, hephaestin (ferrioxidase), converts Fe2+ to Fe3+ at the basal surface prior to binding to transferrin. Therefore these groups are particularly likely to develop iron deficiency if there is additional iron loss or pro longed reduced intake. Causes of iron deficiency In developed countries, chronic blood loss, especially uterine or from the gastrointestinal tract, is the dominant cause of iron deficiency (Table 3. Five hundred millilitres of blood contain approximately 250 mg iron and, despite the increased absorption of food iron at an early stage of iron deficiency, neg ative iron balance is usual in chronic blood loss. Increased demands during infancy, adolescence, preg nancy, lactation and in menstruating women account for the high risk of iron deficiency anaemia in these particular clini cal groups. Newborn infants have a store of iron derived from delayed clamping of the cord and the breakdown of excess red cells. From 3 to 6 months there is a tendency for negative iron balance because of growth. From 6 months, supplemented formula milk and mixed feeding, particularly with ironforti fied foods, prevents iron deficiency. In pregnancy increased iron is needed for an increased maternal red cell mass of approximately 35%, transfer of 300 mg of iron to the fetus and because of blood loss at deliv ery. Although iron absorption is also increased, iron therapy is often needed if the haemoglobin (Hb) falls below 100 g/L Iron deficiency Clinical features When iron deficiency is developing, the reticuloendothe lial stores (haemosiderin and ferritin) become completely depleted before anaemia occurs. As the condi tion develops, the patient may show the general symptoms and signs of anaemia (see p. The cause of the epithelial cell changes is not clear but may be related to reduction of ironcontaining enzymes. In children, iron deficiency is particularly significant as it can cause irritabil ity, poor cognitive function and a decline in psychomotor development. There is also evidence that oral or parenteral iron may reduce fatigue in irondeficient (low serum ferritin) nonanaemic women. Urine, sweat, faeces Adult male Postmenopausal female Menstruating female* Pregnant female* Children (average) Female (age 1215)* 0. Reticuloendothelial (macrophage) stores are lost completely before anaemia develops. Menorrhagia (a loss of 80 mL or more of blood at each cycle) is difficult to assess clinically, although the loss of clots, the use of large numbers of pads or tampons or prolonged periods all suggest excessive loss. It takes about 8 years for a normal adult male to develop iron deficiency anaemia solely as a result of a poor diet or malabsorption resulting in no iron intake at all. In developed countries inadequate intake or malabsorption are only rarely the sole cause of iron deficiency anaemia. Gluteninduced enteropathy, partial or total gastrectomy and atrophic gastritis (often autoimmune and with Helicobacter pylori infection) may, however, predispose to iron deficiency. In developing coun tries, iron deficiency may occur as a result of a lifelong poor diet, consisting mainly of cereals and vegetables. Hookworm Gluteninduced enteropathy, gastrectomy, autoimmune gastritis Poor diet A major factor in many developing countries but rarely the sole cause in developed countries may aggravate iron deficiency, as may repeated pregnancies or growth and menorrhagia in young females.
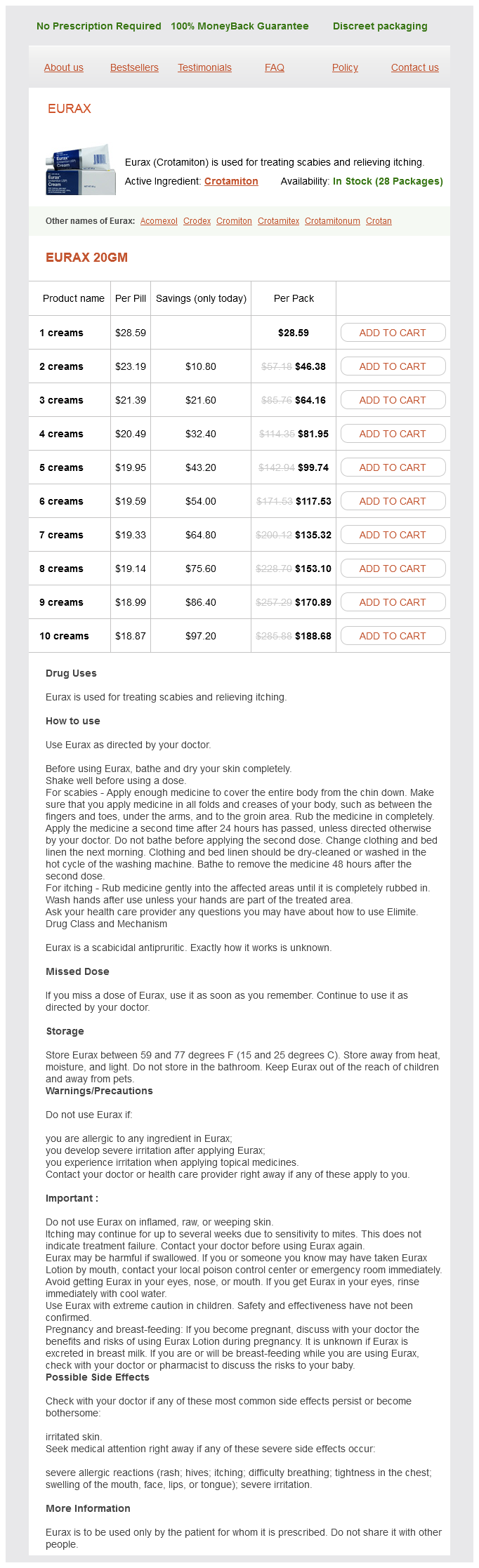
Eurax Dosage and Price
Eurax 20gm
- 1 creams - $28.59
- 2 creams - $46.38
- 3 creams - $64.16
- 4 creams - $81.95
- 5 creams - $99.74
- 6 creams - $117.53
- 7 creams - $135.32
- 8 creams - $153.10
- 9 creams - $170.89
- 10 creams - $188.68
Mild degrees of volume depletion are often not clinically detectable acne vulgaris cause eurax 20 gm purchase on-line, whereas larger fluid losses can lead to mental status changes, oliguria, and hypovolemic shock. Diagnostic Testing Laboratory studies are often helpful but must be used in conjunction with the clinical picture. Urine Na+ <15 mEq is consistent with volume depletion, as is a fractional excretion of sodium (FeNa) <1%. The latter can be calculated as ([Urine Na+ × Serum Cr] ÷ [Urine Cr × Serum Na+]) × 100. Concomitant metabolic alkalosis may increase urine Na+ excretion despite volume depletion due to obligate excretion of Na+ to accompany the bicarbonate anion. In such cases, a urine chloride of <20 mEq is often helpful to confirm volume contraction. In patients with symptomatic volume depletion, a 1- to 2-L bolus is often preferable to acutely expand the intravascular space. The bolus can be repeated if necessary, although close attention should be directed toward possible signs of volume overload. Smaller boluses should be used for patients with poor cardiac reserve or significant edema. Once the patient is stable, fluids can be administered at a maintenance rate to replace ongoing losses. The Hypervolemic Patient the clinical manifestations of hypervolemia result from a surplus of total body Na+. Alternatively, it may be secondary to decreased effective circulating volume, as in heart failure, cirrhosis, or profound hypoalbuminemia. Expansion of the intravascular compartment may result in pulmonary rales, elevated jugular venous pressure, hepatojugular reflux, an S3 gallop, and elevated blood pressures. Because overt signs of hypervolemia may not manifest until 3-4 L of fluid retention, a gradual rise in water weight is often the earliest indication of Na+ retention. Diagnostic Testing Laboratory studies are generally not needed, and hypervolemia is primarily a bedside diagnosis. The urine [Na+] may be low (<15 mEq/L) with decreased effective circulating volume reflecting renal sodium retention. Alleviating the Na+ excess can be accomplished by the judicious use of diuretics and by limiting Na+ intake. Medications Diuretics enhance the renal excretion of Na+ by blocking the various sites of Na+ reabsorption along the nephron. Because of their specific site of action, thiazide diuretics impair urinary dilutional capacity (the ability to excrete water) and often stimulate a responsive increase in proximal tubule reabsorption. Loop diuretics block the Na+-K+-2Cl- transporter in the thick ascending loop of Henle. They are often used in circumstances requiring a brisk and immediate diuresis, such as acute volume overload. Loop diuretics impair urinary concentration (increase renal free water excretion) and enhance the excretion of divalent cations (Ca2+ and Mg2+). Potassium-sparing diuretics act by decreasing Na+ reabsorption in the collecting duct. Although the overall diuretic effect of these agents is comparatively small, they serve as useful adjunctive agents. Furthermore, because aldosterone antagonists do not require tubular secretion, they can be particularly useful in those with decreased renal perfusion or impaired tubular function. Treatment of the underlying disease process is critical to prevent continued Na+ reabsorption in the kidney. Treatment of heart failure is discussed in Chapter 5, Heart Failure and Cardiomyopathy, and cirrhosis is addressed in Chapter 19, Liver Diseases. Disorders of Sodium Concentration Hypernatremia and hyponatremia are primarily disorders of water balance or water distribution. The body is designed to withstand both drought and deluge with adaptations to renal water handling and the thirst mechanism. A persistent abnormality in [Na+] thus requires both an initial challenge to water balance as well as a disturbance of the adaptive response. Any process that limits the elimination of water or expands the volume around a fixed Na+ content may lead to a decrease in Na+ concentration. This is most commonly caused by hyperglycemia, resulting in a fall in plasma [Na+] of 1. Prompt renal excretion and metabolism of the absorbed fluid usually corrects the hyponatremia rapidly, although symptomatic hyponatremia can occasionally be seen in the setting of renal insufficiency. This is seen in psychogenic polydipsia, water intoxication from poorly conceived drinking games, beer potomania, and the so-called "tea and toast" diet. Underlying each of these circumstances is the fact that there is a limit to renal water clearance. Urine cannot be diluted to an osmolality less than approximately 50 mOsm/L, meaning that a small amount of solute is required in even the most dilute urine. Ingestion of a high volume of water can thus exceed the capacity for excretion, particularly in those with a solute-poor diet, because the solute load required to generate urinary water loss is quickly depleted. Decreased clearance of water from the kidney can also occur through a variety of processes. Although this seems counterintuitive from an osmotic standpoint (it further reduces renal water clearance and increases water retention), it is an "appropriate" adaptive response to the threat of volume loss, tissue hypoperfusion, and impending hemodynamic collapse.