Exelon
General Information about Exelon
In conclusion, Exelon is a vital medication in the treatment of mild to average dementia, notably in patients with Alzheimer's illness and Parkinson's illness. It works by helping to spice up the levels of a vital chemical within the mind, leading to improvements in cognitive perform and daily activities. While it may not be a remedy for dementia, Exelon has been shown to effectively handle its symptoms and improve the quality of life for patients. As with any treatment, it's essential to make use of Exelon beneath the guidance of a healthcare skilled, and patients and caregivers should be vigilant in monitoring for any potential unwanted aspect effects.
Like any medicine, Exelon could cause some side effects, corresponding to nausea, vomiting, and loss of urge for food. However, these unwanted side effects are sometimes delicate and may be managed with the assistance of a well being care provider. It is crucial to debate any potential allergic reactions or medical circumstances with a healthcare skilled earlier than starting this treatment.
One of essentially the most important benefits of Exelon is that it may possibly assist delay the development of these conditions and enhance the quality of life for sufferers. In clinical trials, sufferers who took Exelon skilled a major improvement in cognitive perform, main to better reminiscence, judgement, and day by day functioning. This medication has additionally been shown to minimize behavioral and psychological signs, such as agitation and aggression, which could be challenging for caregivers to handle.
For elderly patients with dementia, the use of Exelon requires careful management and monitoring. It is essential to coach sufferers and caregivers in regards to the medication's proper use, potential unwanted facet effects, and potential interactions with other medicine. Patients should also be advised to seek medical assist if they experience any new or worsening symptoms.
Exelon is a broadly used medicine in the therapy of dementia, a situation that affects hundreds of thousands of people worldwide. It is designed to help handle the signs of Alzheimer's illness and Parkinson's disease, two of the most common forms of dementia. In this article, we will discover what Exelon is, how it works, and why it is a crucial treatment possibility for these affected by these debilitating conditions.
The dosage of Exelon varies depending on the severity of the affected person's situation, and it's often administered orally in the type of capsules or a liquid solution. It is important to comply with the dosage instructions offered by a healthcare professional and not to change or cease the treatment without consulting a physician. Patients are additionally suggested to take Exelon with meals to attenuate gastrointestinal unwanted facet effects.
Exelon, also identified by its generic name Rivastigmine, falls under the category of cholinesterase inhibitors. It works by rising the degrees of a naturally occurring chemical in the brain called acetylcholine. This chemical is vital for reminiscence and other cognitive functions, and in individuals with dementia, its levels are often depleted. By inhibiting the breakdown of acetylcholine, Exelon helps to take care of its ranges and improve the communication between nerve cells, main to better cognitive perform.
Primarily used for treating delicate to average dementia, Exelon is prescribed to those who are affected by signs similar to reminiscence impairment, problems with summary pondering, changes in persona, and difficulty with daily activities. These signs are often related to Alzheimer's disease, a condition that impacts an estimated 5.8 million Americans, and Parkinson's illness, which impacts over 1 million Americans.
Because of these characteristics medicine used for adhd exelon 6 mg buy free shipping, ketamine, similarly to etomidate, is an appropriate choice for a patient with hemodynamic compromise. However, large doses can cause uterine hypertonia, which may result in decreased uterine perfusion. Inhaled Anesthetics Succinylcholine is frequently used with general anesthesia in obstetric patients, as it has a rapid onset and short duration. Larger doses of 2 to 3 mg/kg may result in detectable levels of succinylcholine in the umbilical cord. Although levels of Butyrylcholinesterase (pseudocholinesterase), the enzyme that hydrolyzes succinylcholine, are decreased during pregnancy, neuromuscular blockade is not significantly prolonged. Side effects are the same as those seen in the nonpregnant population and include increased maternal potassium levels and myalgia. Like halogenated anesthetic gases, succinylcholine is a known triggering agent for malignant hyperthermia. This fast-acting nondepolarizing agent achieves intubating conditions in 60 to 90 seconds when used at doses of 1. However, the duration of action of rocuronium is much longer than that of succinylcholine, which can be a safety concern if one is unable to ventilate or intubate the patient. Maintenance of muscular relaxation is normally not required for cesarean delivery but can be achieved using a variety of nondepolarizing neuromuscular blockers, such as rocuronium, vecuronium, cis-atracurium, and so on. As a class, these medications are highly ionized and poorly lipid-soluble, and therefore they do not cross the placenta in significant amounts when given within normal dosing parameters. When extremely large and repeated doses are used, neonatal neuromuscular blockade may be seen secondary to these medications crossing the placenta. Reversal of a nondepolarizing muscle relaxant should be considered at the end of every cesarean delivery performed with general anesthesia and muscular relaxation. Standard options include coadministration of glycopyrrolate and neostigmine for reversal of neuromuscular blockade. If administered at the completion of a cesarean delivery, placental transfer of these drugs is irrelevant. If these medications are administered to a pregnant patient undergoing nonobstetric surgery, however, placental transfer must be considered. Glycopyrrolate, an ionized quaternary ammonium compound, is poorly transferred across the placenta. Neostigmine is also an ionized quaternary ammonium compound, but it is smaller than glycopyrrolate and more capable of crossing the placenta. Although this combination is frequently administered to pregnant women for reversal without adverse effect, there have been case reports of profound fetal bradycardia when glycopyrrolate and neostigmine were coadministered. Sugammadex has been used safely for reversal of neuromuscular blockade with rocuronium after completion of cesarean deliveries. According to the pharmaceutical package insert, nonpregnant women using oral contraceptives containing estrogen or progestogen who receive sugammadex should be instructed to use an additional, nonhormonal method of contraception for 7 days after sugammadex administration. Sugammadex binds to Reversal Agents Nitrous oxide is often used as a component of maintenance for general anesthesia, as it has minimal effects on maternal hemodynamics or uterine tone. It rapidly crosses the placenta, but the effects of nitrous oxide on neonates is negligible. Isoflurane, sevoflurane, and desflurane are all non-ionized agents, lipid-soluble, have a low molecular weight, and therefore easily cross the placenta. Although general anesthesia is typically used when an emergent cesarean delivery is required. If the depressed status of a neonate is secondary to anesthetic medications, the newborn should rapidly improve with basic ventilation and standard resuscitation measures. If no improvement is noted, other causes of their depressed status should be investigated. A Cochrane review examined fetal outcomes after uncomplicated cesarean delivery with neuraxial or general anesthesia. With routine use of neuraxial opioids and scheduled non-opioid analgesics, the amount of post-cesarean delivery systemic opioids needed to achieve postcesarean delivery pain control is declining. Systemic opioids should be provided on an as-needed basis to treat breakthrough pain after cesarean delivery, with patients receiving scheduled doses of nonsteroidal antiinflammatory drugs and acetaminophen in addition to analgesia from intrathecal morphine. It is safe for mothers to breastfeed with standard prescribed doses of opioids used for treatment of postoperative pain after cesarean section. However, caution and appropriate consultation are recommended for mothers requiring larger doses of opioids. Codeine is best avoided in breastfeeding mothers, as there is significant transfer to the breast milk and infants with specific genetic polymorphisms are at increased risk of significant respiratory depression. The patient should be transitioned to scheduled oral ibuprofen for continuation of the benefits from a nonsteroidal antiinflammatory pain regimen. A study examining the role of scheduled acetaminophen with as-needed opioids versus as-needed acetaminophen/opioid combination tablets found that scheduled acetaminophen resulted is less total opioid consumption. Avoiding opioid/acetaminophen combination medication reduces unnecessary opioid use and helps to avoid exceeding recommended maximum doses of acetaminophen. There is some evidence to suggest improved pain scores as well as maternal satisfaction with a single 600-mg preoperative dose, but these findings have been inconsistent and there is a high level of fetal transfer. Consequently, gabapentin is not commonly used for postcesarean delivery pain unless the patient has a history of chronic pain. Systemic Opioid and Non-Opioid Analgesics Antiemetics Nausea is an extremely common symptom, affecting about 80% of pregnant women. First-line medications include ginger, pyridoxine (vitamin B6), or antihistamines for mild symptoms. For moderate symptoms, options include pyridoxine/ doxylamine combinations, dopamine antagonists such as metoclopramide, or serotonin antagonists such as ondansetron.
Questions exist about the efficacy of the mechanical effect owing to the lateral displacement of the esophagus medicine 5325 purchase 3 mg exelon with mastercard, which is exacerbated by posterior pressure on the cricoid cartilage. Despite little evidence supporting benefit, the use of cricoid pressure is well entrenched. Because it can worsen the view with laryngoscopy, it should be abandoned if difficulties with intubation or ventilation are encountered. May present and/or strong peristaltic with toxic motility megacolon Increased motility of Intravenous fluid to intestinal wall replace fluid and Increased quantity of fluid electrolytes as rapidly as lost Increased motility Excess secretion of mucus in distal colon Repeated diarrheal bowel movements Ileostomy to heal ulcers or Surgical removal of entire colon Disorders of large intestine Megacolon (Hirschsprung disease) Diarrhea Severe constipation Lack or deficiency of ganglion cells in myenteric plexus in a segment of the sigmoid colon Enteritis: inflammation of intestinal tract caused by either virus or bacteria. Vagal and sympathetic afferent nerves can activate the chemoreceptor trigger zone and vomiting center, located in the medulla close to the area postrema and fourth ventricle. Neurotransmitters involved include acetylcholine, dopamine, histamine, substance P, and serotonin. Clinical risk factors for postoperative nausea and vomiting include female gender, nonsmoking status, history of motion sickness, perioperative opioid use, and use of inhaled anesthetics (see Chapter 34). Emerging Developments Tissue Engineering End-stage liver disease from any cause dramatically alters liver physiology and microanatomy. Currently the only curative therapy for end-stage liver disease is orthotopic liver transplantation. Advances in molecular biology, stem cell biology, and tissue bioengineering focused on hepatology have resulted in exciting new possibilities to repair or replace damaged liver tissue and thereby restore normal hepatic physiology. The nucleus of a mature cell, such as a fibroblast, can be "reprogrammed" by exposure to certain transcription factors to an undifferentiated state. Although in a preliminary stage, these techniques have shown promise in animal models. Similarly, automated engineering platforms emulating standard three-dimensional printer technology can be used to design and develop three-dimensional tissue configurations of various cell types, including cell structures that resemble liver tissue in terms of how the hepatocytes are organized in space relative to other cells types. These "biomanufactured" tissues have exciting potential in the quest to develop artificial "whole" livers for transplantation. The result is an organ with specified genetic characteristics within an animal host. The technique has been applied successfully in animal models for the pancreas and kidney. A key limitation in creating a potentially unlimited pool of donor organs from genetically modified animals (pigs in the case of liver transplantation) has been the fear of transmitting retroviruses to humans. Succinylcholine mimics the effect of acetylcholine at the neuromuscular junction, producing an initial muscle contraction that is clinically evident as fasciculation (see Chapter 22). Fasciculation is associated with increased intragastric pressure, potentially sufficient to overcome the lower esophageal sphincter and result in reflux of gastric contents with possible aspiration. Prevention of fasciculation with the use of a "defasciculating" or subparalytic dose of a nondepolarizing neuromuscular blocking agent might prevent or reduce the increase in intragastric pressure. Scopolamine is used primarily for its central effects, whereas atropine and glycopyrrolate are more commonly used for their peripheral effects. Opioid-induced biliary spasm can confound diagnosis of cardiac disease and might also be misinterpreted as a biliary stone or stricture on cholangiogram. Opioids also cause pancreatic duct contraction, releasing pancreatic amylase and lipase and also potentially confounding a diagnosis of pancreatitis; however, the clinical significance of these effects has been challenged. Alvimopan, a peripherally acting µ-opioid receptor antagonist that does not cross the blood-brain barrier, has been shown to decrease both symptoms and hospital length of stay without compromising pain relief. The cell source for liver repopulation (A) and liver engineering (B) should be facilitated by an unlimited supply of induced pluripotent stemderived hepatocytes, but the underlying tumor potential would remain to be elucidated. Successful liver repopulation will require optimizing functional hepatic cells to achieve high engraftment and repopulation efficiency. Important health and ethical issues associated with blastocyst complementation (D) will need to be addressed. The liver may contain host cells and pathogens that could pose a threat of immunologic rejection and transmission of interspecies diseases. Ethical concerns could be solved once the genetic toolbox makes it possible to restrict differentiation toward particular organs (brain and gonads). Altered liver function can lead to encephalopathy and alter the metabolism, volume of distribution, and protein binding of drugs. A recent review describing liver disease-related contraindications to elective surgery. Reports the effects of a number of risk factors on short- and long-term perioperative mortality of 733 patients with cirrhosis. Mechanism and role of intrinsic regulation of hepatic arterial blood flow: hepatic arterial buffer response. Hemodynamic and organ blood flow responses to halothane and sevoflurane anesthesia during spontaneous ventilation. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Hepatic venous pressure gradient and prognosis in patients with acute variceal bleeding treated with pharmacologic and endoscopic therapy. Long-duration lowflow sevoflurane and isoflurane effects on postoperative renal and hepatic function. Common bile duct pressure changes after fentanyl, morphine, meperidine, butorphanol, and naloxone. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. The new liver allocation system: moving toward evidence-based transplantation policy. Use of serum sodium for liver transplant graft allocation: a decade in the making, now is it ready for primetime Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection.
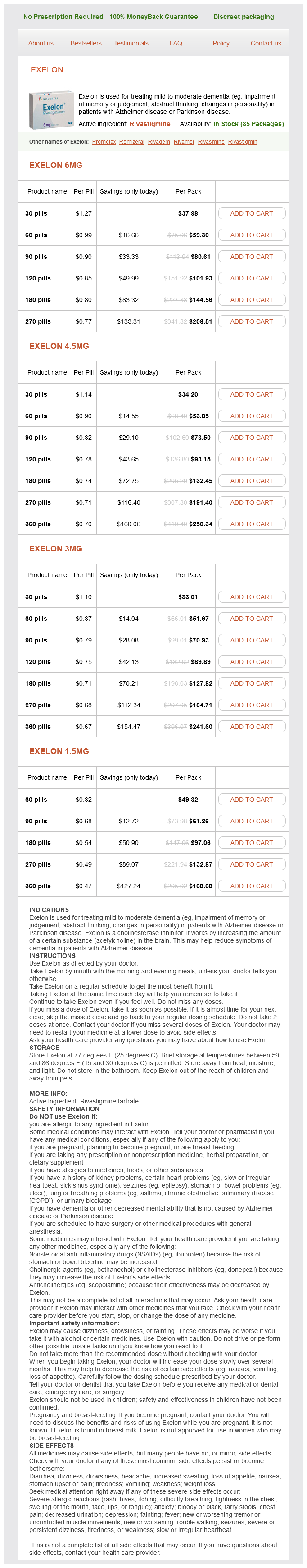
Exelon Dosage and Price
Exelon 6mg
- 30 pills - $37.98
- 60 pills - $59.30
- 90 pills - $80.61
- 120 pills - $101.93
- 180 pills - $144.56
- 270 pills - $208.51
Exelon 4.5mg
- 30 pills - $34.20
- 60 pills - $53.85
- 90 pills - $73.50
- 120 pills - $93.15
- 180 pills - $132.45
- 270 pills - $191.40
- 360 pills - $250.34
Exelon 3mg
- 30 pills - $33.01
- 60 pills - $51.97
- 90 pills - $70.93
- 120 pills - $89.89
- 180 pills - $127.82
- 270 pills - $184.71
- 360 pills - $241.60
Exelon 1.5mg
- 60 pills - $49.32
- 90 pills - $61.26
- 180 pills - $97.06
- 270 pills - $132.87
- 360 pills - $168.68
Inhaled anesthetics and immobility: mechanisms medications descriptions exelon 6 mg mastercard, mysteries, and minimum alveolar anesthetic concentration. Age, Minimum alveolar anesthetic concentration, and minimum alveolar anesthetic concentration-awake. Effect of isoflurane and other potent inhaled anesthetics on minimum alveolar concentration, learning, and the righting reflex in mice engineered to express alpha1 gammaaminobutyric acid type A receptors unresponsive to isoflurane. Gamma-aminobutyric acid type A receptor 3 subunit forebrain-specific knockout mice are resistant to the amnestic effect of isoflurane. Gamma-aminobutyric acid type A receptor alpha 4 subunit knockout mice are resistant to the amnestic effect of isoflurane. Acetylcholine receptors do not mediate the immobilization produced by inhaled anesthetics. Inhibitory effects of isoflurane and nonimmobilizing halogenated compounds on neuronal nicotinic acetylcholine receptors. Depression by isoflurane of the action potential and underlying voltage-gated ion currents in isolated rat neurohypophysial nerve terminals. Isoflurane inhibits synaptic vesicle exocytosis through reduced Ca2+ influx, not Ca2+-exocytosis coupling. Bidirectional modulation of isoflurane potency by intrathecal tetrodotoxin and veratridine in rats. Intrathecal veratridine administration increases minimum alveolar concentration in rats. Isoflurane inhibits multiple voltage-gated calcium currents in hippocampal pyramidal neurons. Isoflurane, but not the nonimmobilizers F6 and F8, inhibits rat spinal cord motor neuron CaV1 calcium currents. An open rectifier potassium channel with two pore domains in tandem cloned from rat cerebellum. The use of the potassium channel activator riluzole to test whether potassium channels mediate the capacity of isoflurane to produce immobility. Contrasting synaptic actions of the inhalational general anesthetics isoflurane and xenon. Two-pore-domain K+ channels are a novel target for the anesthetic gases xenon, nitrous oxide, and cyclopropane. Effects of volatile anesthetics on store-operated Ca(2+) influx in airway smooth muscle. A comparison of sevoflurane with halothane, enflurane, and isoflurane on bronchoconstriction caused by histamine. The effects of diethyl ether, enflurane, and isoflurane at the neuromuscular junction. Isoflurane and sevoflurane interact with the nicotinic acetylcholine receptor channels in micromolar concentrations. Characterization of the interactions between volatile anesthetics and neuromuscular blockers at the muscle nicotinic acetylcholine receptor. Differential effects of isoflurane and propofol on upper airway dilator muscle activity and breathing. Antioxidants prevent depression of the acute hypoxic ventilatory response by subanaesthetic halothane in men. Antioxidants reverse reduction of the human hypoxic ventilatory response by subanesthetic isoflurane. Volatile anesthetic effects on sarcoplasmic reticulum Ca content and sarcolemmal Ca flux in isolated rat cardiac cell suspensions. Activation of the Ca2+ release channel of cardiac sarcoplasmic reticulum by volatile anesthetics. Desflurane-mediated sympathetic activation occurs in humans despite preventing hypotension and baroreceptor unloading. Sensitization of adenylate cyclase by halothane in human myocardium and S49 lymphoma wild-type and cyc- cells: evidence for inactivation of the inhibitory G protein Gi alpha. Evidence that postoperative pain is a mediator of the tumor-promoting effects of surgery in rats. Halothane inhibits T cell proliferation and interleukin-2 receptor expression in rats. Halothane inhibits the intraalveolar recruitment of neutrophils, lymphocytes, and macrophages in response to influenza virus infection in mice. Intraoperative modulation of alveolar macrophage function during isoflurane and propofol anesthesia. Volatile anesthetics differentially affect immunostimulated expression of inducible nitric oxide synthase: role of intracellular calcium. Inhibition of superoxide production and Ca2+ mobilization in human neutrophils by halothane, enflurane, and isoflurane. Formation of trifluoroacetylated protein antigens in cultured rat hepatocytes exposed to halothane in vitro. Biotransformation of halothane, enflurane, isoflurane, and desflurane to trifluoroacetylated liver proteins: association between protein acylation and hepatic injury. Autoantibodies associated with volatile anesthetic hepatitis found in the sera of a large cohort of pediatric anesthesiologists. Long-duration low-flow sevoflurane and isoflurane effects on postoperative renal and hepatic function. Assessment of low-flow sevoflurane and isoflurane effects on renal function using sensitive markers of tubular toxicity. Intrarenal fluoride production as a possible mechanism of methoxyflurane nephrotoxicity.