Exforge
General Information about Exforge
Valsartan, then again, is an angiotensin II receptor blocker (ARB). It specifically targets the AT1 receptors of angiotensin II, a hormone that causes blood vessels to constrict, leading to a rise in blood stress. Valsartan blocks these receptors, preventing the hormone from taking effect, and subsequently, lowering blood pressure.
Combining amlodipine and valsartan in Exforge provides a more sturdy and efficient motion on controlling blood stress in comparability with utilizing either drug alone. It is a perfect instance of synergy, the place the mix of two medicine achieves a extra significant effect than the sum of their individual actions. This makes Exforge the final word selection for patients with hypertension, especially those with severe instances that require a number of medicines.
The advantages of Exforge don't cease at its blood pressure-lowering abilities. It has been found to have a protecting effect on the blood vessels, lowering the chance of growth and development of atherosclerosis, a situation where plaque builds up in the arteries, leading to coronary heart attack and stroke. Exforge also has a useful impact on the guts, improving its function and reducing its workload. This can be attributed to amlodipine, which has been proven to enhance blood move to the center and reduce the workload on the guts muscle.
Moreover, Exforge has fewer side effects in comparability with other antihypertensive medication. Side results corresponding to cough, which are generally related to ACE inhibitors, are not present with Exforge. It also causes less fluid retention, making it suitable for patients with edema, a condition the place extra fluid accumulates in the body's tissues.
Hypertension, commonly often known as high blood pressure, is a silent killer that impacts tens of millions of people worldwide. It is a condition that requires lifelong administration and might put one at risk for severe well being complications such as coronary heart assault, stroke, and kidney illness. As such, having an efficient treatment possibility for hypertension is crucial in preserving it underneath control. Enter Exforge, the mixed antihypertensive that has been making waves within the medical neighborhood.
Amlodipine, one of the parts of Exforge, is a third-generation calcium channel blocker. It works by inhibiting the inflow of calcium ions into the blood vessels and heart muscle cells, which causes the vessels to chill out and widen. This, in flip, reduces the overall resistance of the blood vessels, resulting in a drop in blood stress. Additionally, amlodipine has an extended length of action, which means it stays within the body for an extended interval, providing a sustained impact on blood stress.
In conclusion, Exforge is a potent and efficient medicine for the management of hypertension. It combines the benefits of amlodipine and valsartan, providing a robust and sustained motion on controlling blood pressure. With its added protecting effects on the blood vessels and coronary heart, and a decrease incidence of unwanted effects, it is no wonder that Exforge has become the go-to alternative for physicians in the treatment of hypertension. However, like several treatment, it ought to be taken as prescribed by a healthcare supplier, and common blood stress monitoring is critical to make sure correct control. With Exforge, hypertension administration has never been better.
Exforge: The Ultimate Combination for Hypertension Treatment
Exforge is a medication that combines two potent drugs, amlodipine and valsartan, to successfully handle hypertension. Amlodipine belongs to the calcium channel blockers class, whereas valsartan is a specific blocker of AT1 receptors of angiotensin II. Together, they provide a combined action that helps decrease blood strain and defend in opposition to potential cardiovascular problems.
But what makes Exforge stand out within the vast market of antihypertensive drugs? To understand that, let us take a more in-depth look at the 2 components of Exforge and the way they work together to regulate blood strain.
If the arrest is suspected to be of primary cardiac etiology hypertension classification order 80mg exforge with amex, a compression ratio of 15 compressions to 2 breaths or 30 compressions to 2 breaths may be more effective. A catheter can be quickly inserted into the umbilical vein for intravenous access. After blood is aspirated, insertion of the catheter is stopped, and the epinephrine is given rapidly, followed by a saline flush. Because lung absorption of epinephrine varies, the intravenous route using the umbilical vein is preferred. More personnel will be needed to place the catheter and draw up the medications and saline flushes. If the heart rate does not respond, the dose of epinephrine can be repeated every 3 to 5 minutes. If the infant appears pale, has delayed capillary refill, or decreased pulses, shock may be present. Infant blood loss might have occurred during delivery from placental problems or other sources. Volume expansion should be used cautiously because there is evidence from animal studies for poorer outcomes when it is used in the absence of hypovolemia. Rapid infusion of large volumes has been associated with intraventricular hemorrhage in premature infants. The hands encircle the torso, and the thumbs are placed on top of the lower sternum above the xyphoid process and below a line drawn between the nipples (white line). The index and middle finger are used to apply pressure on the lower third of the sternum above the xyphoid process and below a line drawn between the nipples (white line). The purpose of chest compressions is to squeeze the heart between the sternum and the spine, forcing blood in and out of the heart and to the body. The direction of the compressions should be perpendicular to the chest surface, and the fingers should not be lifted off of the chest after the correct placement is obtained. Incorrect methods during chest compressions can cause rib fracture and liver laceration. Resuscitation of the Newborn bicarbonate benefits the neonate, and its use during resuscitation in the delivery room is not recommended. These infants are at risk for several complications, such as infection, metabolic abnormalities, and seizures. Special Considerations Some newborns do not respond to resuscitation because of specific problems. Infants with upper airway obstruction from micrognathia can be helped by a nasopharyngeal airway and placement of the infant in the prone position. Absence of breath sounds on one side of the chest can indicate a pneumothorax, requiring needle aspiration of the chest. An infant with a scaphoid abdomen and decreased breath sounds may have a diaphragmatic hernia. If the mother has received narcotics shortly before the delivery, the narcotic may be the cause of respiratory depression in the infant. Naloxone is no longer recommended as part of initial resuscitative efforts in the delivery room. The blood vessels in their brains are fragile and can easily bleed during periods of blood pressure variation. The lower birth weights of premature newborns also require smaller sizes of equipment for resuscitation such as facemasks, suction catheters, endotracheal tubes, and umbilical catheters. Oxygen concentrations less than 100% are often used to protect the premature infant from oxygen toxicity. Many personnel trained in newborn resuscitation should be present at the delivery of a high-risk premature infant. Meconium Staining of the Amniotic Fluid Meconium is formed in the newborn gastrointestinal system during gestation. Aspiration of meconium-stained amniotic fluid into the lungs can result in severe pneumonitis and lung injury. The approach to resuscitation for an infant with meconium-stained fluid depends on the condition of the infant immediately after birth. Endotracheal Intubation During neonatal resuscitation, endotracheal intubation may be indicated in the following circumstances: initial endotracheal suctioning of a nonvigorous meconium-stained infant, cases in which bag and mask ventilation is ineffective or prolonged, if chest compressions are performed, and in special situations such as congenital diaphragmatic hernia or extremely low birth weight infants. Intubation of the newborn requires preparation that can be performed while the infant is being ventilated by bag and mask. Complications of intubation include worsening of hypoxia and bradycardia, pneumothorax, contusions, perforation of the trachea or esophagus, and infection. A soft inflatable mask that is attached to a flexible airway tube is placed in the hypopharynx such that the air in the tube is directed into the larynx and away from the esophagus. However, this type of airway cannot be used to suction meconium from the trachea nor to give endotracheal drugs. Crying and Vigorous Infant If the newborn with meconium-stained amniotic fluid has normal respiratory effort and muscle tone with a heart rate higher than 100 beats/min, gentle mouth and nose suctioning can be performed using a bulb syringe or suction catheter. A laryngoscope is inserted, and a 12- or 14-F catheter is used to suction the mouth and posterior pharynx. This maneuver may be repeated until the suctioned fluid is clear unless the infant requires resuscitation. Very low birth weight (less than 1500 g) infants will need additional warming techniques such as prewarming the delivery room, covering the baby in plastic wrapping, and placing the baby under a radiant warmer and/or an exothermic mattress; however, iatrogenic hyperthermia should be avoided. Outcome after successful resuscitation of babies born with Apgar scores of 0 at both 1 and 5 minutes.
World Health Organization Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception blood pressure chart age 13 discount exforge 80mg with amex. The clinical standard for diagnosis of endometriosis is laparoscopic confirmation. Primary dysmenorrhea occurs without underlying pathology, typically beginning soon after menarche. It is common in adolescent girls, with prevalence ranging from 20% to 90% depending on measurement methods; about 15% of adolescents describe their dysmenorrhea as severe. During adolescence, dysmenorrhea leads to high rates of school absence and activity nonparticipation. According to representative national survey data in the United States, 14% of adolescent girls aged 12 to 17 years frequently miss school because of menstrual cramps. A prospective cohort study showed that the prevalence and severity of dysmenorrhea was lower at 24 years of age than at 19 years of age. At 24 years of age, 67% of the women still experienced dysmenorrhea, and 10% reported pain severity that limited daily activity. The prevalence and severity of dysmenorrhea were reduced in women who were parous at 24 years and nulliparous at 19 years, but they were unchanged in women who were still nulliparous or women who had had a miscarriage or abortion. There is a significant correlation between the severity of dysmenorrhea and the amount of menstrual flow. Survey data demonstrate that depression and anxiety are associated with menstrual pain and suggest that loss of social support is a significant contributor to menstrual symptoms. The severity of dysmenorrhea is not associated with height, weight, or regularity of the menstrual cycle. Physical activity has been studied and found not to be associated with any pain parameter. Secondary dysmenorrhea typically starts later in life after the onset of an underlying causative condition, most often endometriosis. The association between dysmenorrhea and endometriosis is uncertain for women with minimal disease. However, based on a study of more than 1000 women with laparoscopically confirmed endometriosis, chronic pelvic pain, dyspareunia, and dysmenorrhea are in fact related to the extent of endometriosis. Sexually active adolescents and young women should be screened for chlamydia and gonorrhea, which can be done with either urine or a genital sampling. For adolescents and women who do not have a history consistent with primary dysmenorrhea or who are refractory to treatment, endometriosis may be suspected. However, the available evidence had little power to detect such differences, because most individual comparisons were based on few small trials. In one study in which diclofenac (Voltaren) 100 mg was compared with placebo for treatment of primary dysmenorrhea, the authors found that leg strength and aerobic capacity were maintained at the level found during luteal phase when women took diclofenac for dysmenorrhea, but they were reduced during menses in the placebo group. In a trial comparing far-infrared emitting belt versus placebo belt for treatment of primary dysmenorrhea, both with concurrent application of topical heat, both groups improved, and the duration of the analgesic effect was significantly longer in the group treated with the infrared belt. They include Psidii guajava extract7 6 mg/day, French maritime pine bark extract (pycnogenol),7 and ginger root powder7 250 mg 4 times daily. Celecoxib (Celebrex) 200 mg was compared with naproxen sodium (Naprosyn) 550 mg and placebo for treatment of dysmenorrhea and found to be superior to placebo but not as effective as naproxen. Etoricoxib (Arcoxia)5 120 mg daily was found to be better than placebo and equivalent to mefenamic acid (Ponstel) for treatment of primary dysmenorrhea with less nausea and epigastric pain than mefenamic acid. Lumiracoxib (Prexige)5 200 mg daily was compared with naproxen 500 mg twice daily and placebo for treatment of primary dysmenorrhea and found to reduce pain more than placebo and similar to naproxen. Acupressure and Acupuncture the evidence for the effectiveness of acupuncture is not conclusive. In unblinded studies women experience clinically relevant reduction in pain scores, a mean of more than 10 points on a 100-point scale, which could be due to placebo effect. Several other studies suggest that acupressure at the Sanyinjiao point or Taichong point is more effective than no intervention or inadequately blinded control groups. Because acupressure is a low-cost and harmless intervention, it may be worth considering even if the pain reduction is a placebo response. In a study of women with laparoscopically proven endometriosis, low-dose ethinyl estradiol and norethisterone (norethindrone) decreased dysmenorrhea associated with endometriosis as compared with placebo (with pain assessment on a verbal rating scale from 0 to 3). Depot medroxyprogesterone acetate1 (Depo-Provera) is similarly effective, but it is less likely to be well tolerated owing to unpredictable bleeding, weight gain, and mood changes. In one uncontrolled study, nifedipine1 (Procardia) 20 to 40 mg given orally reduced myometrial activity and relieved dysmenorrhea. This drug could be considered as an adjunct in severe cases of primary dysmenorrhea after ruling out endometriosis. Participants randomized to the intervention group were told to do the yoga poses during luteal phase and complete a questionnaire regarding menstrual characteristics. There was significant reduction in intensity and duration of pain in the yoga group compared with baseline and with the control group. Nifedipine Spinal Manipulation Overall there is no evidence to suggest that spinal manipulation is effective in the treatment of primary and secondary dysmenorrhea. Both groups improved significantly from baseline without significant difference between them. There were no differences between groups for relief of dysmenorrhea at 3-, 6-, and 12-month follow-up, but more surgical complications were experienced with neurectomy. Danazol is a 19-nortestosterone derivative with a long history of use for treatment of endometriosis pain at a dosage of 400 to 800 mg daily for 6 months, but it is often poorly tolerated owing to androgenic side effects.
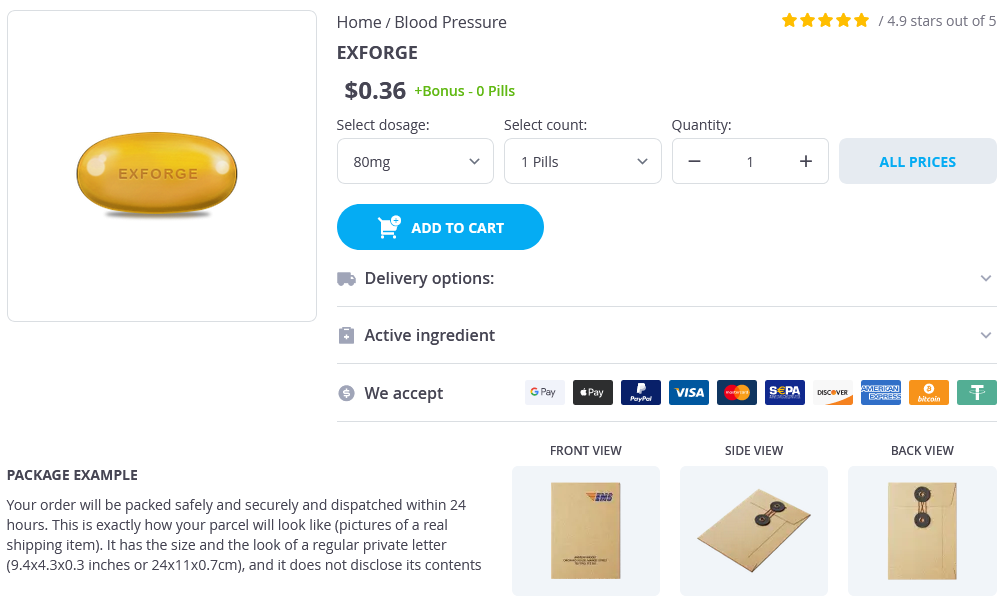
Exforge Dosage and Price
Exforge 80mg
- 1 pills - $0.40
Some improvement should be noted within 3 or 4 weeks heart attack high the honeymoon is over buy exforge us, and the dose should be increased if no improvement is seen. The differential diagnosis can include several organic causes, such as endocrine dysfunction, intoxication or withdrawal, hypoxia, metabolic abnormalities, and neurologic disorders. Severe depression, bipolar disorder, prodromal schizophrenia, delusional disorder, and adjustment disorder can often be accompanied by severe anxiety. Many organic causes can be ruled out by a thorough history and basic laboratory work, including thyroid-stimulating hormone, urine toxicology, electrocardiogram, complete blood count, and metabolic panel. The most common medical conditions associated with anxiety are presented in Box 1. Drugs commonly associated with anxiety include stimulants such as amphetamine, cocaine, methamphetamine, and caffeine. These conditions can be disabling and costly to the patient and to the health care system. Despite the prevalence of anxiety disorders, patients often remain undiagnosed and untreated, and patients with unrecognized anxiety disorders tend to be high users of general medical care. Patients with anxiety disorders can present with multiple somatic complaints and comorbid disorders, causing great effort and expense in identifying the cause of unexplained symptoms. Once anxiety disorders are identified, patients may be treated using well-tested and efficacious pharmacologic and psychotherapeutic treatments. Because of the risk for rebound anxiety when withdrawing from benzodiazepines with short half-lives, such as alprazolam (Xanax), many prefer the longer-acting benzodiazepines, such as clonazepam (Klonopin). Comorbid psychiatric disorders significantly lower the likelihood of recovery from anxiety and increase recurrence rates. A referral to a psychiatrist for further evaluation and management may be necessary if none of these strategies works. Treatmentrefractory anxiety can be extremely frustrating for both the patient and clinician. This can lead to increased dependence on benzodiazepines and an escalation of doses required for the same effect. When approaching the start of therapy, the clinician should reassure the patient that effective treatment is available, but that patience may be necessary until the right combination of modalities is found. Although all of the anxiety disorders display a significant amount of chronicity, most patients have an improved outcome with appropriate treatment. Patients with an earlier onset of symptoms (childhood or adolescence) can generally expect a more chronic course and may be more difficult to treat. However, time to resolution of symptoms is shortened and overall functioning can improve with treatment. Pharmacotherapy often helps to prevent relapse, and rates are improved when effective treatment is continued for 12 months. When considering termination of pharmacologic treatment, the risk for relapse in all of the disorders should be discussed with the patient. If relapse occurs, reinstituting treatment is indicated, and many patients opt for indefinite treatment to maintain remission of symptoms. Lifelong management with pharmacotherapy or psychotherapy, or both, is not unusual for many patients. Guideline watch: Practice guidelines for the treatment of patients with panic disorder. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Important diagnostic features of delirium include development of the disturbance over a short period of time; its fluctuating nature; and the noticeable change from baseline attention, awareness, and cognition. Dysregulation of neuronal activity is accompanied by sleep-cycle disturbance, conceptual disorganization, lability of affect, thought process abnormalities, and evidence of systemic disturbance in physical condition. Epidemiology Delirium is one of the most common conditions in the hospital, with prevalence rates ranging from 15% to 20% on medical floors to 60% in surgical patients and 80% in the intensive care units. Monitoring Early identification, appropriate management, and system-wide efforts at prevention can improve treatment outcome and quality of patient care. Systematic implementation and routine use of validated delirium screening tools have a significant impact on healthcare delivery, quality measures, and patient satisfaction. Improved care of patients with delirium could be achieved through the implementation of effective screening tools, incorporation of delirium assessments into nursing and physician documentation, and improved communication between team members. Risk Factors Several predisposing, precipitating, and perpetuating factors for delirium have been well described. Medication exposure and polypharmacy have been associated with strong predication of delirium. Many theories have been postulated regarding the development of delirium without a single compelling explanation of this complex neurobehavioral syndrome. Knowledge of contributing factors and pathophysiologic mechanisms can assist clinicians in addressing, correcting, and possibly preventing delirium. The disturbance develops over a short period of time (usually hours to a few days), represents a change from baseline attention and awareness, and tends to fluctuate in severity during the course of the day C. The disturbance in criteria A and C are not better explained by another preexisting, established, or evolving neurocognitive disorder and do not occur in the context of a severely reduced level of arousal, such as coma E. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or withdrawal. The patient may be hyperactive (agitated) or hypoactive (lethargic) or may demonstrate a mixed pattern. The patient demonstrates a reduced ability to direct, focus, and shift his or her attention, and a reduced orientation to their environment.