Fincar
General Information about Fincar
In latest years, Fincar has gained recognition as a therapy for male sample hair loss. Developed by Merck & Co., Fincar has been approved by the U.S. Food and Drug Administration (FDA) since 1997 to be used in men solely. It is on the market in tablet form and is taken orally once a day. The active ingredient in Fincar is finasteride, which works by inhibiting the manufacturing of the male hormone, androgen. Androgens, also identified as male hormones, play a task in hair loss, and Fincar works by decreasing the levels of dihydrotestosterone (DHT), a potent type of androgen responsible for hair loss in males.
Fincar is a secure and well-tolerated medicine, and if taken as directed, the unwanted effects are generally mild and uncommon. However, like all medicines, Fincar could cause sure side effects in some males. The mostly reported unwanted effects of Fincar include a lower in libido, erectile dysfunction, and a decrease in ejaculate quantity. These unwanted side effects are often mild, and so they disappear once the medicine is discontinued. In uncommon cases, some men may expertise breast enlargement or breast tenderness, however these side effects often resolve on their own with out intervention.
It is value noting that Fincar isn't a treatment for hair loss, and it should be taken repeatedly to maintain its effects. If therapy is stopped, any hair regrowth will be misplaced within 12 months, and hair loss will proceed as it might have, had the remedy never been began. Therefore, Fincar must be used as a long-term remedy for male pattern hair loss.
One main concern about Fincar, and any treatment that affects hormones, is its potential influence on fertility. Some studies have shown that Fincar can lower sperm count and motility, but this effect is reversible as soon as the medicine is discontinued. Nonetheless, males who are trying to conceive should consult with their physician earlier than beginning Fincar or any other medicine that impacts hormones.
Fincar, also known as finasteride, is a nicely known medication used for treating male sample hair loss. While hair loss is frequent and might affect individuals of all ages, it is more prevalent in men. Male sample hair loss, also referred to as androgenetic alopecia, is a genetic condition that could be hereditary and can happen at any age after puberty. It is estimated that by the age of fifty, over 50% of men will experience some degree of hair loss.
Fincar has been scientifically confirmed to assist prevent further hair loss and promote hair re-growth in males affected by male sample hair loss. In a five-year scientific study, 9 out of 10 men who took Fincar every day experienced an increase in hair development and a slowdown in hair loss. Furthermore, 48% of the men who participated within the examine showed visible hair regrowth after one 12 months of utilizing Fincar.
In conclusion, Fincar is a widely used and efficient treatment for male sample hair loss. It works by decreasing the degrees of the androgen hormone, which is answerable for hair loss in men. While unwanted effects are rare and usually mild, Fincar must be taken as directed to take care of its beneficial results. Men who're experiencing hair loss ought to speak to their doctor about Fincar as a possible remedy choice. With its confirmed efficacy and safety record, Fincar can help men regain their self-confidence and improve their general well-being.
The laparoscopic adjustable gastric band (Lap-Band): a prospective study of medium-term effects on weight prostate cancer cure purchase discount fincar, health and quality of life. Studies of the Swedish adjustable gastric band and Lap-Band: a systematic review and meta-analysis. Busetto L, Valente P, Pisent C, Segato G, de Marchi F, Favretti F, Lise M, Enzi G. The effect of laparoscopic adjustable gastric bands on esophageal motility and the gastroesophageal junction: analysis using high-resolution video manometry. Hunger control and regular physical activity facilitate weight loss after laparoscopic adjustable gastric banding. Laproscopic adjustable gastric banding for patients with body mass index of < or = 35 kg/m2. Changes in satiety, supra- and infraband transit, and gastric emptying following laparoscopic adjustable gastric banding: a prospective follow-up study. Favretti F, Segato G, Ashton D, Busetto L, De Luca M, Mazza M, Ceoloni A, Banzato O, Calo E, Enzi G. Laparoscopic adjustable gastric banding in 1791 consecutive obese patients: 12-year results. Treatmentof mild to moderate obesity with laparoscopic adjustable gastric bandingor an intensive medical program: a randomized trial. Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise: the 6-year Malmo feasibility study. Health outcomes of severely obese type 2 diabetic subjects 1 year after laparoscopic adjustable gastric banding. Effect of Lap-Band-induced weight loss on type 2 diabetes mellitus and hypertension. Symmetrical pouch dilatation after laparoscopic adjustable gastric banding: incidence and management. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Bariatric emergencies for non-bariatric surgeons: complications of laparoscopic gastric banding. Complications after laparoscopic adjustable gastric banding for morbid obesity: experience with 1000 patients over 7 years. Chapter 10 Perioperative Care of the Surgical Patient Patchaya Boonchaya-Anant, Amanda G. Apovian Introduction the prevalence of obesity has been increasing in adults over the past 30 years. Obesity is a risk factor for metabolic complications such as insulin resistance, type 2 diabetes, nonalcoholic fatty liver disease, dyslipidemia and hypertension and can lead to morbidities including atherosclerosis and cardiovascular disease. Treatment of obesity includes behavioral modification, pharmacotherapy, and bariatric surgery. Bariatric surgery is the most effective treatment for obesity and can reduce mortality and obesityrelated comorbid conditions in severely obese patients [2, 3]. There has been an increase in the number of bariatric surgeries performed since the introduction of minimally invasive surgery with an estimated 113,000 cases performed currently per year [4]. Boonchaya-Anant King Chulalongkorn Memorial Hospital, Division of Endocrinology and Metabolism, Department of Medicine, Chulalongkorn University, Thai Red Cross Society, 1873 Rama 4 Rd, Pathum Wan, Bangkok 10330, Thailand e-mail: b patchaya@yahoo. Relative contraindications to surgery may include severe heart failure, unstable coronary artery disease, end-stage lung disease, active cancer diagnosis/ treatment, cirrhosis with portal hypertension, uncontrolled drug or alcohol dependency, and severely impaired intellectual capacity [6]. Practitioners must decide if a patient demonstrates adequate understanding of the procedure and motivation to comply with follow-up care. This includes an understanding of the complications of bariatric surgery, and the need for postoperative medical and nutritional visits. It is crucial to engage the entire team caring for the patient when making the final decision so as to ensure the safest and most optimal outcome for the patient. Preoperative Evaluation A multidisciplinary team, including a medical practitioner, nutritionist, mental health professional, and surgeon, should be involved in the evaluation of patients undergoing bariatric surgery. The goal of the evaluation is to ensure proper candidate selection, reduce surgical risks, and optimize postoperative outcomes. History and Physical Examination; Comorbidities, Weight Loss History Patient evaluation prior to bariatric surgery should be comprehensive, and include the obesity-related comorbidities, possible treatable underlying causes of obesity, weight loss history, psychosocial history, and physical exam. The detailed weight history includes patterns of weight gain and loss, as well as prior weight loss attempts with dietary and medical therapies. Most patients who present for the evaluation of bariatric surgery have a history of extensive dieting. Commitment to medical follow-up is an important component in eligibility for bariatric surgery, as it is critical to monitor for nutritional deficiencies and ensure optimal long-term weight loss [7, 8]. Hypothyroidism is more common in obesity than normal weight individuals and can cause weight gain but it is usually not the sole cause of obesity. Some clinical signs such as purplish striae, proximal muscle weakness, and osteopenia may be a clue for further work up. Screening for Obesity-Related Comorbidities the goal of this evaluation is reduce operative risk and optimize postsurgical outcomes. Cardiovascular risks should be assessed based on individual coronary risk factors, physical exercise capacity, and symptoms of unstable cardiac disease. Patients with existing heart disease may require extensive evaluation by cardiologists. Preoperative stress tests should be considered on patients with known heart disease, those older than 55, patients who have had diabetes for more than 10 years, and those with atypical chest pain.
Less-stringent targets for hemoglobin A1c may be considered in patients with advanced microvascular and macrovascular complications prostate 049 buy generic fincar 5 mg on line, long duration of diabetes, and those who are at risk of hypoglycemia [62]. Poor preoperative glycemic control is associated with postoperative hyperglycemia and less weight loss [63], and postoperative hyperglycemia is an independent risk factor for surgical site infection [64, 65]. With improvement in surgical techniques and surgical experience, the 30-day inpatient mortality rate has declined to about 0. The major complication rates following bariatric surgery are approximately 510 % and most common are venous thromboembolism and respiratory complications [68]. Patients who are at high risk for postoperative myocardial infarction should be monitored in an intensive care setting. Pulmonary embolism is by far the most common cause of mortality after bariatric surgery. Most physicians employ intermittent compression stockings or subcutaneous unfractionated heparin or low molecular weight heparin as mentioned in the previous section. Pulmonary complications can be prevented by use of incentive spirometry, early ambulation, and adequate pain control [75]. Leaks are the second most common cause of death following bariatric surgery, and account for 38 % of deaths after laparoscopic gastric bypass, and 12. Anastomotic leaks can lead to sepsis, organ failure, and death, and may be difficult to diagnose. The presence of tachycardia of > 120 beats/ min, tachypnea, fever, or abdominal pain should prompt an evaluation [78, 79]. Less severe cases can be managed with antibiotics and drainage; however, reoperation is necessary in some cases [80]. Rhabdomyolysis is a potential complication of surgical procedures in morbidly obese patients. They are more common after open procedures than those done laparoscopically (an incidence of 7 % vs. Hyperglycemia is one of the risk factors for surgical site infection [86] and attempt should be made to control postoperative hyperglycemia. Usually, a protocol-derived nutritional program can be started within 24 h after surgery but the diet progression should be discussed with the surgeon and guided by the dietitian. Patients will advance through stages 1 and 2 to stage 3 while in the hospital and will continue on stage 3 at home before being advanced to stages 4 and 5 after post op evaluation by their physician. The diet is advanced from only liquids to high-protein soft solids and then eventually to low-fat high-protein solid foods over the course of 2 months. Minimum protein intake of 6090 g per day should be achieved to avoid loss of lean body mass [87, 88]. Protein intake is usually inadequate in the first 2 months after surgery; therefore, protein supplements such as protein powder are often advised to achieve optimal protein intake. There are some general principles to help patients adjust to digestion with their new anatomy. Patients should chew food very thoroughly to facilitate swallowing 10 Perioperative Care of the Surgical Patient 163 Table 10. During the progression through early food stages, patients should not drink liquids at the same time as they are eating their regular small meals. It is common for patients to have difficulty tolerating several types of food during the first several months after surgery, most commonly dry meats, breads, pasta, milk, and nuts. Patients should keep a food log to help identify food intolerances and monitor compliance. Protein should be consumed at the onset of the meal and carbohydrate should come from nutrient-dense complex carbohydrates to avoid Dumping syndrome [89]. Dumping syndrome can occur after the Roux-en-Y gastric bypass due to the loss of the physiologic sphincter at the stomach outlet. If the patient consumes a bolus of high sugar or high fat food, its arrival into the small intestine will cause a release of gut hormones and an influx of intraluminal fluid. Routine vitamin supplementation will vary from patient to patient, with the most important determinant being the type of surgery performed. Though the laparoscopic adjustable gastric banding does not generally cause vitamin or mineral malabsorption, the variety and amount of food intake are restricted. It is recommended to take a multivitamin to meet daily requirements for both vitamins and minerals. Those undergoing Roux-en-Y gastric bypass, biliopancreatic diversion or biliopancreatic with duodenal switch are at greater risk for nutritional deficiencies [90]. All patients should be encouraged to consume 12 multivitamins per day after surgery depending on the type of procedure performed. Most clinicians recommend routine supplementation with 12001500 mg of calcium per day. Most calcium tablets also contain vitamin D but this may not provide adequate supplementation. It is estimated that 3050 % of patients might develop B12 deficiency after gastric bypass if not supplemented beyond a multivitamin [91, 92]. Treatment with oral crystalline B12 at doses of at least 350 mcg per day has been shown to maintain normal plasma B12 levels [93]. Subcutaneous or intramuscular injections may be used in patients not responding to oral therapy. A multivitamin containing folate will generally provide sufficient folic acid after surgery [94]. Iron deficiency after gastric bypass is quite common especially in premenopausal women.
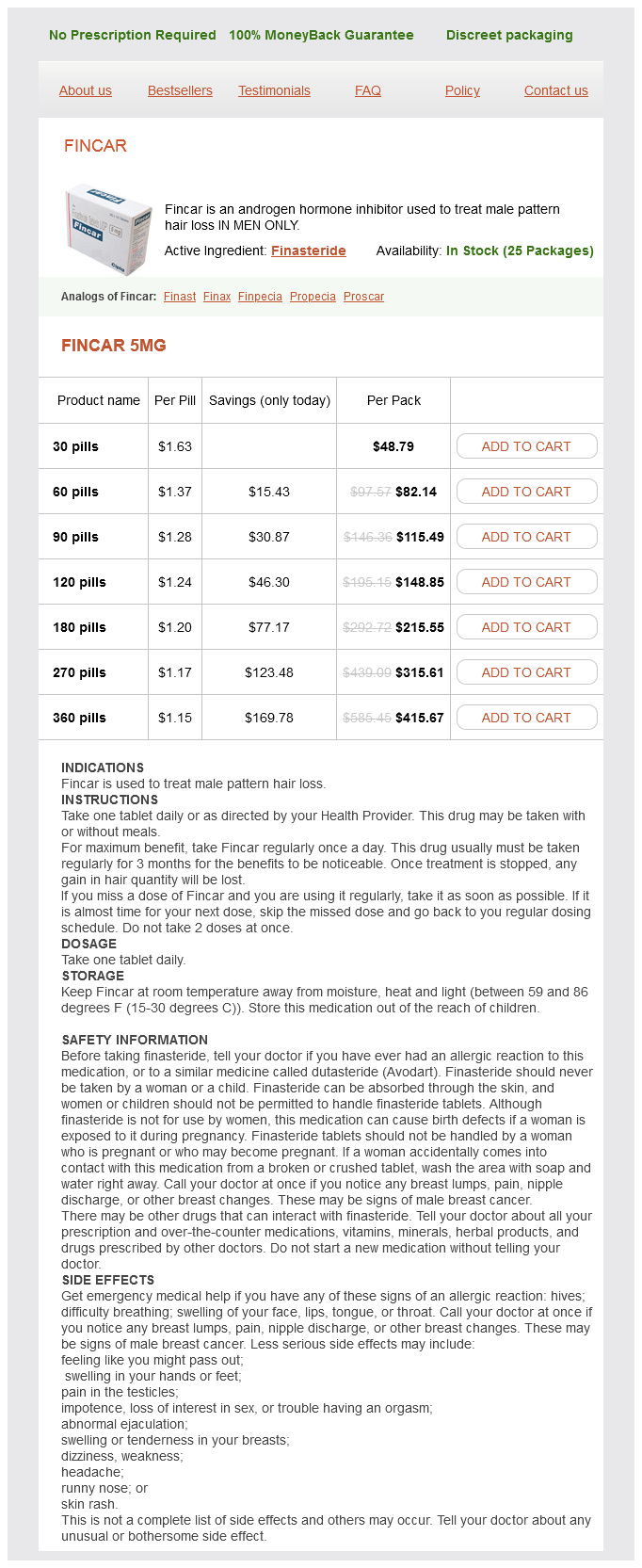
Fincar Dosage and Price
Fincar 5mg
- 30 pills - $48.79
- 60 pills - $82.14
- 90 pills - $115.49
- 120 pills - $148.85
- 180 pills - $215.55
- 270 pills - $315.61
- 360 pills - $415.67
Incidence of deep vein thrombosis in morbidly obese patients undergoing laparoscopic Roux-en-Y gastric bypass prostate cancer 1cd 10 fincar 5 mg purchase amex. Noninvasive ventilation immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparoscopic bariatric surgery. Surgical vs conventional therapy for weight loss treatment of obstructive sleep apnea: a randomized controlled trial. Major respiratory adverse events after laparascopic gastric banding surgery for morbid obesity. Incidence of gastroenterostomy stenosis in laparoscopic Roux-en-Y gastric bypass using 21- or 25-mm circular stapler: a randomized prospective blinded study. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. A multicenter, placebo-controlled, randomized, double-blind, prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Bowel obstruction after open and laparoscopic gastric bypass surgery for morbid obesity. Intussusception after Roux-en-Y gastric bypass for morbid obesity: case report and literature review of rare complication. Comparison of cholecystectomy cases after Roux-en-Y gastric bypass, sleeve gastrectomy, and gastric banding. Wernicke-korsakoff encephalopathy and polyneuropathy after gastroplasty for morbid obesity: report of a case. Prevalence of psychiatric disorders before and 1 year after bariatric surgery: the role of shame in maintenance of psychiatric disorders in patients undergoing bariatric surgery. Prevalence and predictors of self-reported sexual abuse in severely obese patients in a population-based bariatric program. Thirty-day mortality after bariatric surgery: independently adjudicated causes of death in the longitudinal assessment of bariatric surgery. Some Demographic and Socio-cultural Aspects of Synesthesia Sean Day o me, the taste of beef is dark blue. And when tenor saxophones play the music looks like a floating, suspended coiling snake-ball of lit-up purple neon tubes. Over the years that I have been investigating synesthesia, I have heard others frequently refer to what benefits the study of synesthesia might throw upon other, serious and life-threatening disorders. Synesthesia appears to have some aspects in common with-and thus helps us to understand-such conditions as phantom limbs (see. Correspondences I have received over the past 10 years also indicate that synesthesia may have some possible connections or associations with some forms of autism (Temple Grandin, for example, asserted this in personal communication to me on December 9,1998), some types of epilepsy (see Cytowic, 2002), and migraines (see. However, I feel that one major reason for studying synesthesia frequently and persistently seems to be overlooked: There are a lot of synesthetes out there in the world who live with synesthesia-and with being a synesthete-all of their lives. The fact that a large number of individuals join sensations in a different way should not distract from its value as an area of scientific investigation. Overview and Prevalence of Synesthesia Synesthesia is the general name for two related sets (or "complexes") of cognitive states (see Baron-Cohen & Harrison, 1997; Cytowic, 1993, 2002; Day, 2001, 2003; Grossenbacher & Lovelace, 2001; Ramachandran & Hubbard. In the first set, "synesthesia proper," stimuli to one sense, such as smell, are involuntarily and simultaneously perceived as if by one or more other, additional senses, such as sight and/or hearing. For example, I have three types from this set of synesthesia: the sounds of musical instruments will make me see certain colors, each color specific and consistent with the particular instrument playing. I also have colored taste and smell sensations; for example, the taste of espresso coffee can make me see a pool of dark green, oily fluid about four feet away from me. The most common forms of cognitive synesthesia involve such things as colored written letter characters (graphemes), numbers, time units, and musical notes or keys. For example, the synesthete might see, about a foot or two before her (the majority of synesthetes, approximately 72%, are female), different colors for different spoken vowel and consonant sounds, or perceive numbers and letters, whether conceptualized or before her in print, as colored. A friend of mine always perceives the letter "a" as pink, "b" as blue, and "c" as green, no matter what color of ink they are printed with. Synesthesia apparently has neurological aspects in regard to its causation, and it seems to be heritable, with one component (possibly a "trigger factor") perhaps passed down genetically as autosomal dominant. However, Bailey and Johnson (1997) propose X-linked dominance, with male lethality (see also Cytowic 2002, pp. The percentage of the general human population which has synesthesia varies with the type involved; estimates run from 1 in 500 for basic types of cognitive synesthesia (colored graphemes or musical pitches), to 1 in 3,000 for more common forms of synesthesia proper (colored musical sounds or colored taste sensations), to 1 in 25,000 or more (1 in a couple million However, there are a few trends among synesthetes; discovering such trends has been the focus of one of my major lines of research over the past 11 years. In 1991,1 created an international e-mail forum for synesthetes, researchers of synesthesia, and all interested other parties, called the Synesthesia List (I have since come to regret the choice of name, but it has been around too long now to easily change). Over the past 10 years, I have studied cases of colored grapheme synesthesia in attempt to discern whether there are any trends. Approximately 2 7% of my current data comes from publications tracing all the way back to accounts such as that of Sachs (1812) and up to recent reports such as those mentioned by Cytowic (2002); the other 73% stems from my use of the Synesthesia List, personal letters and phone calls, and face-to-face interviews. Ready worldwide availability of the crayons, their ease in transport and use, and the fact that most subjects were very familiar with them, often proved extremely useful in facilitating matters. For those cases I gathered myself, I asked the synesthete to try to classify things within the 11 categories, usually suggesting (and often using, in face-to-face interviews) Crayola Crayons as a guide. When a different color designation was used, it was usually fairly easy to place it as a subtype of one of the 11 given: for example, "tangerine" is a type of orange; "mint green" a type of green; and "cherry" a type of red. I used my own judgment on this, but based my judgment heavily on what category the synesthetes I worked with felt was most proper. Some synesthetes mentioned more than one color for a particular letter; if two colors were mentioned, I scored each as 1/2 (0. With 11 colors, if things were evenly distributed, that means that any particular letter (A, for example) would have one of these colors (red, for example) about 9.