Flutamide
General Information about Flutamide
Flutamide, offered under the brand name Eulexin, is a drugs commonly used in the treatment of prostate most cancers. This most cancers, which affects the prostate gland in men, is likely one of the commonest types of cancer and could be life-threatening if not handled early. Flutamide is classed as an antiandrogen, which means it blocks the results of male hormones, particularly testosterone, within the body. By doing so, it helps to sluggish the expansion and spread of prostate most cancers cells.
Prostate cancer is a type of most cancers that develops within the prostate gland, a small walnut-sized gland situated just under the bladder in men. The risk of creating prostate most cancers will increase with age and is more frequent in males over the age of 50. Symptoms of prostate cancer might embody problem urinating, blood within the urine, and ache in the pelvic space. However, some males may not expertise any symptoms in any respect within the early phases of the disease.
As with any treatment, there are potential unwanted aspect effects associated with Flutamide. The most typical unwanted effects embody sizzling flashes, breast tenderness, diarrhea, and decreased libido. In uncommon circumstances, it may also trigger liver problems, similar to jaundice, which is why regular monitoring of liver function is recommended during remedy.
Flutamide works by blocking the action of androgens, similar to testosterone, which are the male hormones responsible for the event and growth of prostate cancer cells. It does this by binding to androgen receptors, preventing them from receiving messages to develop and divide. This helps to slow the progression of the most cancers and can also shrink the scale of the tumor.
Eulexin is typically taken together with different drugs, similar to a gonadotropin-releasing hormone (GnRH) agonist, to attain the best therapy for prostate most cancers. GnRH agonists work by lowering testosterone ranges in the body, and Flutamide helps to block any remaining testosterone. This combination therapy is called total androgen blockade and has been proven to be more practical in treating prostate cancer than utilizing both medicine alone.
Aside from treating prostate most cancers, Flutamide can also be used in transgender hormone therapy to block the effects of testosterone in male-to-female transitions. It may also be used to deal with hirsutism, a condition the place girls expertise excessive hair growth because of elevated ranges of male hormones in the body.
In conclusion, Flutamide, or Eulexin, is a commonly used medication within the treatment of prostate most cancers. As an antiandrogen, it helps to sluggish the expansion and unfold of prostate most cancers cells by blocking the consequences of male hormones in the body. While there are potential unwanted effects, it has been proven to be an efficient treatment choice when utilized in mixture with different medications. If you or a loved one has been identified with prostate cancer, speak to your doctor about whether Flutamide could additionally be a suitable treatment choice.
Flutamide is taken orally in the form of a pill and is typically prescribed for a period of a number of months. The dosage and duration of remedy will range depending on the person and the severity of their situation. It is necessary to comply with the prescribed dosage and proceed taking the medication as directed, even if symptoms improve.
Comparison of concentrations and viscosities in the proximal tubules and renal pelvis after intravenous injections of contrast media medicine rocks state park cheap flutamide online. Induction, prevention and mechanisms of contrast media-induced acute renal failure. Sodium bicarbonate plus isotonic saline versus saline for prevention of contrast-induced nephropathy in patients undergoing coronary angiography: A randomized controlled trial. Effect of short-term rosuvastatin treatment on estimated glomerular filtration rate. Does prophylactic treatment with felodipine, a calcium antagonist, prevent low-osmolar contrast-induced renal dysfunction in hydrated diabetic and nondiabetic patients with normal or moderately reduced renal function Prophylactic hemodialysis after radiocontrast media in patients with renal insufficiency is potentially harmful. Chronic kidney injury in patients after cardiac catheterisation or percutaneous coronary intervention: A comparison of radial and femoral approaches. Elimination of iohexol, a low osmolar nonionic contrast medium, by hemodialysis in patients with chronic renal failure. Radiographic contrast media induced nephropathy: Experimental observations and the protective effect of calcium channel blockers. Contrast media-induced nephrotoxicity: identification of patients at risk and algorithms for prevention. A randomized controlled trial of intravenous N-acetylcysteine for the prevention of contrast-induced nephropathy after cardiac catheterization: Lack of effect. The Pathogenesis, Outcomes, and Prevention of Contrast-Associated Acute Kidney Injury 303 Weinrauch, L. Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. Relationship of renal hemodynamic and functional changes following intravascular contrast to the renin-angiotensin system and renal prostacyclin in the dog. N-Acetylcysteine and contrast-induced nephropathy: A meta-analysis of 13 randomized trials. High-dose statin pretreatment for the prevention of contrast-induced nephropathy: A meta-analysis. Efficacy of statin pretreatment for the prevention of contrast-induced nephropathy: A meta-analysis of randomised controlled trials. Statins for the prevention of contrast-induced nephropathy: A systematic review and meta-analysis. Short-term, high-dose statins in the prevention of contrast-induced nephropathy: A systematic review and meta-analysis. Systematic review: Sodium bicarbonate treatment regimens for the prevention of contrast-induced nephropathy. These concerns were based on histopathologic studies of the kidney in lithium-treated psychiatric patients suffering from acute lithium intoxication or severe polyuria. Controlled studies of renal function in patients treated with lithium have enabled us to better understand the spectrum of lithium-induced nephrotoxicity, though not all questions have been answered. Studies evaluating renal function in lithium-treated patients must be interpreted with caution due to differences in experimental design, criteria for patient selection, treatment duration, dose and type of lithium preparations, plasma lithium levels, and concurrent therapy with other psychotropic agents. Many of these studies failed to exclude patients with preexisting renal disease, while others lack suitable control groups. Lithium-induced natriuresis frequently contributes to renal insufficiency, and correction of volume depletion may improve renal function (Hansen, 1981; Hansen and Amdisen, 1978; Thomsen and Olesen, 1978). However, renal functional impairment frequently persists even after volume expansion. Even after recovery from an episode of acute lithium intoxication, renal functional impairment may persist (Hansen, 1981; Hansen and Amdisen, 1978). Rarely, nontraumatic rhabdomyolysis has been described in association with lithium-induced neuroleptic malignant syndrome or lithium-induced hyperosmolar dehydration (Bateman et al. Preventing volume depletion during episodes of acute lithium intoxication is important to reduce the risk of nephrotoxicity. The treatment of acute lithium intoxication may include aggressive fluid resuscitation, enteric lavage to prevent continued gastrointestinal absorption of lithium, administration of sodium polystyrene sulfonate, and appropriate renal replacement therapy (Bailey et al. In acute lithium intoxication, symptoms may be absent despite markedly elevated serum lithium levels due to delayed diffusion of lithium across the bloodbrain barrier. In contrast, symptoms may be severe with chronic lithium intoxication despite only modestly elevated serum lithium levels. The Extracorporeal Treatments in Poisoning Workgroup recommends extracorporeal therapy for lithium poisoning if (1) renal function is impaired and the serum lithium level exceeds 4 mequiv. LÀ 1 regardless of symptoms or (2) in the presence of reduced level of consciousness, seizures, or life-threatening cardiac arrhythmias, irrespective of serum lithium level (Decker et al. LÀ 1, significant confusion exists, or the expected time to reduce lithium levels to < 1. These guidelines conform to previous recommendations that appear in the literature (Eyer et al. Extracorporeal therapy should be continued until clinical improvement or a fall in serum lithium level to <1 mequiv. If serum lithium levels cannot be readily measured, extracorporeal treatment should be continued for at least 6 h.
By contrast medications emt can administer order flutamide 250 mg without prescription, other investigators have demonstrated reduced bone mineral density in lithium-treated patients (Ananth and Dubin, 1983; Christiansen et al. Long-term lithium therapy leads to an increase in parathyroid gland volume (Mallette et al. Lithium has been shown to stimulate cellular proliferation of hyperplastic and adenomatous parathyroid tissue in vitro but had no effect on the growth of normal parathyroid tissue (Saxe et al. Parathyroid adenomas and parathyroid gland hyperplasia have been observed in lithium-treated patients (Ananth and Dubin, 1983; Nordenstrom et al. Although parathyroid adenomas are more common than is parathyroid hyperplasia, the latter is overrepresented among lithium-treated patients as compared to the general population (Bendz et al. While hyperchloremic metabolic acidosis is observed in experimental models of lithium nephrotoxicity, an incomplete form of distal renal tubular acidosis is usually observed in lithium-treated patients. The development of a reversible defect in urinary acidification after initiation of lithium therapy has been demonstrated in longitudinal studies (Carreras et al. Although not a universal finding, most studies also found that lithium-treated patients are able to maximally acidify their urine and excrete normal amounts of ammonia and titratable acid after acid loading (Batlle et al. Studies performed in isolated rabbit cortical collecting duct tubules and the turtle bladder showed that the lithium-induced defect in urinary acidification results from a voltage-dependent acidification defect (Bank et al. Consistent with the reduction in the lumen-negative transepithelial gradient mechanism is the fact that infusion of sodium sulfate corrects the acidification defect (Nascimento et al. The expression of other renal acid transporters has been found to be unchanged or increased (Kim et al. However, upregulation of these other renal acid transporters by lithium may merely reflect a compensatory response to metabolic acidosis. More recent studies in subjects on chronic lithium therapy and in rats chronically exposed to lithium have demonstrated that lithium increases basal renal ammonia excretion and the ability to increase ammonia excretion after an acid load (Weiner et al. Increased ammonia excretion was likely related to increased expression of the ammonia transporter protein Rhesus C glycoprotein in the outer renal medulla (Weiner et al. In rats, but not humans, chronic lithium exposure also increases urinary citrate excretion, perhaps by inhibiting proximal tubule apical citrate transporter sodium/dicarboxylate-1 (Weiner et al. Note the findings of interstitial fibrosis, tubular atrophy, and interstitial lymphocytic infiltration. Similar chronic tubulointerstitial abnormalities were observed in psychiatric patients who never received lithium, suggesting that there may not be a causal relationship between chronic tubulointerstitial disease and lithium therapy (Davies and Kincaid-Smith, 1979; Kincaid-Smith et al. When renal biopsy specimens from lithium-treated patients were compared with specimens from 25 patients with affective disorders who had never received lithium, there was no difference in the degree of interstitial fibrosis (Walker et al. The only characteristic that distinguished lithium-treated patients was the finding of microcysts. Other investigators have shown that renal abnormalities are more pronounced in patients treated with lithium in combination with neuroleptics than in patients treated with lithium alone (Bucht and Wahlin, 1980). Some investigators have suggested that characteristics shared by patients with affective disorders, such as the use of other psychotropic medications, may be responsible for tubulointerstitial damage that had been attributed to lithium therapy. Tubular atrophy and interstitial fibrosis that tended to be patchy in early cases were the predominant findings. A sparse, predominantly lymphocytic interstitial infiltrate was frequently seen in association with interstitial fibrosis. In two-thirds of the cases, sparsely distributed tubular cysts, not exceeding 12 mm in diameter, were seen. Focal and segmental glomerulosclerosis was present in half the cases and involved 620% of glomeruli. Additional features included frequent glomerulomegaly and variable podocyte effacement in the absence of electron-dense deposits. Nephrotoxicity of Lithium and Drugs of Abuse 319 Although chronic tubulointerstitial nephropathy is a nonspecific pattern of renal injury, specific renal lesions have been attributed to lithium exposure (Farres et al. Lithium increases the mitotic rate of collecting duct cells and induces marked principal cell hypertrophy (Christensen et al. Approximately 50% of lithium-treated patients with interstitial nephritis show tubular cysts of distal tubule and collecting duct origin, often in association with lesser degrees of tubular dilation (Hansen et al. Lithium-treated New Zealand white rabbits develop progressive renal failure and chronic tubulointerstitial injury associated with identical tubular microcysts (Walker et al. The specificity of these tubular microcysts is suggested by the fact that they are observed in lithiumtreated psychiatric patients with tubulointerstitial nephritis but are not observed in psychiatric patients with chronic tubulointerstitial nephritis who were never treated with lithium (Walker et al. They identified bilateral renal microcysts, typically 12 mm in diameter, in both the renal cortex and the medulla of normal-sized kidneys, which were distributed in a uniform and symmetrical manner in normal-sized kidneys. Nonenhanced magnetic resonance imaging and contrast-enhanced computerized tomography, and renal sonography have also been used to identify microcysts (Di Salvo et al. However, magnetic resonance imaging is more sensitive than other modalities in identifying microcysts as hyperintense foci on T2-weighted images. Microcysts may appear as punctate hypodense foci on contrast-enhanced computerized tomography. Microcysts that are too small to resolve and that may escape detection by this technique may appear as nonshadowing punctate echogenic foci on renal sonography (Di Salvo et al. The presence of microcysts does not correlate with renal function and may be seen in lithium-treated patients with normal renal function (Farshchian et al. Reversible cytoplasmic lesions have also been described in the distal tubules of lithium-treated patients, which were absent in psychiatric controls who had never received lithium (Burrows et al. These lesions consist of vacuolar swelling and glycogen accumulation and have been reproduced in the distal convoluted tubules and collecting ducts of lithiumtreated rabbits (Walker et al. Isolated case reports and case series have described an association between chronic lithium use and increased risk of benign and malignant tumors of the upper urinary tract (Kjaersgaard et al.
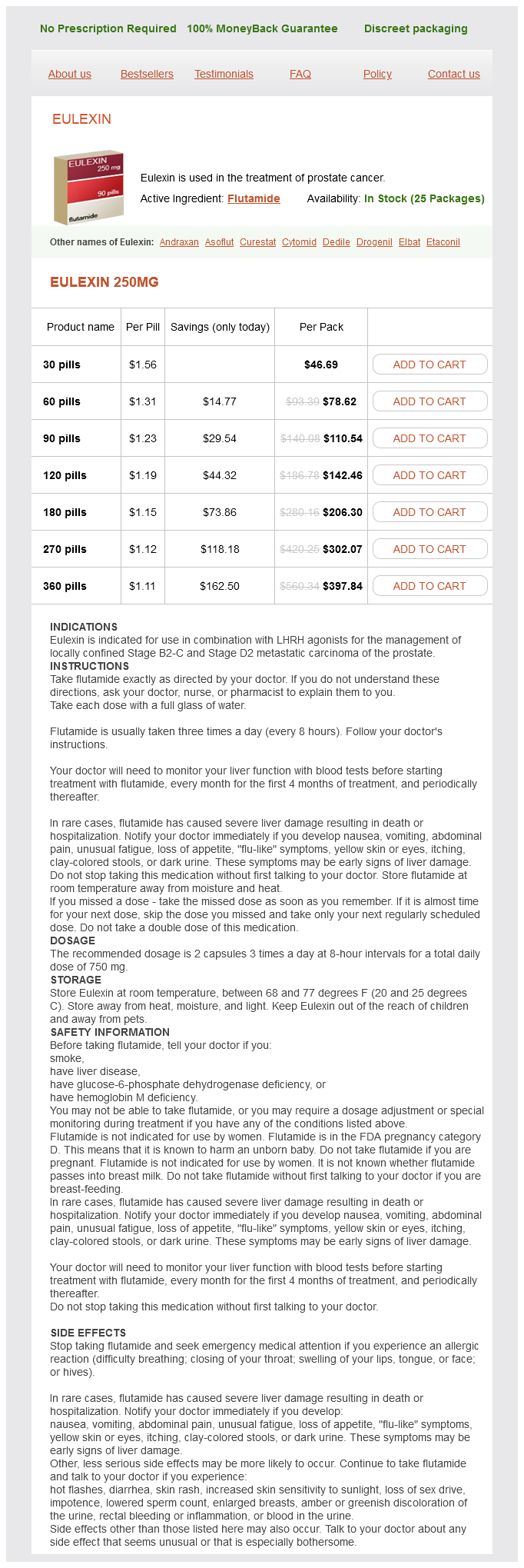
Flutamide Dosage and Price
Eulexin 250mg
- 30 pills - $46.69
- 60 pills - $78.62
- 90 pills - $110.54
- 120 pills - $142.46
- 180 pills - $206.30
- 270 pills - $302.07
- 360 pills - $397.84
Disease outcomes following pre- and early postnatal exposures cover a broad range of physiologic processes; many of which constitute major public health concerns treatment 32 for bad breath cheap 250 mg flutamide with mastercard. Obesity, diabetes, hypertension, cardiovascular disease, immune and autoimmune diseases, neurodevelopmental and neurodegenerative diseases, fertility, cancers, depression, psychiatric disorders, and finally lung disease all have origins, at least in part, in early-life environmental exposures (reviewed in Heindel et al. The Fourth Conference on Prenatal Programming and Toxicity in Boston, in 2014, focused on the connections between early environmental exposures and later onset disease, as well as the substantial role that the placenta plays in influencing development and programming of disease (Grandjean et al. Developmental programming following adverse environmental exposures during development results in alterations in the normal developmental trajectory and "programs" changes in the structure or function of an organ. Alternatively, programming can be more subtle; producing effects not obvious until later in life, or producing effects not elicited until the organ is faced with an additional stressor (Table 1). Understanding of the developmental programming of lung disease is an important public heath directive which has gained momentum over the last decade (Stocks et al. The adverse environmental exposures best understood in the context of programming of lung disease occur during the second half of human gestation, or in the early postnatal periodda time collectively referred to as the perinatal period. The perinatal period corresponds to periods of ongoing development of a number of organs, including the lung (Burri, 1984). A wide range of adverse exposures have been studied in the context of programming of lung disease. Some adverse exposures affect the fetus/neonate directly, while some adverse exposures affect the fetus secondary to effects on the placenta. Table 1 Aspects of environment and chemical exposures on developmental programming Functional l Developmental Exposure act during specific windows of developmental plasticity l Exposures result in sex-divergent effects l Genetic l Exposure interacts with fixed genetic Exposures cause subtle functional changes which may not be apparent without a second components l Exposures act via alteration in epigenetic marks hit later in life l Latency between exposure and disease/ which may be irreversible l Exposure effects can be transmitted via the dysfunction germ line to future generations Adapted from Heindel, J. Endocrinology 156, 34163421 Environmental Exposures and Developmental Programming of the Lung 15. The placenta acts as the lifeline for the fetus, providing nutrients and oxygen to the fetus while removing waste products from the fetal circulation. Another important function of the placenta is to protect the fetus from potential toxic substances. Disruption of placental development and function by environmental exposures therefore effects fetal development; often quite profoundly. An understanding of basic placental biology is necessary to appreciate the effects of toxic exposures on placental function. The origins of the placenta are the trophoblast cells surrounding the blastocyst and early embryo. The trophoblasts facilitate implantation of the embryo into the maternal uterine wall, rupturing maternal capillaries and establishing an interface between maternal blood and the embryonic extracellular fluid. In normal placentation the embryonic vessels, covered by fetal stem cells called cytotrophoblasts, give rise to the fetal chorionic villi which further branch into smaller, terminal villi, and form the interface between maternal and fetal blood flow. When cytotrophoblasts invade the uterine wall, and disrupt the smooth muscle of maternal vessels, spiral arteries are formed in the uterine decidua. This invasion transforms the maternal vasculature to a low-resistance, high-capacitance system and permits increased blood flow to the fetal side. The projections are surrounded by multinucleated syncytiotrophoblasts which secrete hormones that protect the pregnancy and maintain the uterine lining until the syncytiotrophoblast is mature enough to support the pregnancy at approximately the 4th month of gestation. Maternal blood from the spiral arteries surrounds the terminal villi and syncytiotrophoblast layer, providing the primary location for maternal-fetal exchange of nutrients and oxygen (Burton and Fowden, 2015). Environmental exposures frequently result in alterations in placental vascularity and function. Maternal tobacco use contributes to programming of the fetus directly via effects of nicotine and other toxic metabolites, as well as indirectly via effects on the placenta. Notably, incidences of maternal smoking during the last 3 months of pregnancy are as high as 29% in some states. Maternal tobacco smoke exposure has been linked to a number of negative effects on the developing fetus. Evidence from epidemiological studies supports the link between maternal tobacco smoke exposure and negative effects on lung function, as well as increased wheezing and asthma (Cunningham et al. Of these chemicals, nicotine and carbon monoxide are the best studied agents for adverse effects on the fetus during pregnancy. Nicotine and carbon monoxide both readily cross the placenta from the maternal to the fetal side. Human studies have demonstrated that nicotine levels are 15% higher in fetal circulation and 88% higher in the amniotic fluid than in maternal plasma (Luck et al. Nicotine reaches peak concentrations in the fetus after 1530 min and is rapidly distributed throughout the fetus with high affinity to the brain, heart, and lungs. Cotinine is often used as a biomarker for smoking because it has a longer half-life than nicotine, 17 h for cotinine versus 2 h for nicotine. Nicotine clearance is mainly determined by hepatic blood flow, while the clearance of cotinine is dependent on the activity of liver metabolizing enzymes. Carbon monoxide, another by-product of tobacco smoke, leads to fetal hypoxia via multiple mechanisms. Due to its ability to freely cross the placenta, carbon monoxide reaches the fetal circulation and binds to fetal hemoglobin. Fetal blood and tissue have lower oxygen partial pressures than the maternal circulation which helps the fetus to extract oxygen from the maternal blood. However, this mechanism also predisposes the fetus to profound tissue hypoxia, when carbon monoxide displaces oxygen from hemoglobin to form carboxyhemoglobin (Venditti et al. In response to such carbon monoxide-induced hypoxia, the fetus 150 Environmental Exposures and Developmental Programming of the Lung redistributes blood flow from nonessential tissues such as skeletal muscle, to essential tissues in order to preserve its brain, heart, and adrenal function. Multiple studies have assessed the effects of maternal tobacco smoke on the placenta. While studies are beginning to undercover mechanisms by which tobacco smoke affects the placenta, much still remains unclear. Cytotrophoblasts invade the maternal vasculature, forming high-capacity spiral arteries that permit increased blood flow to the fetus.