Fosamax
General Information about Fosamax
Fosamax can be used to deal with glucocorticoid-induced osteoporosis. Glucocorticoids, also referred to as steroids, are used to treat numerous medical circumstances such as asthma, rheumatoid arthritis, and lupus. However, prolonged use of these drugs may end up in bone loss. Fosamax helps increase bone density in people taking steroids, decreasing their risk of osteoporosis.
Moreover, Fosamax can be permitted to be used in men who have osteoporosis. Although males are much less likely to develop osteoporosis in comparability with girls, they can still be affected. Fosamax has been proven to increase bone mass in males, making their bones stronger and less vulnerable to fractures.
One of the commonest causes of osteoporosis in women is menopause. During this stage, the body produces less estrogen, a hormone that helps keep bone density. This lower in estrogen leads to bone loss, making postmenopausal ladies extra vulnerable to osteoporosis. Fosamax has been confirmed to be efficient in stopping and treating osteoporosis in postmenopausal ladies.
Fosamax just isn't appropriate for everybody, and sure medical conditions can affect its effectiveness. It is crucial to inform your doctor in case you have any kidney disease, vitamin D deficiency, or are unable to take a seat or stand upright for no less than 30 minutes. Additionally, it isn't recommended for pregnant or breastfeeding girls.
Fosamax, also identified by its generic name alendronate, is a prescription medication that belongs to a class of medicine called bisphosphonates. It is used to deal with and forestall osteoporosis in each men and women. Fosamax works by slowing down the breakdown of bone and rising bone density, thus lowering the danger of fractures.
Like any medicine, Fosamax also has its share of side effects. Some common unwanted aspect effects of Fosamax embrace mild gastrointestinal signs similar to nausea, indigestion, and diarrhea. In uncommon circumstances, it can lead to more severe unwanted effects, similar to jaw bone issues (osteonecrosis), esophageal ulcers, and irregular heartbeat. It is essential to inform your physician should you experience any of these signs whereas taking Fosamax.
Fosamax is available in two varieties – a tablet and an oral resolution. The pill is normally taken once per week, whereas the oral resolution is taken once a day. It is beneficial to take Fosamax on an empty stomach within the morning with a full glass of water. It is crucial to observe the dosing instructions offered by your doctor fastidiously. This medication should be taken consistently to get one of the best results.
Osteoporosis is a common condition that affects hundreds of thousands of people, especially women after menopause. It is characterised by low bone density, making bones weaker and more prone to fractures. In the United States alone, over 10 million folks have osteoporosis, and virtually 80% of them are women. To fight this condition, a number of medicines have been developed, and one such drug is Fosamax.
Another condition that Fosamax is used to treat is Paget's illness of bone. This is a continual situation the place there might be abnormal bone progress, leading to weak bones which might be extra prone to fractures. Fosamax helps regulate the bone growth, reducing the chance of fractures and enhancing bone power.
In conclusion, Fosamax is a extensively used medication for treating and preventing osteoporosis in each women and men. Its ability to extend bone density and cut back the chance of fractures has made it a preferred alternative amongst docs and patients. However, it is important to observe the dosing instructions carefully and inform your physician of any side effects or medical circumstances before beginning Fosamax. With correct use, Fosamax might help enhance bone health and high quality of life for those affected by osteoporosis.
Some viral infections can cause hemorrhagic fever characterized by fever menstruation gas bloating fosamax 35 mg purchase, hypotension, bleeding, and renal failure. Amniotic fluid embolism is a rare but serious complication of pregnancy and delivery. A maternal mortality rate of 86% was reported in a 1979 review of 272 cases, but in a more recent population-based study, the maternal mortality was 26%. Patients predisposed to amniotic fluid embolism are multiparous women whose pregnancies are postmature with large fetuses and women undergoing a tumultuous labor after pharmacologic or surgical induction. Amniotic fluid is introduced into the maternal circulation through tears in the chorioamniotic membranes, rupture of the uterus, and injury of uterine veins. Mechanical obstruction of pulmonary blood vessels by fetal debris, meconium, and other particulate matter in the amniotic fluid enhances local fibrinplatelet thrombus formation and fibrinolysis. The extensive occlusion of the pulmonary arteries and an acute anaphylactoid response reminiscent of severe systemic inflammatory response syndrome provoke sudden dyspnea, cyanosis, acute cor pulmonale, left ventricular dysfunction, shock, and convulsions. These symptoms are followed within minutes to several hours by severe bleeding in 37% of patients. Hemorrhage is particularly severe from the atonic uterus, puncture sites, gastrointestinal tract, and other organs. In a large series of patients, a good correlation was noted between the clinical severity and abnormalities in platelet counts and fibrin(ogen) degradation products. Despite these observations, administration of heparin to patients with preeclampsia and eclampsia has not resulted in convincing benefits. Interactions of P- and L-selectins with mucin from mucinous adenocarcinoma can induce the formation of platelet microthrombi, which probably constitute a third mechanism of cancer-related thrombosis. With some large aortic aneurysms, localized consumption of platelets and fibrinogen can produce coagulation abnormalities and bleeding. Kasabach and Merritt were the first to describe bleeding in association with giant cavernous hemangiomas, benign tumors found in newborns or children that can evolve into convoluted masses of abnormal vascular channels that sequester and consume platelets and fibrinogen. Localized pain may occur, likely from thrombosis of these vascular channels and there may be bleeding after trauma or surgery because of the consumptive process. Patients with this syndrome exhibit accelerated platelet turnover, and accumulation of labeled platelets and fibrinogen in the hemangiomas. Hemangiomas may regress spontaneously; some respond to radiation or laser therapy. Thrombocytopenia is common because of hypersplenism and decreased hepatic production of thrombopoietin. These include a reduced half-life of radiolabeled fibrinogen that is reversed with heparin administration; failure of replacement therapy to significantly increase the levels of hemostatic factors (suggesting ongoing consumption); and increased levels of markers of activation of coagulation. These large multimers promote platelet-vessel wall interaction, which can lead to thrombotic microangiopathy and organ dysfunction. Therefore the fibrinogen level may remain within the normal range for a long period of time despite ongoing consumption. Latex agglutination assays can be used for rapid point-of-care determination in emergency cases. Unfortunately there are no reliable tests to quantify plasma levels of soluble fibrin. Since plasma levels of soluble fibrin reflect intravascular fibrin formation, the test is not influenced by extravascular fibrin formation, which can occur with local inflammation or trauma. Venoms of these snakes contain enzymes or peptides that (1) release fibrinopeptide A (Agkistrodon rhodostoma); (2) activate prothrombin even in the absence of calcium (E. However, only 35% to 44% of critically ill patients develop thrombocytopenia (platelet count <150 × 109/L). In patients with meningococcal septicemia, plasma levels of protein C are markedly reduced, which likely contributes to the purpura fulminans that occurs in these patients. The low levels reflect consumption due to ongoing thrombin generation, decreased synthesis, and degradation by neutrophil elastase. However, because the normal plasma concentration of 2antiplasmin is about half that of plasminogen, 2-antiplasmin is susceptible to consumption when there is excessive plasmin generation. With 2-antiplasmin consumption, other protease inhibitors, such as antithrombin, 2-macroglobulin, 1-antitrypsin, and C1-inhibitor may act as plasmin inhibitors as well. Score global coagulation test results Platelet count (>100 = 0; <100 = 1; <50 = 2) Level of fibrin markers. The major difference between the international and Japanese scoring systems is a slightly higher sensitivity of the Japanese algorithm, which may reflect differences in the patient populations because the Japanese series include relatively large numbers of patients with hematologic malignancies. A complicating factor is that patients may have multiple explanations for their coagulopathy. Sepsis itself is a risk factor for thrombocytopenia in critically ill patients and the severity of sepsis correlates with the extent of thrombocytopenia. The principal factors that contribute to thrombocytopenia in patients with sepsis are decreased platelet production, increased consumption or destruction, or sequestration platelets in the spleen or on the endothelial surface. Platelet production is impaired because of hemophagocytosis, a pathologic process characterized by phagocytosis of megakaryocytes and other hematopoietic cells by monocytes and macrophages. This may result in platelet activation and consumption and arterial and venous thrombosis. Using receiver-operating characteristic curves, an optimal D-dimer cut-off was identified, thereby optimizing the sensitivity and the negative predictive value of the test. A common pathogenic feature of these disorders is endothelial damage, which triggers platelet adhesion and aggregation, thrombin generation, and an impaired fibrinolysis. The clinical consequences of extensive endothelial dysfunction include thrombocytopenia, mechanical fragmentation of red cells with hemolytic anemia, and microvasular occlusion, which leads to multiorgan dysfunction, including renal insufficiency and neurologic symptoms.
Denuding injury to the vessel wall also exposes tissue factor constitutively expressed by subendothelial fibroblasts and smooth muscle cells menstruation with iud order genuine fosamax line. In addition to cells in the vessel wall, circulating monocytes and monocyte-derived microparticles (small membrane fragments) also provide a source of tissue factor. However, the physiologic mechanism for activation of the pathway remained unclear until studies showed that nuclear material released from neutrophils in the form of neutrophil extracellular traps, nucleic acids, and inorganic polyphosphates released from activated platelets or microorganisms, activated coagulation in a contact pathwaydependent fashion. With a valid association between the contact pathway and physiologic activators, investigation into the role of the contact pathway in thrombosis exploded. Similar interest in targeting the contact pathway is directed at device-related thrombosis. Thrombosis is a major cause of failure of blood-contacting medical devices, a problem that can lead to life-threatening complications including pulmonary embolism, coronary occlusion, and stroke. Therefore the contact pathway has emerged as an attractive target for development of agents that reduce thrombosis with little impact on hemostasis. By binding to adhesion molecules expressed on activated endothelial cells or to P-selectin on activated platelets, these tissue factorbearing cells or microparticles can initiate or augment coagulation. This phenomenon likely explains how venous thrombi develop in the absence of obvious vessel wall injury. The decryption step is thought to occur by a disulfide bond rearrangement catalyzed by protein-disulfide isomerase and exposure of phosphatidylserine on the outer membrane surface. Because sufficient levels of factor Xa and thrombin are formed in response to exposure of tissue factor, the extrinsic tenase complex is considered the essential mediator of the initiation phase. For this reason, the contact pathway lost prominence when the physiologic tissue factor pathway was identified. We cannot ignore the contact pathway, however, because catheters and other blood-contacting medical devices, such as stents or mechanical valves, likely trigger clotting through this mechanism. The high levels of thrombin produced during the amplification phase are controlled by antithrombin. Although antithrombin is abundant, it exhibits only moderate inhibitory activity, except in the presence of cell-associated glycosaminoglycans, such as heparan sulfate. This is the biochemical basis for use of heparin as an anticoagulant (see Chapter 149). Further regulation of thrombin generation is mediated by the protein C anticoagulant pathway which is catalyzed by thrombin. Surface Common Pathway Fibrin Formation Thrombin converts soluble fibrinogen into insoluble fibrin. Fibrinogen is a dimeric molecule, each half of which is composed of three polypeptide chains, the A, B, and chains. Electron micrographic studies of fibrinogen reveal a trinodular structure with a central E domain flanked by two D domains. Crystal structures show symmetry of design with the central E domain, which contains the amino termini of the fibrinogen chains, joined to the lateral D domains by coiledcoil regions. Because they are products of thrombin action on fibrinogen, plasma levels of these fibrinopeptides provide an index of thrombin activity. Fibrinopeptide release creates new amino termini that extend as knobs from the E domain of one fibrin monomer and insert into preformed holes in the D domains of other fibrin monomers. This creates long strands known as protofibrils, consisting of fibrin monomers noncovalently linked together in a half-staggered, overlapping fashion. Hemostasis depends on the dynamic balance between the formation of fibrin and its degradation. Prothrombinase Being the only physiologic producer of thrombin, the prothrombinase complex is essential for hemostasis. Factor Xa binds to factor Va, its activated cofactor, on anionic phospholipid membrane surfaces to form the prothrombinase complex. Activated platelets release factor V from their -granules, and this platelet-derived factor V may play a more important role in hemostasis than its plasma counterpart. Activated platelets express specific factor Va binding sites on their surface, and bound factor Va serves as a receptor for factor Xa. The catalytic efficiency of factor Xa activation of prothrombin increases by 105-fold when factor Xa incorporates into the prothrombinase complex. Prothrombin is the most abundant coagulation factor, and the efficiency of activation generates high local levels of thrombin. FibrinolyticSystem Fibrinolysis initiates when plasminogen activators convert plasminogen to plasmin, which then degrades fibrin into soluble fragments. Thus the termination phase plays a critical role in balancing the procoagulant forces. A dimeric molecule, each half of fibrinogen is composed of three polypeptide chains, A, B, and. Numerous disulfide bonds (lines) covalently link the chains together and join the two halves of the fibrinogen molecule to yield a trinodular structure with a central E domain linked via the coiled-coil regions to two lateral D domains. Fibrin monomers polymerize to generate protofibrils arranged in a half-staggered overlapping fashion. The substrate of the fibrinolytic system, fibrin, serves a transient but essential stimulatory role that subsides as it degrades. Native Glu-plasminogen is a single-chain polypeptide with a Glu residue at its amino-terminus. Plasmin cleavage near the aminoterminus generates Lys-plasminogen, a truncated form with a Lys residue at its new amino terminus. Kringle domains are triple loop-like structures that bind Lys residues on fibrin and other proteins.
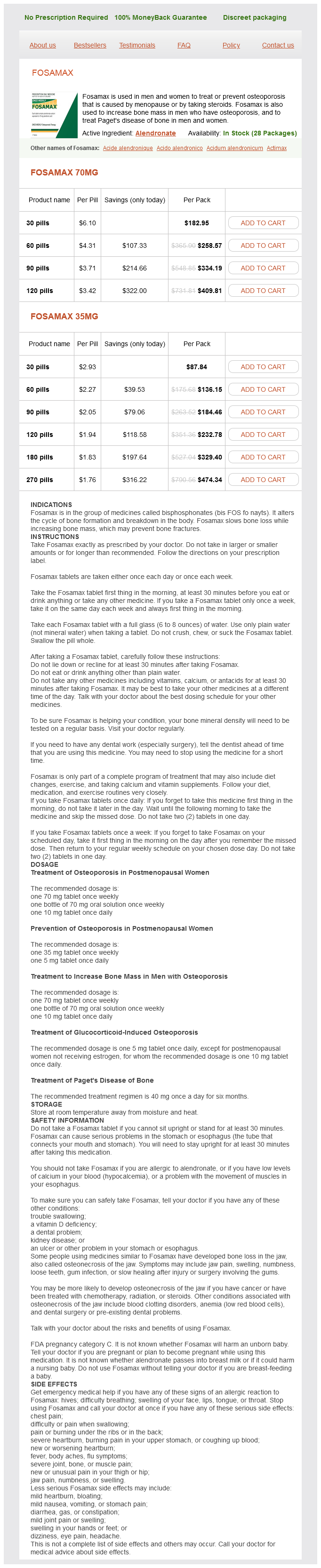
Fosamax Dosage and Price
Fosamax 70mg
- 30 pills - $182.95
- 60 pills - $258.57
- 90 pills - $334.19
- 120 pills - $409.81
Fosamax 35mg
- 30 pills - $87.84
- 60 pills - $136.15
- 90 pills - $184.46
- 120 pills - $232.78
- 180 pills - $329.40
- 270 pills - $474.34
Because the drug is being infused in close proximity to the spinal cord menstruation disorders discount fosamax 35 mg without a prescription, only a small amount of opioid is needed, and the systemic side effects are reduced. Problems with this delivery system in patients who are not opioid naive include pruritus, respiratory depression, and sedation. If tolerance to the opioid develops and higher doses are required for relief, the incidence of side effects may approach that of systemically administered opioids. Modafinil (Provigil), a novel psychostimulant with a mechanism of action different than the amphetamine derivatives, which is approved for narcolepsy and fatigue related to multiple sclerosis, has also been found to be effective for opioid-related sedation. Detailed bowel preparation recommendations can be found, but no regimen has been studied in a controlled fashion. Commonly used stool softeners and stimulants include docusate sodium, senna, lactulose, and polyethylene glycol. A combination of a stool softener and laxative seems to be a rational choice for patients taking chronic opioids. Promotility agents most directly counter the mechanism of opioid-induced constipation. Bulk-forming laxatives such as psyllium and methylcellulose should be avoided because they increase stool volume without promoting peristaltic action. For refractory opioid-induced constipation, a trial of oral naloxone, methylnaltrexone, or alvimopan may be initiated. There is minimal systemic absorption with oral naloxone and subsequently a low risk of precipitating opioid withdrawal or worsening pain at low-to-moderate doses (1. Methylnaltrexone (administered subcutaneously)9 and alvimopan (oral) do not cross the bloodbrain barrier and therefore do not cause opioid withdrawal or worsening pain. Transmucosal Route Subcutaneous and Intravenous Routes Nausea Prochlorperazine (10 mg taken two or three times daily) or metoclopramide (10 mg taken three to four times daily) can prevent the nausea that occurs in most patients during the first days of opioid therapy. Rarely, patients need oral or intravenous ondansetron (8 mg taken two or three times daily). Respiratory Depression Naloxone (Narcan), given intravenously, reverses opioid-induced respiratory depression, although repeated doses are often required. Caution should be exercised before administering naloxone to patients who are chronically receiving opioids to avoid precipitation of severe pain and withdrawal. Corticosteroids given epidurally, intravenously, or orally are useful as antineoplastics. Doses of 16100 mg of dexamethasone are needed to reduce vasogenic edema in spinal cord compression,9 but lesser doses (620 mg/day) can be helpful in patients with plexus injuries. Patients must be monitored for the development of oral or esophageal candidiasis and steroid-induced delirium. Calcium and sometimes vitamin D supplementation (especially for denosumab) are often needed. AdjuvantAnalgesics Adjuvant analgesics are a diverse class of medications, which typically have indications for conditions other than pain. They have analgesic properties and are often used when an opioid regimen alone is unable to provide sufficient analgesia or is associated with dose-limiting side effects. The effective dose of gabapentin varies between 900 and 3600 mg/day in divided doses and that of pregabalin is 150300 mg twice a day. The pharmacokinetics of gabapentin are unique in that it has a ceiling effect related to a saturable transport mechanism in the gut, such that the effects of this drug may plateau during dose escalation. Gabapentin and pregabalin need to be renally dosed in patients with decreased creatinine clearance. Other, generally less effective anticonvulsants used for neuropathic adjuvants include phenytoin, carbamazepine, lamotrigine, topiramate, and tiagabine. However, because of their anticholinergic side effects they should be started at doses of 1025 mg Cannabinoids Long used empirically for their analgesic and antiemetic properties in a wide range of illnesses, cannabis and cannabinoid therapies have been subjected to an increasingly large number of controlled clinical trials (of varying size and quality) over the last several decades. The study showed analgesic efficacy in the low and medium dose ranges, which were also well tolerated. Additional studies have provided evidence for its effect on spasticity, appetite stimulation, and insomnia. A thorough dental evaluation and prompt treatment of infections can minimize the discomfort arising from underlying periodontal disease and caries; secondary bacterial, viral, and fungal infections; and mucositis. Anesthetic cocktails composed of agents such as viscous lidocaine (Xylocaine), dyclonine hydrochloride, or a slurry of sucralfate, provide temporary relief from oral mucositis-related oral pain. A variety of mucosal-coating agents have been used to protect mucosal surfaces of the oral cavity including Orabase, Episil, oral antacids, and Gelclair. There is little evidence from randomized trials to support any benefit from these preparations. Gelclair, a bioadherent gel that adheres to the oral surface, creating a protective barrier for irritated tissue, showed a reduction in oral discomfort within 57 hours of initial treatment in an uncontrolled, open-label study of 30 hospice patients (only three of whom had chemotherapy-related mucositis). Pilocarpine (510 mg three times daily 1 hour before meals) may improve xerostomia from neck irradiation. However, caution is warranted because of reported side effects of glaucoma and cardiac problems. The anticonvulsant medications gabapentin, pregabalin, and valproic acid are especially useful in reducing the lancinating component of the various pain syndromes generated by this infection. A 2011 systemic review identified four placebo-controlled randomized trials, with two trials evaluating immediate-release gabapentin at doses between 1800 and 3600 mg daily showing benefit compared with placebo for the outcome of "much or very much improved" (38% vs. Topical lidocaine (5%) has been used for the relief of pain associated with postherpetic neuralgia; however, its role has not been established. Acute vasoocclusive pain may occur along with the chronic pain caused by the long-term complications of compression fractures, avascular necrosis, arthropathies, fractures, avascular necroses, and leg ulcers. Using short-acting analgesics on an "as-needed" basis exposes the patient to periods of insufficient analgesia, anticipation, and anxiety. Their repeated requests for medication to relieve their ongoing pain may be mistakenly interpreted as "drug-seeking behavior," and they may be unfairly stigmatized.