Glyburide
General Information about Glyburide
Micronase is not really helpful for use in folks with kind 1 diabetes, as it isn't efficient in stimulating insulin production in these with a non-functioning pancreas. It can also be not beneficial to be used in pregnant women or those with kidney or liver illness. Additionally, people with a sulfa allergy must also avoid using this medicine.
In conclusion, Glyburide, or Micronase, is a commonly prescribed treatment for kind 2 diabetes. By stimulating insulin manufacturing, it helps to lower blood sugar levels and improve overall blood sugar management. However, it is essential to work intently with a healthcare supplier, make needed life-style changes, and monitor blood sugar levels to successfully manage diabetes. With correct care and management, individuals with type 2 diabetes can live a healthy and fulfilling life.
Like all medications, Micronase does have potential side effects. The commonest side effects are low blood sugar (hypoglycemia) and upset abdomen. These side effects can typically be managed by adjusting the dosage or ensuring dietary adjustments. It is essential to discuss any unwanted facet effects with a healthcare provider to determine the most effective course of action.
Glyburide, also recognized by its brand name Micronase, is a medicine commonly prescribed for the therapy of kind 2 diabetes. This medicine, classified as a sulfonylurea, helps to decrease blood sugar levels by rising the quantity of insulin produced by the pancreas.
Micronase works by stimulating the beta cells in the pancreas to provide extra insulin. This helps to lower blood sugar ranges and improve the physique's ability to make use of insulin effectively. The treatment is typically taken once a day, with or with out meals, on the similar time each day to maintain constant ranges within the body.
When prescribed Micronase, it is essential to monitor blood sugar ranges often to ensure they stay within a healthy vary. The dosage may need to be adjusted based on these ranges, as well as different components corresponding to food plan, train, and overall well being. It is essential to observe the instructions of a healthcare supplier and make any needed dietary and way of life changes to successfully handle diabetes.
In some cases, Micronase may be used in combination with other diabetes drugs to higher handle blood sugar levels. This may embrace insulin therapy or other oral medications such as metformin. It is necessary to observe healthcare supplier instructions and continue monitoring blood sugar levels to ensure proper administration of diabetes.
Type 2 diabetes is a persistent situation during which the body either doesn't produce enough insulin or is unable to correctly use the insulin it produces. Insulin is a hormone that regulates blood sugar levels, allowing cells to soak up and use glucose for vitality. Without enough insulin, glucose builds up in the blood, resulting in excessive blood sugar levels. Over time, this could result in critical health issues corresponding to coronary heart disease, nerve harm, and kidney disease.
New aprons diabetes type 2 omega 3 proven glyburide 2.5 mg, which are not made of lead, can be as much as 50% lighter than a lead apron, making them more comfortable to wear and producing less fatigue. They are made from several layers of very light fabric; each layer absorbs a different wavelength of radiation but covers the same radiation spectrum as a lead apron. A thyroid collar reduces the exposure risk to the thyroid by approximately one-half. Additional measures that are helpful to reduce the overall amount of radiation exposure to both the patient and the staff include: 1. Intermittent use of the fluoroscopy with reduction in fluoroscopic frame rate to the minimum needed for visualization of pertinent catheter course and cardiac structures. Careful attention to catheter pressure tracings by the operator in order to correlate with catheter course on fluoroscopy. The field of interest should be centered in the detector, with appropriate filters, collimators in use, and the detector as close to the patient as possible. Angiography the importance of good technique when performing angiography cannot be overemphasized. It is preferable to deliver the bolus of contrast within one cardiac cycle, where feasible, in order to provide the opacification needed for detailed angiography. When positioned in a ventricle, a balloon-tipped angiographic catheter may cause less ectopy than other catheters. It is common during interventional procedures to make calibrated measurements of structures that are defined angiographically. During diagnostic studies, vessel size and ventricular function also can be quantitated in order to provide a thorough assessment of anatomy and function. More accurate measurements may be obtained using a marker catheter, which has radiopaque bands placed 1 or 2 cm apart (compared with a catheter that may be only 1 to 3 mm in diameter), but the x-ray beam must be perpendicular to the catheter to avoid foreshortening, which causes a calibration error. The most accurate method of calibration is that which is built into the imaging system itself, with the patient positioned at isocenter on the table, whereby automated calibration references allow for measurement of structures or vessels from stored fluoroscopic or angiographic images. As viewed from the flat panel detector, the image plane is perpendicular to a line drawn between the x-ray tube and the detector. Again, familiarity with the anatomy and structures that need to be defined during angiographic assessment is required, so that adjustments in camera angles can be made to optimize structural definition. An exhaustive discussion of the use of angled views in congenital heart disease is beyond the scope of this chapter; however, basic imaging of the biventricular heart and of several other common defects is discussed below. Right Ventricle and Pulmonary Arteries the right ventricle is most often imaged in the frontal (Video 16. Occasionally, 0 to 25 degrees of cranial angulation is added to the frontal plane detector to provide better definition of the outflow tract. Neither view displays the interventricular septum well as the normal right ventricle wraps around the left ventricle. The interventricular septum should be imaged from a left ventricular injection (unless there is simple transposition of the great arteries). Note the hinge points (arrows) of the thickened pulmonary valve that domes in systole and the narrow jet of contrast passing through the valve. In both views, there is significant poststenotic dilation of the main pulmonary artery. The mitral valve is indicated by the open arrow, and mitral insufficiency (if present) would be seen in this view. The mitral valve is visualized, and mitral insufficiency (if present) would be noted. A qualitative assessment of left ventricular function can be performed in this view, and when calibrated systems are in place, the ventricle can be measured in diastole and systole to provide ejection fraction and volumes. The aortic valve is imaged well from a left ventricular injection, and the leaflets should be thin and barely visible when normal. For atrioventricular septal defects (which are not commonly seen in the cath lab for purposes of diagnostic angiography but for determination of pulmonary resistance in the older patient) and posterior muscular ventricular septal defects, visualization of the inlet portion of the ventricular septum is required. For this, the lateral detector is moved to 40 degrees of leftward angulation and 40 degrees of cranial angulation, whereas the frontal camera has 30 degrees of rightward angulation. Central Pulmonary Arteries In some patients, particularly those who have tetralogy of Fallot, it is not possible to obtain sufficient cranial angulation to display the pulmonary artery bifurcation in the frontal plane view. In other cases, where this does not provide adequate visualization of the individual branches, extreme caudal angulation may display the central pulmonary artery bifurcation. Pulmonary Angiography through a Sano, Modified BlalockThomasTaussig Shunt, or Cavopulmonary Anastomosis Current Norwood stage I palliation for hypoplastic left heart syndrome is carried out with either a Sano modification or a modified BlalockThomasTaussig shunt as a source for pulmonary blood P. In patients with the Sano modification, a right ventricular injection may show the pulmonary arteries fairly well but the Sano shunt is better visualized in the lateral projection due to overlap of the structures in the frontal plane projection. A modified BlalockThomasTaussig shunt can be easily accessed with a soft-tipped catheter in order to perform an angiogram in the shunt; this provides definition of the shunt caliber and pulmonary artery branch anatomy. It is possible to directly measure pulmonary artery pressure if the catheter can be advanced through the shunt without hemodynamic embarrassment, and the tip is free without pressure dampening. Additional hand injections can be performed in the shunt with this catheter in order to demonstrate the anatomy more specifically. In some cases, the pulmonary arteries may be imaged without crossing the shunt, particularly if the patient has low saturations (unless intervention is anticipated). A balloontipped angiographic catheter can be advanced antegrade through the heart into the subclavian artery, distal to the origin of the shunt. The balloon is inflated, occluding the distal subclavian artery, while a power injection of 0. Pulmonary Vein Wedge Angiography Pulmonary vein wedge angiography may be necessary when the pulmonary arteries cannot be imaged by direct injection or by injection of an aortopulmonary shunt or aortopulmonary collateral (32). With free flow of blood upon drawing back on the syringe, a 5- to 12-mL syringe containing 1 to 4 mL of contrast (0.
Finally blood glucose to a1c conversion purchase glyburide 5 mg without prescription, the presence of a large left-to-right shunt may cause severe right ventricular enlargement with bowing of the septum to the left. To overcome the false impression of left ventricular hypoplasia on 2-D echocardiography, van Son et al. A: Diastolic frame from the subcostal sagittal imaging plane showing balanced ventricles. Due to right ventricular volume overload, the septum bows toward the left ventricle. However, if one assumes normalization of septal position, the potential volume of the left ventricle after repair may be predicted. However, despite use of all imaging assessments, practitioners must realize that none of the methods factor in patient/cardiac growth. Enlargement of the right atrium is suggested by increased convexity of the right heart border, and left atrial enlargement may produce a characteristic flattening of the left heart border. The pulmonary artery is prominent, and the pulmonary vascular markings are increased. In an older child, when pulmonary vascular obstructive disease is suspected, there is a role for determining pulmonary vascular resistance. Severe pulmonary vascular obstructive disease (pulmonary vascular resistance of >10 U·m2) is rare but has been reported in infants <1 year of age. Cardiac catheterization reveals increased oxygen saturation at both the right atrial and the right ventricular levels. Pulmonary blood flow is increased as a result of left-to-right shunting at both atrial and ventricular sites, and the degree of shunting depends upon the relationship of pulmonary to systemic vascular resistance. The timing of surgical intervention must account for development of pulmonary vascular disease in these patients at an early age. Children with associated Down syndrome may require surgical intervention at an earlier age due to their propensity to develop pulmonary vascular obstructive changes. In contrast, splenic anomalies and abnormalities of sidedness (situs) are rare in patients with Down syndrome. Others (55,56) have suggested that children with Down syndrome have pulmonary parenchyma hypoplasia and develop pulmonary vascular obstructive disease earlier than patients with normal chromosomes. These factors contribute to carbon dioxide retention, relative hypoxia, and elevated pulmonary vascular resistance. Patients with Down syndrome have a higher ratio of pulmonary to systemic resistance than patients without Down syndrome (57). This difference resolves with administration of 100% oxygen, suggesting that apparent hypoxia and hypoventilation are factors that can be corrected during hemodynamic evaluation. Fixed and elevated pulmonary vascular resistance has been demonstrated in 11% of Down syndrome patients <1 year of age (57). These objectives can be accomplished by careful approximation of the edges of the valve cleft with interrupted nonabsorbable sutures. On occasion, it is necessary to add eccentric annuloplasty sutures, typically in the area of the commissures to correct persistent central leaks. The repair is completed by closure of the interatrial communication (usually with an autologous or bovine pericardial patch), avoiding injury to the conduction tissue (59). However, the morphologic concepts and surgical methods, favored by Carpentier (60) and Piccoli et al. In that series, there was one surgical death, and the remaining patients had excellent palliation. Once the patch is sutured into place, the bridging leaflets are resuspended to the patch. Two-patch technique was used in 72% of cases, single-patch technique in 18%, and the Australian repair in 10%. Surgeons at many North American centers prefer to utilize a two-patch technique thereby avoiding division of the bridging leaflets (71). In an Australian report, the cleft was completely closed in 43%, partially closed in 20%, and left open in 36%. The bridging leaflets are sutured directly to the crest of the ventricular septum. Current recommendations are to close the zone of apposition, partially or completely, to reduce postoperative regurgitation. This will leave mild valve stenosis, which is usually well tolerated and may improve with time (75). Right or Left Ventricular Hypoplasia these anomalies may be severe enough to preclude septation. The only option for definitive surgical palliation is the Fontan procedure preceded by adequate pulmonary artery banding in infancy (78). In tetralogy of Fallot, there is obstruction of the right ventricular outflow tract. These cyanotic infants often initially are treated with a systemic-to-pulmonary artery shunt and then with "complete repair" at 2 to 4 years of age. The intracardiac repair of these hearts is best accomplished through a combined right atrial and right ventricular approach (51). Subaortic Stenosis If discovered at the time of initial preoperative evaluation, subaortic stenosis tends to be of the fibromuscular membrane type and should be treated by appropriate resection during surgical repair. The obstruction usually is due to the formation of endocardial fibrous tags and fibromuscular ridges. Usually it can be treated by local resection, although in some patients a modified Konno procedure may be necessary (79,80,81,82). Repeat valve repair is possible if the dysplasia is not severe or when the mechanism of regurgitation is through a residual cleft. Patientprosthetic mismatch in patients who required valve replacement during infancy or early childhood will merit valve re-replacement.
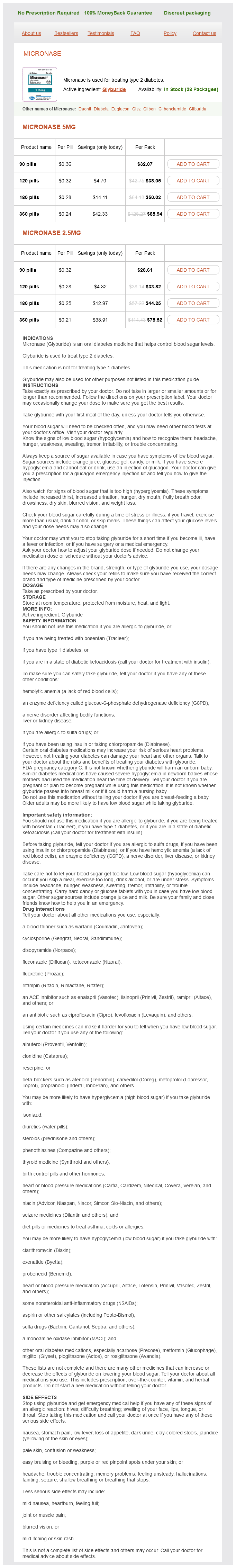
Glyburide Dosage and Price
Micronase 5mg
- 90 pills - $32.07
- 120 pills - $38.05
- 180 pills - $50.02
- 360 pills - $85.94
Micronase 2.5mg
- 90 pills - $28.61
- 120 pills - $33.82
- 180 pills - $44.25
- 360 pills - $75.52
Transhepatic vascular access for diagnostic and interventional procedures: techniques definition de la diabetes 5 mg glyburide purchase otc, outcome, and complications. Feasibility of pulmonary artery pressure measurements in infants through aorto-pulmonary shunts using a micromanometer pressure wire. Diagnostic reference levels and effective dose in paediatric cardiac catheterization. Visualization of the pulmonary arteries in pseudotruncus by pulmonary vein wedge angiography. Enlarged bronchial arteries after early repair of transposition of the great arteries. Hazards of cardiac catheterization in children with primary pulmonary vascular obstruction. The use of heparinization to prevent arterial thrombosis after percutaneous cardiac catheterization in children. Cheatham Introduction Catheter-based techniques, whether palliative or corrective, are the accepted therapy for many congenital cardiac defects. Interventional, or, better termed, therapeutic catheterizations, were initiated by Dotter and Judkins, who first reported the treatment of peripheral vascular lesions during a catheterization in 1964 (1), when they dilated a stenotic peripheral vessel through a cutdown on the vessel. The next major innovative accomplishment and the first intracardiac therapeutic catheterization procedure for pediatric congenital heart disease were the balloon atrial septostomy done by Rashkind and Miller in 1966 (2). That procedure really "set the stage" for all therapeutic catheterization procedures used today. In 1967, Porstmann and colleagues reported the first nonsurgical corrective procedure in the catheterization laboratory with their description of a technique for closure of a patent ductus (3). Even though their device has not found widespread use, it set the stage for future development of transcatheter devices. One of the largest contributions to interventional cardiology has probably been made by Gruentzig, a Swiss-native who in 1976 reported on dilation of peripheral vessels with noncompliant balloons. Jean Kan reported the first successful transcatheter static balloon pulmonary valvuloplasty (6) and Dr. Phillip Bonhoeffer, a German cardiologist working in France in 2000, performed the first transcatheter pulmonary valve replacement in a human (9). Transcatheter valve therapies and other interventional therapies to treat patients with structural heart disease have rapidly increased over the last few years. These therapies are not limited anymore to patients with congenital heart disease. In this section, the most important therapeutic catheterization procedures performed as of this writing are discussed. Acknowledgment We have used and expanded upon this chapter published in other editions of this textbook and therefore acknowledge the previous contributions made by Drs. It should be emphasized that not every pediatric cardiologist, or, for that matter, every center, should offer every therapeutic catheterization procedure. For any procedures to be performed at any particular institution, minimal specific skills are required, special techniques must be mastered and maintained, and a large inventory of specialized and expensive catheters and devices must be stocked to offer the patient an optimal procedure. Absence of appropriate qualifications and equipment can result in unnecessary risk to the patient without a reasonable chance of the therapeutic catheterization procedure being successfully accomplished. In fact, even if the patient is not acutely harmed by the attempt, it is important to be aware of the fact that the next procedure in a more appropriate setting might be compromised by a previously unsuccessful attempt. Adverse Events and Quality Improvement For many years, reporting of procedure-related adverse events was limited mostly to single-center retrospective experiences, often without any clearly and consistently applied criteria of what would be considered an adverse event, and how its severity should be defined (11,12,13). The data derived from these registries often provided the only prospective multicenter outcome data for many procedure types. This registry documented not insignificant rates of adverse events, 10% for diagnostic cases, and 20% for interventional procedures. Higher severity (level 3 to 5) adverse events occurred in 9% of interventional cases, and 5% of diagnostic cases. The incidence of life-threatening adverse events has been reported to be as high as 2. Following the definition of procedure-type risk groups, Bergersen and colleagues reported on hemodynamic variables associated P. The Interventional Armamentarium General Considerations the spectrum of transcatheter procedures available for the treatment of children and adults with congenital heart disease has rapidly increased over the last three decades. Even though many interventional meetings have a focus on new device developments, the choice of appropriate balloons, catheters, sheaths and wires is in many situations even more important for a successful outcome. It is beyond the scope of this discussion to describe all available balloon catheters, but the operator has to make a wellinformed decision on which balloon to use, based on profile, rated maximum pressure, available lengths, and degree of compliance and adjust his/her choice to suit specifically the therapeutic intervention that is intended. Even though transcatheter devices have long been available for the management of congenital cardiac lesions, the greatest progress has been made through introduction of a large variety of newer devices that were specifically developed for individual congenital cardiac lesions over the last 10 years. In this chapter, a variety of device-specific sections have been taken with permission from an article on this topic that was published in "Expert Review of Medical Devices" (29). The spectrum of devices that are discussed below is not intended to be complete, but rather represents subjective choices of the authors. Devices for the treatment of structural cardiac lesions or the treatment of acquired heart disease are not included in this chapter. The procedure was complicated and required a large arterial cannulation and as a result, this technique never found widespread use. Rashkind and Cuaso, while still working on the septostomy balloon, also developed a device for closure of the patent ductus.