Glycomet
General Information about Glycomet
Glycomet, also referred to as Metformin, is a generally prescribed medicine for the therapy of kind 2 diabetes. It is an oral medication that belongs to a class of medication known as biguanides and is primarily used to lower blood sugar ranges in folks with type 2 diabetes.
In conclusion, Glycomet is a highly effective medicine for managing type 2 diabetes. It helps to manage blood sugar ranges, promotes weight reduction, and has minimal unwanted facet effects. However, it is important to make use of it underneath the supervision of a well being care provider and at the facet of lifestyle modifications for optimum outcomes. Maintaining a healthy way of life, common monitoring of blood sugar ranges, and following the doctor’s directions are key to successfully managing diabetes with Glycomet.
Type 2 diabetes is a continual situation which affects millions of people worldwide. It is brought on by the body’s lack of ability to use insulin successfully, a hormone that regulates the quantity of sugar in the blood. This results in high blood sugar ranges, which can have serious problems such as heart illness, kidney failure, and nerve damage.
Unlike type 1 diabetes which is characterized by the body’s inability to provide insulin, sort 2 diabetes is a progressive illness that can be managed via a combination of healthy lifestyle decisions, including common train, proper diet, and drugs.
Another necessary facet to bear in mind whereas taking Glycomet is its potential interactions with other medicines. It is crucial to inform the physician about another medicines being taken to avoid any opposed effects.
The medication is often prescribed together with a healthy diet and exercise regime to effectively manage blood sugar ranges. It just isn't meant to replace these lifestyle modifications, but rather to enhance them. Glycomet is out there in various strengths from 500mg to 1000mg and is normally taken two to a few occasions a day with meals.
One of the main benefits of utilizing Glycomet is that it does not trigger hypoglycemia (low blood sugar). This is a typical side effect of other diabetes medicines such as insulin or sulfonylureas. Hypoglycemia may be life-threatening if left untreated, and Glycomet eliminates this concern for patients.
Glycomet works by lowering the production of glucose in the liver, decreasing the absorption of glucose within the intestines, and bettering the body’s sensitivity to insulin. This action helps to decrease blood sugar levels and prevents complications associated with high blood sugar.
Pregnant and breastfeeding girls are often advised not to take Glycomet, as it may harm the fetus or move via breast milk. Diabetic patients who expertise episodes of low blood sugar or these with kidney or liver diseases may also need nearer monitoring whereas taking Glycomet.
Moreover, Glycomet is also associated with weight reduction, which is an added benefit for individuals with diabetes who often struggle with managing their weight. The treatment doesn't improve the manufacturing of insulin, which is a significant factor in weight acquire. Instead, it works by bettering insulin sensitivity, which aids in weight loss.
Some different potential side effects of Glycomet may embrace gastrointestinal disturbances similar to nausea, vomiting, and diarrhea. These unwanted effects are usually delicate and may subside with continued use. In some rare cases, more extreme unwanted facet effects such as allergic reactions or lactic acidosis could occur. It is important to seek the advice of a health care provider instantly if any opposed reactions are skilled.
Although it is true that the very nature of natural or man-made disasters present unique and new challenges in every new presentation blood glucose keeps dropping discount glycomet master card, it is also true that many of these problems arise from the fact that, once disaster response plans are made, they often end stored and forgotten, and the teams eventually become untrained. The Institute of Medicine has reported that most children receive emergency care in general hospitals. Most of the communications occurred without significant technical issues, and in 40% of them telemedicine was used to supervise the critical care transport team. A survey reported high satisfaction among consulting and referring physicians, with most of the providers perceiving telemedicine as improving patient care, being superior to telephone conversations, and allowing good provider-to-provider communication. Communications occurred with the pediatric critical care fellow in 100%, nursing staff in 68%, and parents in 66% of their teleconsultations. Telemedicine will undoubtedly be an integral part of this new approach, perhaps enabling critical patients to be treated closer to their homes, family, friends, and support network while empowering local teams, providing best-evidence guidelines and quality assurance as well as accelerating the decision-making process to expedite definite treatment or else more compassionate, palliative, or end-of-life care. Integration through a continuum from home and the community to the critical care environment will incorporate early preventive strategies aimed at well-being preservation and risk avoidance, rather than the current reactive approach toward already established critical care disease, connecting presently disjointed practices in ambulatory medicine and critical care. Tele-pharmacy in remote medical practice: the Royal Flying Doctor Service Medical Chest Program. Evolution of telemedicine from an applied communication perspective in the United States. Harrison A, Thongprayoon Ch, Kashyap R, Chute C, Gajic O, Pickering B, Herasevich V. Developing the surveillance algorithm for detection of failure to recognize and treat severe sepsis. Enrollment into a time sensitive clinical study in the critical care setting: results from computerized septic shock sniffer implementation. Association of telemedicine for remote monitoring of intensive care patients with mortality, complications, and length of stay. A picture is worth a thousand words: critical care consultations to emergency departments using telemedicine. Nighttime telecommunication between remote staff intensivists and bedside personnel in a pediatric intensive care unit: a retrospective study. Impact of telemedicine on hospital transport, length of stay, and medical outcomes in infants with suspected heart disease: a multicenter study. International telemedicine in pediatric cardiac critical care: a multicenter experience. Lopez-Magallon A, Otero A, Welchering N, Bermon A, Castillo V, Duran A, Castro J, Muñoz R. The tele-intensive care unit during a disaster: seamless transition from routine operations to disaster mode. Delivering a carefully organized PowerPoint presentation, supervising problem-based workshops, or providing bedside clinical tutorials does not mean one has taught. Unless the learner has acquired new cognitive or psychomotor skills, teaching has not occurred. The focus of this model is on what the teacher did and not on what the learner learned. Said another way, a teacher is someone whose students learn, not one who presents well. The teacher as a "manager" creates specific educational objectives, motivates students, utilizes various educational strategies, evaluates learning, and provides effective feedback to ensure the learner achieves all the educational objectives. Therefore, many of the topics discussed in this chapter are still relevant, even those described by Bloom, Mager, and many other cited authors with works dating back to the 1960s. What has changed, however, are the learning environments medical trainees face, requirements by medical education governing bodies, and the ways students can learn through advancements in technology. The goal of this chapter is to provide a detailed description of each of these steps, from creating educational objectives to providing feedback, so the teacher can apply the concepts, whether organizing and presenting a 1-hour lecture, a 1-day workshop, a 1-month elective, or a 1-year curriculum. Objectives should be developed for every instructional activity because they are a road map. They guide the teacher in developing an appropriate curriculum, they set unambiguous expectations for the learner, and they serve as a reference for evaluation and feedback. An objective such as "teaches concepts of airway management" is not adequate because it defines what the teacher is doing and does not clearly describe what the learner should be demonstrating. Therefore, it neither serves as a road map for the teacher or the student nor does it identify a clear behavior the teacher can evaluate. Second, the teacher should describe the conditions under which the behaviors are to occur. For example "given a scenario using human simulation, the student will evaluate the airway and demonstrate effective bag-mask ventilation. This is called scaffolding and is based on a classical hierarchy of levels of comprehension described by Bloom. The teacher can ask some simple questions to better understand what level of cognitive domain the student is at, as well as how or why the student is at that point in order to progress to the next level. Using an example from the treatment of heart failure, a teacher could start with a comprehension-level question such as "What is the mechanism of action of furosemide For them to value a specific goal, they need to understand why it is necessary to incorporate the material into their clinical practice. For example, the instructor should explain why certain educational goals have been chosen, why they are important, and the consequences of failing to incorporate them. Safe and respectful learning environment Learning Objectives for Fourth-Year Critical Care Medicine Course others or demonstrating negative body language, for example. These concepts are consistent with the pillars and principles of adult learning listed in Table 186-1.
This finding is not always present in cardiac tamponade diabetes in dogs information glycomet 500 mg buy otc, because the amount of fluid in the pericardial space may be small but still cause a tamponade physiology, depending on the acuity with which the effusion accumulates and the compliance of the pericardium. Doppler findings of cardiac tamponade are based on characteristic changes in intrathoracic and intracardiac hemodynamics that occur with respiration. Because of the principle of ventricular interaction, mitral inflow velocity (E wave) decreases after inspiration and increases after expiration. With tamponade, the exaggerated inspiratoryexpiratory variation of the inflow velocity (E wave) over one respiratory cycle should be greater than 40% on the left and greater than 80% on the right. A significant pleural effusion sometimes causes significant respiratory Doppler variations of the inflow velocities that disappear when the effusion is drained. In some circumstances, echocardiographic signs of tamponade may be subtle or absent, so one must keep in mind that the diagnosis of tamponade remains a clinical one and that the echocardiographic signs must be analyzed in conjunction with the clinical findings. Complications After Cardiac Surgery Bedside echocardiography has proved to be of particular value in the critical care management of patients with hemodynamic instability after cardiothoracic operations. The most frequent echocardiographic diagnoses encountered in these patients are left ventricular or right ventricular failure, tamponade, hypovolemia, and valvular dysfunction. This postcardiotomy patient was in profound shock and was brought back to the operating room emergently for reexploration and drainage of the effusion. Left ventricular failure was found in 27% of patients, hypovolemia in 23%, right ventricular failure in 18%, biventricular failure in 13%, and tamponade in 10%. Comparison with hemodynamic parameters showed agreement on diagnosis (hypovolemia versus tamponade versus cardiac failure) in only 50% of the cases. Echocardiography identified two cases of tamponade and six of hypovolemia that were not suspected based on standard hemodynamic data. Descriptions of the echocardiographic findings of left ventricular dysfunction, tamponade, hypovolemia, and valvular dysfunction were described earlier in this chapter. Infective endocarditis was the second most common indication for performance of an echocardiogram among centers reporting their experience, as summarized in a review article by Heidenreich. Classic clinical findings suggesting endocarditis106 are uncommon in this patient population. Echocardiography is the test of choice for the noninvasive diagnosis of endocarditis. Absence of clinical stig- mata is especially likely if the infection presents acutely. Because the consequences of untreated endocarditis are devastating and often ultimately fatal, it is important that the infection and its complications be recognized promptly and treated appropriately. All positive studies were in patients who had an increased likelihood for infective endocarditis before the examination, as indicated by the presence of fever, positive blood cultures, new-onset murmur, prosthetic valve, or new-onset heart failure (alone or in combination). Clinical risk factors considered high risk included intracardiac prosthetic material, positive blood cultures (in particular, S. The aorta may have to be imaged to rule out dissection, rupture, aneurysm, aortic debris, or aortic abscess. As described earlier, there exists a blind spot in the distal portion of the ascending aorta and the proximal portion of the transverse aorta where imaging can be suboptimal. Exclusion of major trauma to the ascending and descending aorta at the bedside is important in this context. Assessment for Intracardiac and Intrapulmonary Shunts In critically ill patients, clinical suspicion for an intracardiac or intrapulmonary shunt most often is raised in the context of unexplained embolic stroke or refractory hypoxemia. Theinitialelectrocardiogram was unremarkable, and the chest x-ray showed a widened mediastinum. The patient underwent transesophageal echocardiography, which revealed the presence of a large dissecting aneurysm of the descending thoracic aorta. The short-axis view (A) revealed the presence of a large aneurysm withatrueandafalselumen. Common origins of right-to-left shunt are atrial septal defect or patent foramen ovale at the cardiac level5 and arteriovenous fistula at the pulmonary level. Color-flow imaging increases the detection rate of intracardiac shunt to some extent, but usually only when the shunt is large. After injection, the contrast is seen in the vena cava, right atrium, right ventricle, and pulmonary artery. In the absence of a shunt, only a minimal amount of contrast should be seen in the left-sided cavities, because most of the microbubbles from the agitated saline are unable to pass through the pulmonary capillaries. Performance of a Valsalva maneuver by the patient during contrast injection increases the sensitivity of the bubble study to detect right-to-left shunting. In mechanically ventilated patients, a maneuver equivalent to a Valsalva may be performed by inducing sudden release of sustained airway pressure previously achieved by inflating the lungs manually. This maneuver reverses the atrial transseptal gradient and may help uncover a patent foramen ovale that would not have been seen otherwise. Right-to-left shunting also can be caused by the presence of pulmonary arteriovenous fistulas. These often are associated with end-stage liver disease (hepatopulmonary syndrome). The characteristic of intrapulmonary versus intracardiac shunt is that there is a longer delay (three to five cardiac cycles) between the appearance of contrast from the right-sided to left-sided cavities in the presence of an intrapulmonary shunt. After myocardial infarction, patients can develop cardiogenic shock due to acute development of a ventricular septal defect and resultant left-to-right shunt. Physical examination and invasive hemodynamic monitoring (pulmonary artery catheterization) sometimes can miss this diagnosis.
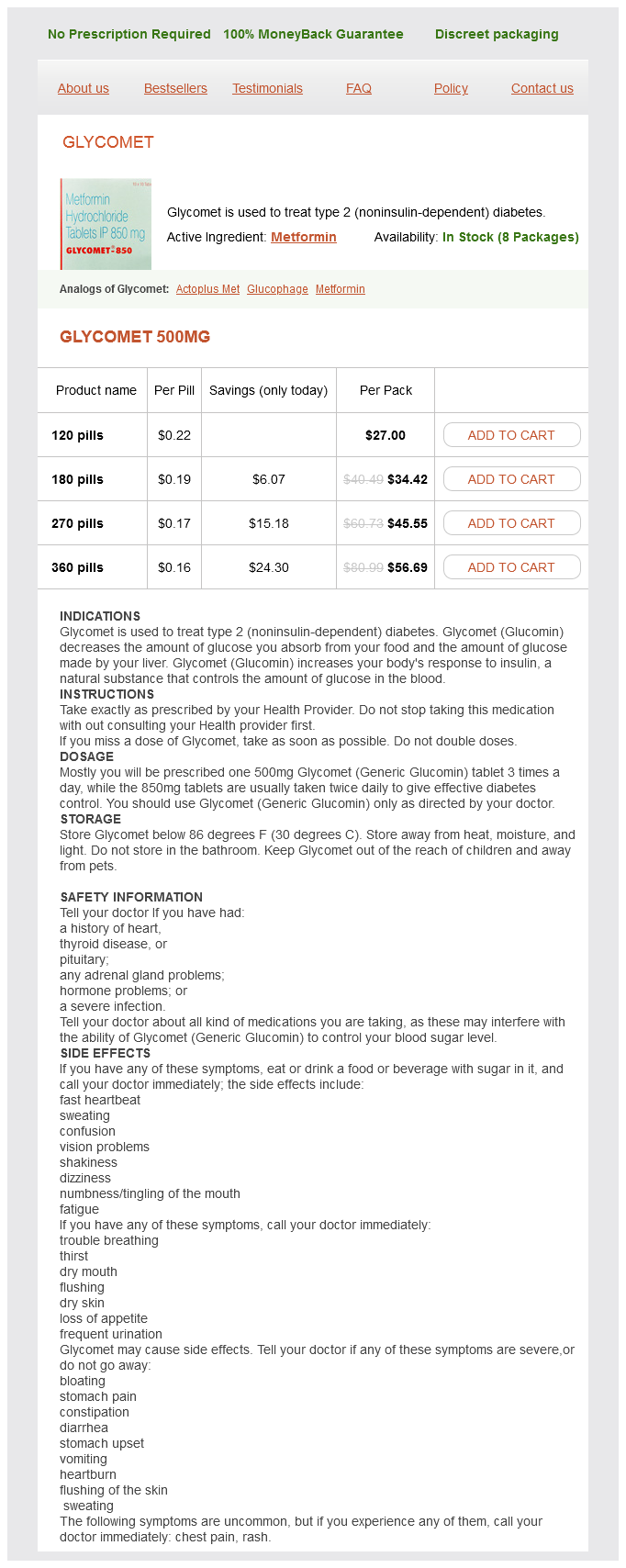
Glycomet Dosage and Price
Glycomet 500mg
- 120 pills - $27.00
- 180 pills - $34.42
- 270 pills - $45.55
- 360 pills - $56.69
It is almost always unilateral and can be characterized as aching or cramping rather than shock-like neuritic pain typical of trigeminal neuralgia diabetes glucose levels chart glycomet 500 mg purchase without a prescription. The distribution of pain is in the distribution of the trigeminal nerve but invariably overlaps divisions of the nerve. Headache often accompanies the pain of atypical facial pain and is clinically indistinguishable from that of tension-type headache. Stress is often the precipitating or exacerbating factor in the development of atypical facial pain. Depression and sleep disturbance are also manifest in a significant number of patients suffering from atypical facial pain. A history of facial trauma, infection, or tumor of the head and neck may be elicited in some patients with atypical facial pain, but in most cases, no precipitating event can be identified. The pain of trigeminal neuralgia is always within the distribution of a division of the trigeminal nerve, whereas the pain of atypical facial pain will invariably overlap these divisional boundaries. The trigger areas that are characteristic of trigeminal neuralgia are absent in patients suffering from atypical facial pain. Signs and Symptoms Table 134-1 compares atypical facial pain with trigeminal neuralgia. Chapter 135 Occipital Neuralgia 219 Testing Radiographs of the head are usually within normal limits in patients suffering from atypical facial pain but may be useful to help identify tumor or bony abnormality. Complete blood count, erythrocyte sedimentation rate, and antinuclear antibody testing are indicated if inflammatory arthritis or temporal arteritis is suspected. The pain of atypical facial pain is dull and aching in character, whereas the pain of reflex sympathetic dystrophy of the face is burning in nature, with significant allodynia often present. Stellate ganglion block may help distinguish the two pain syndromes, because the pain of reflex sympathetic dystrophy of the face readily responds to this sympathetic nerve block and atypical facial pain does not. The pain of atypical facial pain must be distinguished from the pain of jaw claudication associated with temporal arteritis. Treatment the mainstay of atypical facial pain is the combination of pharmacologic treatment with tricyclic antidepressants and physical modalities such as oral orthotic devices and physical therapy. Trigeminal nerve block and intraarticular injection of the temporomandibular joint with small amounts of local anesthetic and steroid may also be of value. Orthotic devices help the patient avoid jaw clenching and bruxism, which may exacerbate the clinical syndrome. Treatment of underlying depression and anxiety is mandatory if the clinician hopes to help relieve the symptoms of atypical facial pain. Differential Diagnosis the clinical symptomatology of atypical facial pain may often be confused with pain of dental or sinus origin or may be erroneously characterized as trigeminal neuralgia. Tumors of the zygoma and mandible, as well as posterior fossa tumors and retropharyngeal tumors, may produce ill-defined pain that may be attributed to atypical facial pain, and these potentially life-threatening diseases must be carefully searched for in any patient with facial pain. The pain of occipital neuralgia is characterized as persistent pain at the base of the skull with occasional sudden shocklike paresthesias in the distribution of the greater and lesser occipital nerves. Tension-type headache, which is much more common than occipital neuralgia, will occasionally mimic the pain of occipital neuralgia. The patient suffering from occipital neuralgia will experience neuritic pain in the distribution of the greater and lesser occipital nerves when the nerves are palpated at the level of the nuchal ridge. Some patients can elicit pain with rotation or lateral bending of the cervical spine. Testing is aimed primarily at identifying occult pathology or other diseases that may mimic occipital neuralgia (see Differential Diagnosis). Screening laboratory testing consisting of complete blood count, erythrocyte sedimentation rate, and automated blood chemistry testing should be performed if the diagnosis of occipital neuralgia is in question. Signs and Symptoms the greater occipital nerve arises from fibers of the dorsal primary ramus of the second cervical nerve and, to a lesser extent, from fibers from the third cervical nerve. The lesser occipital nerve passes superiorly 220 Section 3 Painful Conditions Sensory distribution of greater occipital nerve Sensory distribution of lesser occipital nerve Neural blockade of the greater and lesser occipital nerves can serve as a diagnostic maneuver to help confirm the diagnosis and to distinguish it from tension-type headache. Differential Diagnosis Occipital neuralgia is an infrequent cause of headaches and rarely occurs in the absence of trauma to the greater and lesser occipital nerves. More often, the patient with headaches involving the occipital region is in fact suffering from tension-type headaches. Tension-type headaches will not respond to occipital nerve blocks but are very amenable to treatment with antidepressant compounds such as amitriptyline in conjunction with cervical steroid epidural nerve blocks. Therefore, the clinician should reconsider the diagnosis of occipital neuralgia in those patients whose symptoms are consistent with occipital neuralgia but who fail to respond to greater and lesser occipital nerve blocks. Treatment the treatment of occipital neuralgia consists primarily of neural blockade with local anesthetic and steroid combined with the judicious use of nonsteroidal anti-inflammatory drugs, muscle relaxants, tricyclic antidepressants, and physical therapy. Neural blockade of the greater and lesser occipital nerves is a straightforward technique and is a reasonable early treatment of occipital neuralgia. In addition to the pain, the patient with cervical radiculopathy may experience associated numbness, weakness, and loss of reflexes. The causes of cervical radiculopathy include herniated disk, foraminal stenosis, tumor, osteophyte formation, and, rarely, infection. Occasionally, a patient suffering from cervical radiculopathy will experience compression of the cervical spinal cord resulting in myelopathy. Cervical myelopathy is most commonly due to midline herniated cervical disk, spinal stenosis, tumor, or, rarely, infection.