Grifulvin V
General Information about Grifulvin V
Grifulvin V is primarily used for the therapy of fungal infections of the skin, hair, and nails. It is usually prescribed for situations like athlete's foot, jock itch, and ringworm. These infections are caused by a sort of fungi generally identified as dermatophytes. Grifulvin V can additionally be used for treating infections caused by fungi that have an effect on the scalp, hair follicles, and nails.
One of the significant benefits of using Grifulvin V is its effectiveness in opposition to a variety of fungal infections. It is also a cheap choice in comparability with other antifungal medications, making it accessible to a larger population. The treatment is available in the type of tablets, making it simple to take and handle. Furthermore, the outcomes of using Grifulvin V are often seen within a quantity of weeks, making it a fast-acting and environment friendly treatment possibility.
Precautions to be taken while utilizing Grifulvin V
Grifulvin V works by binding to the fungal cells and preventing them from multiplying and spreading. It blocks the cells from producing new cell partitions, which are necessary for their growth and survival. With the absence of new cell partitions, the fungus is unable to survive and unfold, finally resulting in its demise. This mechanism of action makes Grifulvin V a extremely effective treatment for treating fungal infections.
Grifulvin V is a drugs that accommodates the lively ingredient griseofulvin. It is an antifungal drug that works by stopping the expansion of fungus within the body. The treatment is available in the type of tablets and is prescribed by medical doctors for the therapy of varied fungal infections. Let's take a closer take a look at what Grifulvin V is and how it might help in treating fungal infections.
Fungal infections are a common drawback that impacts tens of millions of people yearly. They can occur on various parts of the body, together with the scalp, feet, nails, and even within the hair follicles. These infections could be uncomfortable, itchy, and even painful if left untreated. One of the simplest treatments for these fungal infections is Grifulvin V.
While Grifulvin V is a secure and effective medicine, it is important to take precautions to keep away from any potential side effects. The medicine is in all probability not suitable for folks with sure medical circumstances, corresponding to liver illness or lupus. It is also not beneficial for pregnant or breastfeeding girls. Additionally, Grifulvin V might interact with certain medicines, so it's essential to tell your physician about any other drugs you take.
How does Grifulvin V work?
Benefits of utilizing Grifulvin V
In conclusion, Grifulvin V is a extremely efficient medicine for treating fungal infections of the scalp, physique, foot, nails, and hair follicles. With its mechanism of action, it successfully stops the growth and unfold of the fungus in the body, offering reduction from the uncomfortable signs of those infections. However, it's always really helpful to consult a physician before beginning any medicine and to follow their directions for secure and effective therapy.
Grifulvin V is a prescription medication that belongs to a category of medicine generally known as antifungals. It is an oral antifungal medicine that's used to deal with fungal infections of the scalp, body, foot (athlete's foot), nails, thighs (jock itch), or hair follicles (barber's itch). The active ingredient, griseofulvin, works by stopping the growth of fungus in the physique, thereby treating the an infection.
What is Grifulvin V?
What are the makes use of of Grifulvin V?
It is an abnormal proliferation of fibroblasts that can produce tumors fungus gnats kitchen sink purchase grifulvin v 250 mg mastercard, or hard white sheets. Desmoid tumors can grow rapidly and be fatal, while even desmoid sheets can pucker adjacent organs, causing bowel or ureteric obstruction, and enterocutaneous fistulas. Overall, about 12% regress, 7% are lethal, and the remainder never disappear, but rather grow and shrink to a small extent while remaining relatively asymptomatic. The risk factors predicting the possibility of desmoid disease include sex (females twice as likely as males), family history of desmoids, extracolonic manifestations of Gardner syndrome (epidermoid cysts, osteomas, extra teeth), and genotype. While there is no predictably successful treatment for desmoid disease, a staging system can be used to triage patients for the various options (Table 165. Since complete eradication of desmoid disease is unlikely, the achievable therapy goal is to stabilize the disease and render the patient asymptomatic. For early-stage desmoid disease, sulindac is effective, but the response may take up to 2 years to be clinically evident. Methotrexate and vinorelbine is effective in about 30% of cases,50 while doxorubicin (Doxil) is perhaps even more effective. Abdominal wall desmoids can be resected with success, often requiring abdominal wall repair with mesh. Intraabdominal desmoids are less often resectable because of their predilection to occur in the retroperitoneum and the small bowel mesentery. However, desmoids in the distal mesentery away from the root vessels are often resectable, but have a local recurrence rate ranging from 50% to 80%. Although desmoid tumors may be sensitive to radiation, this is not an option for intraabdominal desmoids due to the proximity of the small bowel. Fifty percent of normal-appearing ampullas have epithelial dysplasia, although the significance of this is questionable. However, they can be numerous, and when proliferative can hide an underlying carcinoma. Low-grade dysplasia has been found in up to 40% of random biopsies and a low threshold for concern is appropriate. They are frequently located in the antrum and may develop as a result of bile reflux into the stomach. The severity of duodenal adenomatosis predicts the chances of duodenal cancer, and can be described using the Spigelman staging system that is based on adenoma number, size, and histology (Table 165. Duodenal adenomas can be treated by snare polypectomy or by transduodenal polypectomy. Ampullary adenomas can be treated by endoscopic mucosal resection or surgical ampullectomy. All of these lesser procedures have lower morbidity than duodenectomy but have much higher recurrence rates. The cluster of manifestations referred to as Gardner syndrome includes osteomas (usually in the head and face), epidermoid cysts, extra teeth, and desmoids. Cleveland Clinic has shown that thyroid cancers detected on screening are smaller than incident cancer and have a better outcome. They are rarely symptomatic and even more rarely functional, and can be observed as long as they are less than 5 cm in diameter. If found early, it is curable with surgery, making the case for screening infants to age 7 with ultrasound and -fetoprotein. With extreme 3 prime mutations there is a predilection for severe desmoid disease, and sometimes there are no colorectal adenomas at all (hereditary desmoid disease). Desmoid disease is common in those with 3 prime mutations but can also happen with 5 prime mutations. Patients with very mild colorectal polyposis may be treated with colonoscopy every year rather than colectomy. Since these diseases are recessively inherited, a mutated copy from each parent must be passed on for the offspring to develop the syndrome. If one parent has the disease and the other parent is a carrier, the odds of the children developing the disease are 1 in 2. The polyps may develop early or late, and can include adenomas and serrated polyps. There are reports of gastric and duodenal adenomas, small bowel carcinomas, desmoid tumors, and thyroid cancer. Management depends on the severity of colorectal polyposis and the age of the patient at presentation. If the colorectal neoplasia is controllable by colonoscopy, this is a reasonable option, especially when expert colonoscopy is available and the patient is compliant. The exam is repeated at an interval appropriate for the polyp number, size, and degree of dysplasia, but no longer than 1 to 2 years. Failure of these proofreading domains can lead to a dominantly inherited syndrome of colorectal and endometrial cancer predisposition. There are few families reported with this syndrome, so the full picture of the phenotype is lacking. Patients must be treated according to their presentation, although in those already diagnosed who present with a cancer, extended surgery seems reasonable. Knowledge of these syndromes allows the appropriate genetic counseling and testing, the assessment of cancer risk, and the screening recommendations. They are bright red, usually pedunculated, and histologically are hamartomas that feature an inflammatory infiltrate with large mucus-filled spaces distributed in an expanded lamina propria and a prominent inflammatory infiltrate. In sporadic cases, the condition may represent a new mutation or incomplete penetrance of the gene, but it also may result from environmental factors. Polyp growth begins in the first decade of life and there are variable numbers, usually between 50 and 200.
Digestive System Table 39: Summary of distinguishing digesting tract features fungus key purchase genuine grifulvin v line, by region and layers Muscularis (Inner Circular Mucosa (Epithelium, and Outer Longitudinal Region and Lamina Propria, Submucosa (with Layers, with Myenteric subdivisions Muscularis Mucosae) Submucosal Plexuses) Plexuses between Them) Esophagus (upper, middle, Nonkeratinized stratified Small esophageal glands Both layers striated muscle lower) squamous epithelium; (mainly mucous) in upper region; both layers cardiac glands at lower smooth muscle in lower end region; smooth and striated muscle fascicles mingled in middle region No distinguishing features Three indistint layers of Stomach (cardia, fundus, Surface mucous cells body, pylorus) and gastric pits leading smooth muscle (inner oblique, middle circular, and to gastric glands with parietal and chief cells, (in outer longitudinal the fundus and body) or to mucous cardiac glands and pyloric glands Small intestine Plicae circulares; villi, with Duodenal (Brunner) glands No distinguishing features (duodenum, jejunum, enterocytes and goblet (entirely mucous); possible ileum) cells, and crypts/glands extensions of Peyer patches in ileum with Paneth cells and stem cells; Peyer patches in ileum Adventitia/Serosa Adventitia, except at lower end with serosa Serosa Mainly serosa 201 Self Assessment and Review of Anatomy Muscularis (Inner Circular and Outer Longitudinal Submucosa (with Layers, with Myenteric Submucosal Plexuses) Plexuses between Them) Adventitia/Serosa No distinguishing Outer longitudinal layer Mainly serosa, with features separated into three bands, adventitia at rectum the teniae coli Venous sinuses Inner circular layer thickened as internal sphincter Adventitia Region and subdivisions Large intestine (cecum, colon, rectum) Anal canal Mucosa (Epithelium, Lamina Propria, Muscularis Mucosae) Intestinal glands with goblet cells and absorptive cells Stratified squamous epithelium; longitudinal anal columns Gut tube has 4 layers: Mucosa, Submucosa, Muscularis externa and Adventitia/Serosa. Its contraction moves the mucosa Submucosa consists of mainly dense irregular connective tissue. Adventitia is chiefly made up of connective tissue, whereas, serosa has the serous membrane made up of squamous epithelium. Oral Cavity Table 40: Review of oral tissues Structure Details Oral mucosa Stratifies squamous epithelium with variable site-dependent keratinization Teeth Enamel: surface layer of closely packed calcium hydroxyapatite crystals formed by an extemal ameloblast layer; destroyed with tooth eruption Dentine: deeper zone of calcified tissue containing numerous fine parallel tubules radiating from odontoblasts which line the pulp cavity and form dentine Pulp: central core of loose tissue with nerves and vessels supplying odontoblasts Tongue Muscular organ with layers of skeletal muscle fibers oriented perpendicular to each other; numerous minor salivary glands and surface stratified squamous eprthelium with filiform, fungiform and circumvallate papillae Taste buds Sensory organs of taste situated in tongue mucosa Salivary glands Serous and/or mucinous glands; found as large glands (parotid, submandibular and sublingual) and innumerable small (minor) glands Tonsils and lingual tonsils Lymphoid organs near posterior tongue and extension of similar structures onto posterior tongue 202 Histology Oral cavity has non-keratinized stratified squamous epithelium. Para-keratinization: persistence of the nuclei of the keratinocytes into the stratum corneum; this is normal only in the epithelium of true mucous membranes of the mouth and vagina. The mucosa consists of a relatively thick stratified squamous epithelium, a thin layer of lamina propria containing occasional lymphatic nodules, and muscularis mucosae. Mucous glands are present in the submucosa, their ducts, which empty into the lumen of the esophagus, are not evident in this section. External to the submucosa in this part of the esophagus is a thick muscularis externa made up of an inner layer of circularly arranged smooth muscle and an outer layer of longitudinally arranged smooth muscle. Gastric intrinsic factor is essential for absorption of vitamin B12 (and erythropoiesis). In pernicious anemia, autoantibodies destroy the parietal cells leading to deficiency of intrinsic factor and resultant Vit. Chief cells are small, basophilic columnar cells, more numerous in the lower half of the gland-more so at the base (fundus) of the gastric gland. Neuroendocrine cells are small cells, found at the deeper areas-base (fundus) of the gastric gland, along with chief cells. The secretory activities of the chief and parietal cells are controlled by the autonomic nervous system and the hormone gastrin, secreted by the enteroendocrine cells of the pyloric region of the stomach. Submucosa · the submucosa consists of a layer of fibroelastic connective tissue containing blood vessels and nerves. It is the strongest component of the esophagus and intestinal wall and therefore should be included in anastomotic sutures. In the upper third of the oesophagus, the muscularis externa is formed by skeletal muscle; in the middle third, smooth muscle fascicles intermingle with striated muscle; and this increases distally such that the lower third contains only smooth muscle. They are mainly located in the apical half of the body of gland, reaching as far as the neck. Surface mucus cells are distributed in the gastric pit region of the gastric mucosa. Neuroendocrine cells are situated mainly in the deeper/basal parts of the glands, along with the chief cells. Enterocyte (Absorption) Goblet cell (Mucus) Paneth cell (Maintain intestinal flora/Cytokines) Enteroendocrine cell (Hormones) M (micro-fold) cell (Immunity) Stem cell 206 6. In the anal canal, the simple columnar epithelium undergoes transition into a stratified columnar (or cuboidal) epithelium and then to a stratified squamous epithelium. This transition occurs in the area referred to as the anal transitional zone, which occupies the middle third of the anal canal between the colorectal zone and the squamous zone of the perianal skin. Paneth cell · Most of the cells in the mucosa of small intestine are derived from the stem cells located in the basal region of the crypts and this progeny migrate out along the wall of the crypts towards the villi (Paneth cell being an exception migrate towards the base). The apical region has large number of lysozymes, which takes eosin, making the paneth cell appear dark pink at the apex. Neck cells · At least six types of cells are found in intestinal mucosal epithelium: 1. M cells (microfold cells), modified enterocytes that cover enlarged lymphatic nodules in the lamina propria. Base of intestinal crypts · Stem cells are located near the base (lower half) of crypts of Lieberkuhn, in the intestine. Liver and Pancreas Table 43: Review of liver and pancreas Structure Key components and features Liver Solid organ composed of plates of hepatocytes with network of portal tracts Hepatocytes Large eosinophilic cells with central nuclei and prominent nucleoli Cells arranged in plates one cell thick with intervening sinusoids Diverse metabolic functions Secretion of bile into canaliculi Portal tracts · · · · · Branches of: Bile duct Portal Vein Hepatic artery · Surrounded by limiting plate of hepatocytes · Dual vascular supply Portal vein (products of digestion but deoxygenated blood) Hepatic artery (Oxygenated blood from systemic circulation) · Drainage via hepatic vein back to systemic circulation · Classical liver lobule is hexagonal with central venule and peripheral portal tracts. Note that the hexagonal-shaped classic lobule (red) has the terminal hepatic venule (central vein) at the center of the lobule and the portal canals containing portal triads at the peripheral angles of the lobule. The triangular portal lobule (green) has a portal canal at the center of the lobule and terminal hepatic venules (central veins) at the peripheral angles of the lobule. A diamond-shaped liver acinus (multicolor) has distributing vessels at the equator and terminal hepatic venules (central veins) at each pole. It consists of adjacent sectors of neighbouring hexagonal fields of classic lobules partially separated by distributing blood vessels. The zones, marked 1, 2, and 3, are supplied with blood that is richest and most nutrient-oxygenated in zone 1 and least so in zone 3. The terminal hepatic venules (central veins) in this interpretation are at the pointed edges of the acinus instead of in the center, as in the classic lobule. The portal triads (terminal branches of the portal vein and hepatic artery) and the smallest bile ducts are shown at the corners of the hexagon that outlines the cross-sectioned profile of the classic lobule. It includes the the liver acinus/hepatic acinus is a diamond-shaped unit/area of liver parenchyma. It includes portions of two classical liver lobules with portal triad at each side of elliptical area and central vein on each end. Kupffer Cells Kupffer cells are hepatic macrophages derived from circulating blood monocytes and originate in the bone marrow. They are long-term hepatic residents and lie within the sinusoidal lumen attached to the endothelial surface. Stellate cells of von Kupffer are seen in the sinusoids of which of the following organs: a.
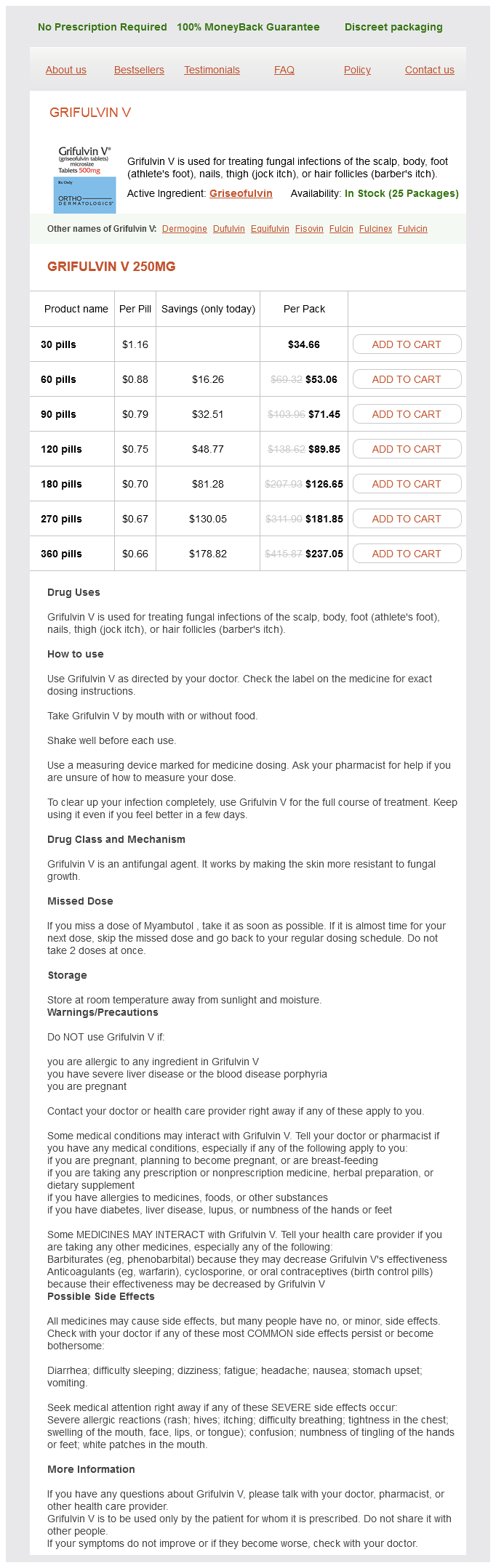
Grifulvin V Dosage and Price
Grifulvin V 250mg
- 30 pills - $34.66
- 60 pills - $53.06
- 90 pills - $71.45
- 120 pills - $89.85
- 180 pills - $126.65
- 270 pills - $181.85
- 360 pills - $237.05
Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer antifungal treatment for dogs order grifulvin v 125 mg on-line. Microsatellite instability in colorectal cancer: from molecular oncogenic mechanisms to clinical implications. Association between glutathione S-transferase P1, T1, and M1 genetic polymorphism and survival of patients with metastatic colorectal cancer. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in the Netherlands. A national strategic change in treatment policy for rectal cancer-implementation of total mesorectal excision as routine treatment in Norway. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. The effect of multidisciplinary teams for rectal cancer on delivery of care and patient outcome: has the use of multidisciplinary teams for rectal cancer affected the utilization of available resources, proportion of patients meeting the standard of care, and does this translate into changes in patient outcome Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. Late side effects of short-course preoperative radiotherapy combined with total mesorectal excision for rectal cancer: increased bowel dysfunction in irradiated patients-a Dutch colorectal cancer group study. Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01. Chemoradiotherapy with capecitabine versus fluorouracil for locally advanced rectal cancer: a randomised, multicentre, non-inferiority, phase 3 trial. Neoadjuvant capecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic resonance imaging-defined poor-risk rectal cancer. The contribution of targeted therapy to the neoadjuvant chemoradiation of rectal cancer. Systematic review of candidate single-nucleotide polymorphisms as biomarkers for responsiveness to neoadjuvant chemoradiation for rectal cancer. Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. Neoadjuvant chemotherapy without routine use of radiation therapy for patients with locally advanced rectal cancer: a pilot trial. Neoadjuvant bevacizumab, oxaliplatin, 5-fluorouracil, and radiation for rectal cancer. The reported incidence of anastomotic leak following colorectal surgery has varied from 1% to 30%, largely based on the criteria for diagnosis and the length of follow-up; the highest leak rate is seen with anastomoses involving the distal rectum. This results in significantly increased hospital costs and resource use, decreased quality of life, and potentially worse oncologic outcomes. Both of these areas of inquiry have contributed to only a limited understanding of the actual mechanism by which leaks occur and how best to prevent them. The reported risk factors vary greatly from study to study, and it can be challenging to know which clinical features are simply associated with a greater tendency for a leak and which may serve as a surrogate for some other factor that is of pathogenic importance. For decades, studies have focused on the technical aspects of anastomotic creation, considering such issues as sutures versus staples versus compression, single- versus two-layer construction, inverted versus everted technique, and the merits of a wide variety of mechanical devices designed to strengthen or protect the anastomosis, usually finding minimal impact on the incidence of anastomotic leaks. This structural framework of understanding has not appreciably moved the needle in preventing this devastating complication; it seems clear that new paradigms are needed. In this light, the possible role of the microbiome and collagenolytic bacteria in causing anastomotic leaks is intriguing. There are a broad array of clinical scenarios that could reasonably be described as representing or caused by an overt or occult disruption/imperfection in the anastomotic site. In 2010 the International Study Group of Rectal Cancer proposed a uniform definition of anastomotic leak as a defect at the anastomotic site leading to a communication between the intraluminal and extraluminal compartments. This communication can be confirmed radiographically, endoscopically, or intraoperatively. A pelvic abscess in close proximity to the anastomosis is also considered an anastomotic leak. The group also defined the severity of anastomotic leaks based upon the clinical management required. Prevention of anastomotic leaks will require improved understanding of the actual mechanisms by which they occur. Early detection, perhaps by more aggressive use of endoscopy or biomarkers of inflammation, may diminish the deleterious effects of a leak and allow for greater use of nonsurgical treatments. Reduction in the frequency and severity of complications due to anastomotic leak may eventually allow surgeons to move away from the current liberal use of "temporary" diverting stomas, which are, in and of themselves, a source of substantial physical and psychological morbidity and expense. Dye Test A dye test can be performed by injecting a mixture of sterile water and blue dye or povdone-iodine (Betadine) through a large-bore catheter placed transanally, while clamping the proximal bowel. A volume of 180 to 240 mL is usually required to adequately distend the anastomosis. One study has shown that the dye test allowed for the easier detection and localization of leaks than air leak testing. Although intraoperative endoscopy provides a useful adjunct to air leak testing, there is currently no evidence that its use alone results in fewer anastomotic complications. Less obvious is the amount of blood flow that represents a critical threshold for adequate healing to occur.