Indinavir
General Information about Indinavir
Apart from its antiviral properties, Indinavir has also been shown to extend the variety of CD4+ T cells in the physique, that are a type of white blood cell that performs an important function within the immune system. This helps to strengthen the body's capability to struggle off infections and illness.
Indinavir, also referred to as Crixivan, is a medication used to manage HIV/AIDS. It is classified as an HIV protease inhibitor, a kind of drug that works by blocking the perform of an enzyme known as protease, which is answerable for the manufacturing of new virus particles. This leads to a lower in the quantity of virus in the physique, slowing the development of HIV and improving the immune system.
Another limitation of Indinavir is its need for strict adherence to dosing schedules and dietary restrictions. For the medication to work successfully, it have to be taken precisely as prescribed and on an empty abdomen. This may be difficult for some patients and may lead to inconsistent treatment.
In conclusion, Indinavir has performed a significant function within the management of HIV since its approval over twenty years in the past. Its antiviral properties, along with its capability to increase CD4+ T cells, have proved to be efficient in slowing the progression of the virus and improving immune perform. While there are some drawbacks to this medicine, it stays an necessary component of HAART and continues to be a useful device within the battle towards HIV and AIDS.
One of the primary advantages of Indinavir is its capability to reduce the quantity of HIV in the body to undetectable levels. Studies have shown that when used as part of a HAART routine, Indinavir can lower the amount of virus within the blood to a level so low that it becomes undetectable. This is important because it not solely slows the progression of the illness but additionally reduces the risk of HIV transmission to others.
Indinavir is normally taken within the type of capsules, that are sometimes taken each 8 hours. It is important to take the treatment as prescribed and to not miss any doses, as this will result in drug resistance and make the therapy less effective. Adverse results of Indinavir can include nausea, diarrhea, headache, and fatigue, but these are usually manageable and diminish over time.
While Indinavir is an effective medicine in the treatment of HIV, it isn't with out drawbacks. One of the largest issues with this drug is its potential to cause kidney problems. Research has proven that long-term use of Indinavir can lead to the formation of kidney stones, and also can impression kidney function. It is subsequently important for patients taking Indinavir to have common kidney operate checks as a part of their HIV management.
With that being mentioned, Indinavir stays an necessary drug within the struggle in opposition to HIV and AIDS. Its capability to decrease viral load and increase CD4+ T cell count has been confirmed beneficial in bettering the health and high quality of life of these residing with the virus. However, it is essential to note that Indinavir isn't a treatment for HIV and will only be used as part of a comprehensive therapy plan.
Indinavir was first accredited by the United States Food and Drug Administration (FDA) in 1996 and has since been used in the therapy of HIV. It is often taken in combination with other medicines, as part of a extremely active antiretroviral therapy (HAART) regimen, to successfully handle the virus.
Coomassie brilliant blue) Different proteins bind differently; several different dyes in use; used in many laboratories for 24-hour excretion Measures albumin excretion not total protein medicine 0027 v discount indinavir 400 mg mastercard. Two to five per cent of children, 5% of young adults, and up to 16% of the elderly will show proteinuria on testing of a single sample. Impregnated with 100 mg/L indicator dye which changes colour in the presence of protein Confirm and quantitate Note whether haematuria is also present. Exclude infection by dipstick for nitrite, leucocytes, and by microscopy and culture. Exclude transient proteinuria There are several causes of transient proteinuria that usually do not convey the same connotations of renal disease and risk as sustained proteinuria: Postural proteinuria (see Chapter 51), the most common diagnosis in children and young people. The coexistence of haematuria greatly increases the probability of identifiable glomerular disease. Lower thresholds should be considered relevant in young patients because they face longer at risk. The presence of blood interferes with protein assays variably, but usually only at quite high levels of blood content. Microalbuminuria Microalbuminuria is presumed to be a consequence of derangement of function of the glomerular filtration barrier, although this has not been formally proven in all circumstances. This would explain the early appearance of microalbuminuria in glomerulopathies, as first demonstrated in diabetes (Mogensen and Christensen, 1984; Viberti, 1988) (see Chapter 149). However the origin of microalbuminuria in many patients with cardiovascular disease (see Chapters 97 and 98) has not been satisfactorily explained, and in theory it could alternatively be caused by reduced capacity of proximal tubules to reabsorb tubular proteins from filtrate. In young patients without comorbid conditions, microalbuminuria is likely to reflect early glomerular disease. Assess the degree of proteinuria Nephrotic range proteinuria Proteinuria at nephrotic levels (Table 50. Unless the cause is readily apparent, investigation including renal biopsy is usually indicated. For patients with nephrotic range proteinuria who fall short of nephrotic syndrome, many will require the same investigation and management. There may be exceptions when comorbidity makes it unlikely that disease-specific therapies could be tolerated. Assess other renal risk factors these include family history, drug history, hypertension, and low or (even more important) reducing estimated glomerular filtration rate. Conversely, elderly patients with comorbid conditions may be unlikely to have their management altered significantly by nephrological review at this level of proteinuria. If significant haematuria coexists with proteinuria, renal risk is substantially higher. The diseases causing proteinuria are increasingly likely to be recognizable glomerular conditions as the levels of proteinuria rise. Towards the lower end of this range diagnoses are less likely to alter management, except possibly in relatively young patients. Estimation of urinary light chains by immunofixation is the most widely used test, and though not as sensitive as assays for free Ig light chains it will certainly be positive if the explanation for proteinuria at this level. Assess and manage cardiovascular risk Patients with proteinuria are at significantly increased risk of cardiovascular disease and death (see Chapter 98). However, in the general population without an established renal diagnosis, cardiovascular endpoints are more likely than renal (discussed in Chapter 99). Proteinuria and progression of renal diseases the association between proteinuria and population outcomes was known before 1900. In the late 1970s, it was first appreciated how strongly the outcome of diverse renal diseases was dependent on proteinuria, and that this seemed even more important than the nature of the renal diagnosis. This experience was extended across other diseases including those in which proteinuria was not an initial feature such as reflux nephropathy (Kincaid-Smith and Becker, 1979), and during the 1980s it was found that the association of poor outcome with proteinuria seemed universal (Williams et al. Costbenefit analysis and prediction of 24-hour proteinuria from the spot urine proteincreatinine ratio. Protein and albumin-to-creatinine ratios in random urines accurately predict 24 h protein and albumin loss in patients with kidney disease. Chronic kidney disease and measurement of albuminuria or proteinuria: a position statement. Angiotensin-converting enzyme inhibitors, which happen to lower proteinuria, show additional renoprotection beyond that conveyed by blood pressure control. This was first shown in diabetes but later also in other diseases associated with proteinuria (see Chapter 98). It has not been proven whether this association with proteinuria is causative, or simply a useful epiphenomenon. Early research focused on possible direct toxicity of filtered proteins on cells of the nephron and the interstitium, but an equally viable hypothesis is that proteinuria is an indication of podocyte damage, and it is podocyte death that determines the outcome of scarred or stressed glomeruli. Attempts to lower proteinuria further by adding additional agents with proteinuria-lowering effects have had disappointing results so far, but there are other candidates to test (see Chapters 45 and 99). Differentiation of glomerular, tubular, and normal proteinuria: determinations of urinary excretion of beta-2-macroglobulin, albumin, and total protein. Fluorescent antibody identification of TammHorsfall protein in matrix and serum proteins in granules. Low molecular weight protein excretion in glomerular disease: a comparative analysis. Renal pathology and proteinuria determine progression in untreated mild/moderate renal failure.
Another option is based on treating relapses with daily prednisone medicine bottle 400 mg indinavir with mastercard, 4060 mg/m2, until proteinuria has disappeared for 45 days. Thereafter, prednisone is switched to alternate days and the dosage is tapered to 1520 mg/m2 every other day, according to the steroid threshold, that is, the dosage at which the relapse has occurred. The first approach allows better Levamisole the beneficial effect of levamisole was first described by Tanphaichitr et al. However, the beneficial effect of levamisole is not sustained after stopping treatment. Side effects occasionally include neutropenia, agranulocytosis, vomiting, cutaneous rash, neurological symptoms including insomnia, hyperactivity, and seizures. Alkylating agents Alkylating agents, such as cyclophosphamide and chlorambucil, have been used for > 50 years to achieve long-lasting remission. Unfortunately they are toxic, and in the long term, remissions may not seem long enough. The efficacy of alkylating agents is illustrated by a meta-analysis that compared alkylating agents with prednisone in maintaining remission. Therefore a prolonged treatment is necessary with an increased risk of nephrotoxicity (Niaudet and Habib, 1994; Hulton et al. Ciclosporin has been compared to alkylating agents in two randomized trials (Niaudet, 1992; Ponticelli et al. The effect of ciclosporin was initially the same as chlorambucil and cyclophosphamide in maintaining remission. However, after ciclosporin was discontinued, it was less effective in maintaining remission at 12 months compared with either alkylating agents and at 24 months for chlorambucil. Because of the concern for nephrotoxicity, the serum creatinine concentration should be monitored regularly in patients who are maintained on a long-term course of ciclosporin. However, serial renal biopsies demonstrate histologic lesions of nephrotoxicity without clinical evidence of renal function impairment (Habib and Niaudet, 1994; Iijima et al. Histological lesions most often consist of tubulointerstitial injury, characterized by stripes of interstitial fibrosis containing clusters of atrophic tubules and by lesions of arteriolopathy. Thus, some authors propose to routinely perform a kidney biopsy in asymptomatic patients after 18 months of ciclosporin therapy. Other side effects include hypertension, hyperkalaemia, hypertrichosis, gum hypertrophy, and hypomagnesaemia. The recommended starting ciclosporin dose is 150 mg/m2 per day divided into two oral doses. The dose should be adjusted to maintain trough whole blood levels between 100 and 200 ng/mL, and the level should not exceed 200 ng/mL. In order to limit the risk of nephrotoxicity, once remission is achieved, we recommend decreasing the dose to < 5 mg/kg, if possible. Low-dose alternate-day prednisone in combination with ciclosporin may be a good approach to maintain remission with lower doses of ciclosporin. Several studies involving patients with frequently relapsing or steroid-dependent nephrotic syndrome showed that cyclophosphamide resulted in sustained remission in 5793% of patients at 1 year, 3166% at 5 years, and 25% at 10 years (Cameron et al. However, a more recent series reported lower remission rates of 44%, 27%, and 13% at 1, 2, and 5 years after cyclophosphamide therapy (Cammas et al. In another study of 90 children with a steroid-dependent course, sustained remissions were observed in 31% of patients at 5-year follow-up (Azib et al. These variations are probably due to differences in the patient populations as steroid-dependent patients have a lower response rate than frequently relapsing patients. The Arbeitsgemeinschaft für pädiatrische Nephrologie (1987) reported that treatment for 12 weeks at a daily dose of 2 mg/kg was more effective than an 8-week course, with 67% as compared to 22% remaining in remission after 2 years. However, a randomized trial showed that prolonging the course of cyclophosphamide from 8 to 12 weeks did not further reduce the proportion of children experiencing relapses (Ueda et al. Cyclophosphamide toxicity includes bone marrow depression, haemorrhagic cystitis, gastrointestinal disturbances, alopecia, and infection (Latta et al. Leucopoenia is frequently observed, but weekly haematological monitoring may limit its severity and concomitant steroids help blunt marrow depression. Alopecia, which is variably pronounced, remits a few weeks after stopping treatment. Viral infections can be overwhelming if cyclophosphamide is not stopped in due time. Gonadal toxicity is well established and the risk of sterility is greater in boys than in girls. The cumulative threshold dose above which oligo/azoospermia may be feared lies between 150 and 250 mg/kg (Penso et al. In females, the cumulative dose associated with sterility is greater, but not well defined. In this and other contexts, early menopause may be a late consequence of alkylating agents. Most authors would prescribe a 12-week course of oral cyclophosphamide at a daily dose of 2 mg/kg. Beneficial results have also been achieved with chlorambucil in steroid-responsive nephrosis (Grupe et al. Acute and long-term toxic effects are similar to those observed with cyclophosphamide. Tacrolimus Though data is not so comprehensive, tacrolimus is probably as effective as ciclosporin in maintaining remission in children with steroid-sensitive nephrotic syndrome, Transplantation experience (see Chapter 281) suggests that it is less nephrotoxic but more likely to be associated with diabetes (Dotsch et al. In a series of five children treated with tacrolimus, two developed type 1 diabetes mellitus, which resolved after stopping tacrolimus therapy (Dittrich et al.
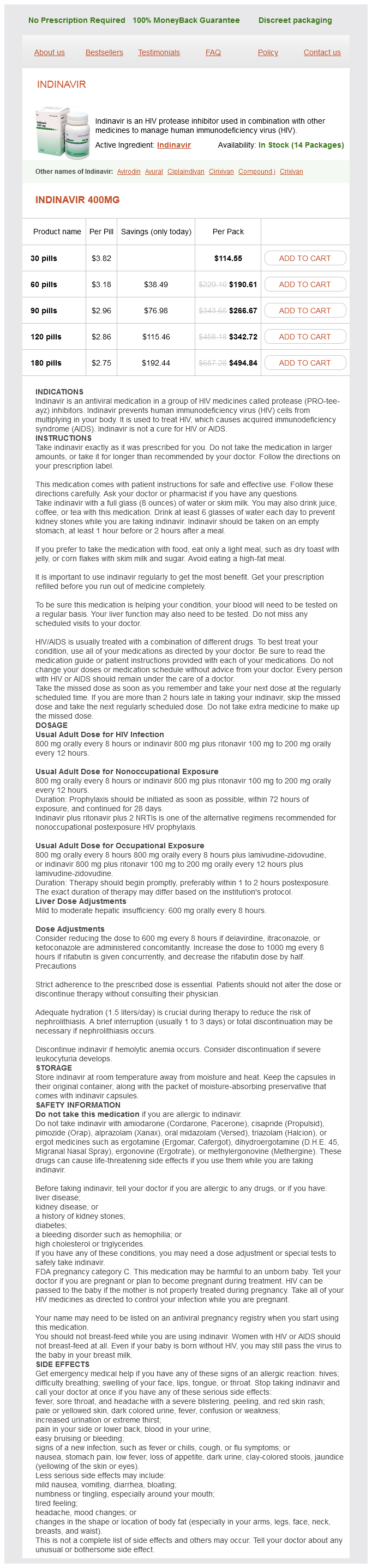
Indinavir Dosage and Price
Indinavir 400mg
- 30 pills - $114.55
- 60 pills - $190.61
- 90 pills - $266.67
- 120 pills - $342.72
- 180 pills - $494.84
Individuals with microscopic haematuria being worked up as potential kidney transplant donors should be biopsied since it is important to exclude a glomerulonephritis such as IgA nephropathy medicine wheel generic 400 mg indinavir otc. However, a biopsy may be helpful to assess the acuteness of the illness and the degree of chronic and irreversible damage. Transplant kidneys Some units routinely take biopsies during implantation either before and/or after reperfusion. This may be helpful in defining the presence or degree of existing disease in the donor kidney, particularly important in older donors. This policy may vary depending on the induction therapy (early rejection is unlikely with anti-T-cell-agent induction). Later in the post-transplant course the kidney is biopsied to investigate dysfunction or heavy proteinuria (see Chapters 286 and 289). The procedure Pre-biopsy evaluation Before renal biopsy, the patient should have a renal ultrasound to establish the presence of two normal-sized unobstructed kidneys. Biopsy of a small kidney is associated with higher risks of bleeding and is less likely to provide diagnostic information (small scarred kidneys often show sclerosed glomeruli and interstitial fibrosis with no features of the original disease). Biopsy of a kidney with a cortical thickness of < 1 cm has a higher risk of complications and a lower chance of obtaining diagnostically useful tissue. Anatomic abnormalities, for example, ectopic kidneys, crossed fused ectopia, and horseshoe kidneys, increase the risk of bleeding. Any of these factors need to be taken into account when estimating the balance of risk over benefit for the individual patient. The patient should be tested for any bleeding tendency and have normal clotting tests, a platelet count 100,000 and not be severely anaemic (haemoglobin < 9 g/dL). Although there have been reports that it is predictive of complication (Stratta et al. Although not evidence based, many recommend this for patients with poor renal function. Patients with diabetic nephropathy usually have evidence of retinopathy and/or neuropathy and when these are present, a biopsy is not usually indicated. In the absence of these complications or with rapid-onset nephrotic syndrome, a short duration of (diagnosed) diabetes and possibly with significant haematuria or systemic disease, a biopsy is indicated to determine if another treatable condition is present. Even when another cause for renal disease is found there is often evidence of diabetic nephropathy as well (Pham et al. It is difficult to argue benefit in patients with relatively low-level proteinuria (< 1. Management of such patients with good blood pressure control and maximizing angiotensin-converting enzyme inhibitor/angiotensin receptor blocker therapy would be the same unless nephrotic syndrome and/or renal impairment were to develop. The threshold for biopsy is lowered as the proteinuria increases but the arguments are essentially the same. These would include the following: Mild to moderate back/loin pain which usually settles with simple analgesia such as paracetamol Visible haematuria (up to 5%) which usually clears spontaneously within 24 hours Local bleeding always occurs but is usually minor and self-limiting; more severe bleeding requiring transfusion (~ 1%) Bleeding requiring angiographic intervention (0. Biopsies are generally performed under direct ultrasound control using a disposable Tru-Cut needle or biopsy gun. Biopsy under direct vision has a higher success and lower complication rate than using ultrasound merely for localization. Choice of needle gauge (G) is a matter of personal preference; it is customary to use a 16-G needle for native and 18-G for transplant biopsies. These generally provide adequate sample size with a trend to lower bleeding rates in these single kidneys which may require multiple biopsies. Either kidney may be biopsied, but the left kidney is usually more convenient as it is usually lower so access to the pole is easier. The patient lies prone on one or two firm pillows and the operator first determines the optimum entry site with ultrasound and in which phase of respiration the biopsy will best be performed, aiming for the lower pole through the cortex. The skin is sterilized, sterile gel applied, and the probe covered with a sterile sheath. Local anaesthetic is administered and then, using a spinal (21-G) needle, more local anaesthetic is delivered down to the capsule of the kidney. The biopsy needle is then advanced to the renal capsule under ultrasound visualization, the patient stops breathing as the device is fired and immediately removed, after which the patient can breathe normally. Patients unable to lie prone may be biopsied in the sitting position as for a pleural drain. Transplant biopsies are usually more straightforward because the kidney is superficial and does not move with respiration. However, transplant kidneys sometimes lie in unusual orientations and more care needs to be taken to avoid bowel (especially with intraperitoneal kidneys). It is also useful to use colour Doppler to identify large blood vessels, such as the iliac artery and vein, which may lie very close to the lower pole. Patients are kept on bed rest for 4 hours with pulse and blood pressure monitoring and the urine tested for the presence of blood. Patients are discharged home approximately 6 hours after the procedure provided there are no signs of bleeding and the patient will not be alone for the first night. Patients with macroscopic haematuria are kept under observation until this settles (and usually overnight). Other techniques have been described including open surgical and laparoscopic biopsy and, in patients with uncorrectable clotting abnormalities, biopsy is performed via the internal jugular vein but bleeding complications can still occur and the samples are small and often difficult to interpret. Biopsy of patients on aspirin and clopidogrel should be avoided but if absolutely essential then platelet transfusion will reduce the risk of bleeding. Anticoagulants should be reversed or stopped before biopsy and the decision to change to heparin needs to be considered on an individual patient basis. Unfractionated heparin should be stopped at least 6 hours and low-molecular-weight heparin 24 hours before biopsy. Correction of clotting abnormalities with fresh frozen plasma or clotting factors may be necessary for an urgent biopsy.