Isoptin
General Information about Isoptin
In addition to controlling high blood pressure, Isoptin can also be used for treating various heart circumstances similar to angina, arrhythmias, and heart failure. It may additionally be used to stop or reduce recurring chest ache and improve blood flow to the heart.
The medication is out there in each immediate-release and extended-release formulations, and is usually taken orally a couple of times a day. It is necessary to take it precisely as prescribed by the doctor for maximum effectiveness.
Isoptin helps in treating high blood pressure by blocking the entry of calcium into the smooth muscle tissue of the blood vessels, causing them to relax and dilate. This ends in a decrease blood pressure and decreased workload on the guts.
Certain precautions should be taken when utilizing Isoptin. It just isn't really helpful for people with a identified allergy to verapamil or those that have a history of heart failure, liver or kidney illness, or low blood stress. It also needs to be used with caution in pregnant or breastfeeding ladies.
Moreover, Isoptin shouldn't be taken with sure drugs similar to beta-blockers, amiodarone, and sure antibiotics. It is necessary to tell your physician about all the medications you're taking to avoid potential drug interactions.
In conclusion, Isoptin is an effective medicine for controlling high blood pressure. It works by enjoyable the blood vessels, resulting in a lower blood pressure. It is necessary to follow the prescribed dosage and consult your doctor should you expertise any unwanted effects. With correct use and monitoring, Isoptin may help in managing hypertension and scale back the danger of problems related to high blood pressure.
Isoptin, also called verapamil, is a medicine used for controlling high blood pressure. It belongs to the class of calcium channel blockers and works by enjoyable the blood vessels, allowing for clean blood move and decreasing the pressure within the arteries.
High blood pressure, or hypertension, is a common situation affecting millions of individuals worldwide. It happens when the pressure of blood in opposition to the artery partitions is just too high, placing further pressure on the guts and blood vessels. If left uncontrolled, hypertension can lead to critical health issues corresponding to coronary heart disease, stroke, and kidney failure.
Isoptin is mostly safe and well-tolerated by most individuals. However, as with every treatment, there are some attainable unwanted effects. The commonest ones embrace dizziness, headache, and constipation. More severe unwanted facet effects, though uncommon, may include low blood stress, gradual coronary heart fee, and coronary heart rhythm disturbances. It is important to tell your doctor if you experience any of those unwanted aspect effects while taking Isoptin.
Clinical presentation can mimic chronic cholecystitis while radiologically it may raise concern about the presence of a gallbladder tumor hypertension kidney infection buy discount isoptin online. The diagnosis may be made on careful imaging but is often only made following cholecystectomy, as the gallbladder normally contains stones. Acute acalculous cholecystitis Few patients with acute cholecystitis have acalculous inflammation. The condition may be precipitated by major surgery, bacteraemia, trauma, pancreatitis or other serious illness, and may complicate parenteral nutrition. The inflammatory reaction in the gallbladder wall may be intense and severe, leading to gangrene and perforation. In ill patients, percutaneous drainage (cholecystostomy) under ultrasound guidance may be considered, but urgent cholecystectomy is often advisable. Complications occur in up to 7% of patients and may include cholangitis, bleeding and acute pancreatitis. Patients with asymptomatic gallstones are treated expectantly, particularly if they are elderly or suffering from medical conditions likely to increase the risk of surgery. In younger patients, there may be a stronger case for surgery despite the absence of symptoms, particularly if the stones are multiple and likely to cause complications, such as acute pancreatitis or there is a high underlying prevalence of gallbladder cancer within the population being treated. Investigation of patients with suspected gallstones Blood tests A full blood count may reveal a neutrophilia in acute cholecystitis or its complications. An elevated serum bilirubin or alkaline phosphatase may signify the presence of common duct stones. Plain abdominal x-ray As only 15% of gallstones contain enough calcium to be seen on a plain radiograph, this investigation is not used in diagnosis. Gas is rarely seen outlining the biliary tree if there is a fistula between the biliary tract and the gut, as in gallstone ileus or following endoscopic sphincterotomy. Stones reflect the ultrasonic wave and are thrown into prominence by the acoustic shadow they produce. As it does not depend on hepatic excretion of contrast, it can be used in both jaundiced and nonjaundiced patients. However, it cannot accurately assess the common bile duct with regard to the presence or absence of stones. Once a patient with gallstones becomes symptomatic, elective day case laparoscopic cholecystectomy is indicated. For those patients with common bile duct stones duct clearance and cholecystectomy should be considered irrespective of symptoms. Common bile duct stones can be removed by the principles of surgical treatment involve removal of the gallbladder and the stones it contains, while ensuring that no stones remain within the ductal system. Conversion from a laparoscopic procedure to open cholecystectomy should be seen as a limitation of the minimally invasive technique and not as a failure of the surgeon. Injury to the bile duct during cholecystectomy requires immediate referral to a surgeon or service specialised in the management of such a complication. Open cholecystectomy the gallbladder is usually approached through a right subcostal incision. The peritoneal layer can gently be incised with minimal diathermy and then blunt dissected to expose the contents of the hepatobiliary triangle; this can be repeated for the posterior surface. With the cystic duct and artery clearly identified and skeletonised, intraoperative cholangiography is performed under image intensification by cannulating the cystic duct and following the injection of contrast. The cholangiogram displays the anatomy of the duct system, identifies ductal stones, and confirms that contrast passes freely into the duodenum. The cystic duct and artery are ligated and divided and the gallbladder is removed. The surgeon must be very aware of the possibility of fibrosis having drawn in the right portal structures such that they are easily damaged during such dissection. Here the peritoneal surface of the gallbladder is incised well clear of any potential portal structures, all stones evacuated and the cystic duct orifice identified from within the gallbladder and safely oversewn. Some surgeons pursue a policy of selective cholangiography, obtaining a cholangiogram only in patients at high risk of having ductal stones. The intra- and extrahepatic ducts are seen and there is flow of contrast into the duodenum. A small radiolucent calculus is present at the lower end of the common bile duct (arrow). This is a warning sign of severe fibrosis and this situation presents a high risk of duct injury if attempts are made to dissect the hepatobiliary triangle or perform fundus-first cholecystectomy. A safer option is to open the gallbladder as seen here and extract the stones and drain the gallbladder remnant. In event of biliary fistula it can be controlled by endoscopic retrograde cholangiopancreatography and stenting. The value of routinely placing an abdominal drain has been questioned although its use in difficult surgery may prevent the development of a collection and identify leakage of bile. The gallbladder and bile ducts · 227 Laparoscopic cholecystectomy Laparoscopic cholecystectomy is now the treatment of choice for symptomatic gallstones, despite having a significantly higher risk of major bile duct injury. Thus it is crucial surgeons performing such surgery create a culture of safety by understanding the steps required for safe cholecystectomy and understanding factors that contribute to bile duct injury. This posterior dissection is a key difference to the open approach to cholecystectomy.
When the gastric mucosal cells become less uniform in size, shape and organisation, dysplastic changes may result and may be low or high grade blood pressure 80 over 60 order cheap isoptin line. Hereditary diffuse gastric cancer: Inherited mutations of the E-cadherin gene can result in an aggressive form of signet ring gastric adenocarcinoma affecting young patients. Consequently, patients with a strong family history of gastric cancer should be referred for genetic counselling and, if appropriate, offered endoscopic surveillance and/or a prophylactic total gastrectomy. This type of cancer is confined to the most superficial layers of the stomach wall and is independent of the occurrence of lymph node metastasis (which can be present in a small minority of patients). Such tumours, if adequately treated surgically, are associated with 5-year survival rates in excess of 90%. The survival rate will depend upon the depth of invasion of the tumour and the presence or absence of lymph node metastases at the time of surgical excision. Advanced gastric cancer the vast majority of malignant gastric tumours found in Western countries are locally advanced gastric adenocarcinomas. These tumours have invaded into the muscularis propria and sometimes through to the serosa. The risk of peritoneal metastases and lymphovascular invasion is much higher than for early tumours. Advanced gastric tumours often invade the adjacent gastric wall via submucosal lymphatics creating a diffusely thickened and rigid stomach (linitis plastica). Factors affecting survival in advanced gastric cancer the survival of patients with advanced gastric cancer depends upon the stage of the tumour at presentation and on the general fitness of the patient. Treatment with curative intent implies surgical resection, increasingly combined with perioperative chemotherapy. Diagnosis Diagnosis is made on the basis of a thorough medical history, clinical examination and an upper gastrointestinal endoscopy and biopsy. Patients deemed potentially fit enough for radical therapy should have a series of staging investigations. Learning curves of surgeons and centres performing low-volume cancer surgery may confound any benefit of more radical surgery. Poor survival has been correlated with depth of tumour invasion through the stomach wall, involvement of tumour resection margins and the presence of lymph node metastases. Transgression of the tumour through the stomach wall is associated with poor survival, as the tumour is able to spread transperitoneally and therefore seed the peritoneum with malignant cells, making complete surgical excision impossible. A comprehensive pathological classification of tumours has enabled the prognosis of a particular stage of cancer to be estimated. Such staging is usually classified according to the tumour size (T), the node status (N), and the presence or absence of distant metastases (M) (Table 13. This should provide information about the M-stage (liver, lung, peritoneum and distant nodes) and can help exclude T4 involvement of adjacent structures such as the pancreas. Peritoneal washings are also helpful as patients with positive peritoneal cytology for malignancy have a very poor prognosis and rarely benefit from surgery. Such symptoms should not be overlooked and should not be treated without further investigation, particularly in patients in a vulnerable age group (>40 years). More advanced gastric cancer tends to be associated with weight loss, anaemia, dysphagia, vomiting, epigastric or back pain, or the presence of an epigastric mass. Those with potentially curable disease who are deemed fit enough for radical therapy have the following options: · Surgery alone: Patient with early gastric cancer should undergo a distal (subtotal) or total D2 gastrectomy Table 13. Gastric neoplasia · 201 (depending upon the site of the tumour) done by an experienced surgeon working in a high-volume cancer centre. Groups 1 to 6 are called N1 nodes (first tier nodes or perigastric lymph nodes) and groups 7 to 12 are N2 nodes (second tier nodes along the named gastric arteries). When oncologically safe to do so, a distal gastrectomy is preferable to a total gastrectomy as it gives a better quality of life. The chemotherapeutic agents used include epirubicin, cisplatin and 5-fluorouracil. Newer agents such as oxaliplatin, cepcetabine and bevacizamab can improve survival further. Eating can be particularly difficult for patients with advanced gastric cancer and dietetic support is essential. Towards the end of life, the patient may need medication via a subcutaneous infusion from a portable syringe driver. Palliative chemotherapy: For patients who are fit enough, valuable improvements in quality of life can be achieved with palliative chemotherapy using combinations of drugs such as epirubicin, cisplatin and 5-fluorouracil. Palliative radiotherapy: Bleeding from advanced gastric tumours can be troublesome and can be greatly reduced by a short course of external beam radiation. Stenting: Patients with gastric outlet obstruction who have persistent vomiting may benefit from the endoscopic placement of a self-expanding metallic stent although results are unpredictable. Options include a gastric bypass (often done laparoscopically) for distal tumours, or palliative resection. The latter is a big undertaking for patients with incurable disease and should only be considered in fit patients with distal tumours who have not benefited from lesser interventions. Palliative surgery should not be attempted in the presence of gross ascites or jaundice because of the poor outcome. Occasionally, lymphomas may transform to a highgrade type of tumour that carries a poorer prognosis and require more aggressive treatment with chemotherapy. Newer combinations with irinotecan- or taxane-based regimens show promising results.
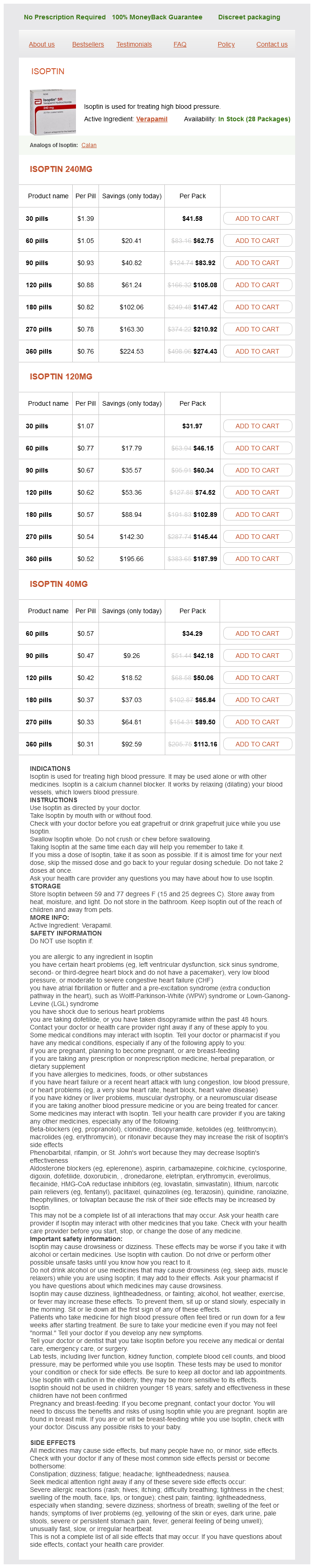
Isoptin Dosage and Price
Isoptin 240mg
- 30 pills - $41.58
- 60 pills - $62.75
- 90 pills - $83.92
- 120 pills - $105.08
- 180 pills - $147.42
- 270 pills - $210.92
- 360 pills - $274.43
Isoptin 120mg
- 30 pills - $31.97
- 60 pills - $46.15
- 90 pills - $60.34
- 120 pills - $74.52
- 180 pills - $102.89
- 270 pills - $145.44
- 360 pills - $187.99
Isoptin 40mg
- 60 pills - $34.29
- 90 pills - $42.18
- 120 pills - $50.06
- 180 pills - $65.84
- 270 pills - $89.50
- 360 pills - $113.16
Improvement in pain was not predictive of improvement in a desire for a hastened death arterial ulcer order isoptin 240 mg. However, a change in depression severity was predictive of hastened death desire, thus illustrating that depression needs to be both better recognized as well as better treated in this population. Is there a standard of care for the radical management of non-small cell lung cancer involving the apical chest wall (Pancoast tumours)? Tumor of the thoracic inlet producing the Pancoast syndrome: a report of 17 cases and a review of the literature. Clinical significance of Pancoast syndrome: a reference to the early diagnosis of the bronchial cancer. Cervicobrachialgia and Pancoast tumor: value of standard anteroposterior cervical radiographs in early diagnosis. Surgical treatment of superior sulcus tumors with spinal and brachial plexus involvement. Induction chemoradiation and surgical resection for non-small cell lung carcinomas of the superior sulcus: initial results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). Factors determining outcome after surgical resection of T3 and T4 lung cancers of the superior sulcus. Brachial plexopathy in apical non-small cell lung cancer treated with definitive radiation: dosimetric analysis and clinical implications. Radiation-induced brachial plexopathy: neurological follow-up in 161 recurrence-free breast cancer patients. Dose constraints to prevent radiation-induced brachial plexopathy in patients treated for lung cancer. Electrophysiological findings in patients who received radiation therapy over the brachial plexus: a magnetic stimulation study. Pancoast tumor: five-year survival without recurrence or metastases following radical resection and postoperative irradiation. Combined chest wall resection with vertebrectomy and spinal reconstruction for the treatment of Pancoast tumors. High-dose radiotherapy in trimodality treatment of Pancoast tumors results in high pathologic complete response rates and excellent long-term survival. Survival after trimodality treatment for superior sulcus and central T4 non-small cell lung cancer. Non-small cell lung carcinoma of the superior sulcus: favourable outcomes of combined modality treatment in carefully selected patients. Superior sulcus tumors: treatment selection and results for 85 patients without metastasis (Mo) at presentation. Nociceptive and neuropathic pain in patients with lung cancer: a comparison of pain quality descriptors. Therapeutic effects of peripheral magnetic stimulation on traumatic brachial plexopathy: clinical and neurophysiological study. Does interscalene catheter placement with stimulating catheters improve postoperative pain or functional outcome after shoulder surgery? Continuous interscalene block using a stimulating catheter: a review of the technique. Influence of stimulating different cords on the efficacy of infraclavicular brachial plexus block. Differential efficacy of electric motor cortex stimulation and lesioning of the dorsal root entry zone for continuous vs paroxysmal pain after brachial plexus avulsion. Dorsal root entry zone lesioning for pain after brachial plexus avulsion: results with special emphasis on differential effects on the paroxysmal versus the continuous components. Dorsal root entry zone lesions for treatment of pain-related to radiation-induced plexopathy. Dorsal root entry zone lesions for phantom limb pain with brachial plexus avulsion: a study of pain and phantom limb sensation. Follow-up 26 years after dorsal root entry zone thermocoagulation for brachial plexus avulsion and phantom limb pain. Radiofrequency lesions of the stellate ganglion in chronic pain syndromes: retrospective analysis of clinical efficacy in 86 patients. Pulsed radiofrequency treatment within brachial plexus for the management of intractable neoplastic plexopathic pain. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Cellular and molecular insights into neuropathy-induced pain hypersensitivity for mechanism-based treatment approaches. Glycine inhibitory dysfunction induces a selectively dynamic, morphine-resistant, and neurokinin 1 receptor-independent mechanical allodynia. Membrane potential oscillations in dorsal root ganglion neurons: role in normal electrogenesis and neuropathic pain. Peripheral effects of morphine and expression of mu-opioid receptors in the dorsal root ganglia during neuropathic pain: nitric oxide signaling. Downregulation of tetrodotoxin-resistant sodium currents and upregulation of a rapidly repriming tetrodotoxin-sensitive sodium current in small spinal sensory neurons after nerve injury. Time course and specificity of the pharmacological disruption of the trafficking of voltage-gated calcium channels by gabapentin. The use of pindolol with fluoxetine in the treatment of major depression: final results from a double-blind, placebo-controlled trial.