Januvia
General Information about Januvia
It is an oral treatment that helps to control blood sugar levels by stimulating the production of insulin and decreasing the production of glucose within the liver.
Januvia is not suitable for everyone, and it is essential to discuss any medical circumstances or drugs with a healthcare supplier earlier than starting treatment. Pregnant or breastfeeding women also needs to seek the guidance of with their doctor earlier than taking Januvia.
Type 2 diabetes is a chronic situation where the body either doesn't produce enough insulin or does not successfully use the insulin that's produced. Insulin is a hormone that helps to manage blood sugar ranges, and without sufficient of it, glucose ranges can turn into too excessive. This can lead to severe health problems similar to coronary heart illness, kidney harm, and nerve damage.
One of the principle advantages of Januvia is that it's an oral medication, which means it may be taken in tablet kind rather than injected like some other diabetes medicines. This makes it far more convenient and user-friendly for patients who will not be snug with injecting themselves. Additionally, Januvia does not cause weight gain, which is a common facet impact of many other diabetes medicines.
Januvia is typically taken once every day, with or with out food. The dosage may differ depending on the person's needs, but it is important to comply with the prescribed dosage and directions from a healthcare supplier. It can additionally be essential to frequently monitor blood sugar levels while taking Januvia to ensure that it's successfully controlling blood sugar levels.
Januvia, or sitagliptin, is a medication that belongs to a category of drugs called DPP-4 inhibitors. These medicine work by inhibiting the enzyme DPP-4, which breaks down a hormone known as incretin. When this hormone just isn't damaged down, it stimulates the pancreas to supply more insulin and also helps to reduce the production of glucose in the liver. This helps to control blood sugar ranges and forestall them from getting too high.
In conclusion, Januvia is a extensively used and effective medication for the remedy of kind 2 diabetes. It helps to control blood sugar levels and prevent serious issues related to the condition. However, you will want to comply with directions and monitor blood sugar levels frequently whereas taking this medicine. By working closely with a healthcare provider, individuals with type 2 diabetes can successfully handle their condition and live a more healthy life.
Like any treatment, Januvia could cause side effects in some individuals. Common side effects embrace headache, runny or stuffy nose, sore throat, and higher respiratory tract infections. In rare instances, serious unwanted effects similar to pancreatitis, allergic reactions, and liver issues may happen. It is necessary to hunt medical consideration if any extreme or persistent unwanted side effects are experienced.
They are perhaps limited to the suspicion of proximal iliac artery disease or clamp injury and an obese recipient in whom visualization of the renal artery and iliac vessels is not technically feasible blood sugar 67 proven januvia 100 mg. Without suction it is withdrawn slowly with a twisting motion to dislodge fatty tissue trapped in the small side holes of the drain as a result of the suction. Small pediatric kidneys have been known to undergo torsion of the vascular pedicle on removal of the drain with resultant loss of graft function. The timing of drain tube removal depends on the volume and nature of the drained fluid. It is not unusual to record 100 to 200 mL of heavily blood-stained drainage in the first few hours of transplantation. Drainage volume can be an unreliable gauge of active bleeding, particularly if brisk. Patient discomfort, tachycardia, hypotension, and abdominal findings of an enlarging mass around the transplant are indicators of a significant bleed requiring urgent surgical exploration. Large-volume drainage of less heavily blood-stained fluid generally indicates residual peritoneal dialysate (if the peritoneum was breached), lymph, or urine. Urine is excluded by biochemical analysis or absence of glucose on dipstick testing. The careful positioning of the kidney at time of surgery can be undone readily by a restless recipient flexing the hips because of pain, urinary catheter intolerance, and hypoxia, or an unhelpful radiographer who determines that the recipient should sit bolt upright for a mobile chest x-ray. Transplanted kidneys producing urine at the end of the surgical procedure are easier to manage, particularly if urine is being produced in volumes that could not be achieved by residual native kidney function. If no urine has been seen on the operating table or in recovery and the recipient is hemodynamically stable with a central venous pressure of at least 5 cmH2O, ultrasound examination is useful before the recipient leaves the operating suite complex, particularly if difficulty was encountered with kidney positioning during wound closure. Out of routine working hours, it helps if the transplant surgeon is adept with the use of an ultrasound machine dedicated to the transplant unit. An inadequate arterial signal and significant collections are indications for an immediate return to the operating room. However, when the patient is placed in a sitting or standing position, downward movement of abdominal contents can cause external compression of the transplanted kidney or change its position. Contributing factors include a large native polycystic kidney, heavy fat-laden small-bowel mesentery, and greater omentum in a patient with truncal obesity. A paralytic ileus or pseudoobstruction of the large bowel can be frustrating to manage in the first week after transplantation. It demonstrates a small disruption of the anastomosis (arrow) that led to catastrophic bleeding 10 days after transplant surgery. The perfusion of the kidney transplant in the right iliac fossa was compromised by gross pseudoobstruction of the large and small bowel. Surgical decompression with insertion of a mesh to relieve pressure may be required. Most hematomas are small and insignificant ultrasound findings that resolve spontaneously. Those associated with discomfort, hypotension, transplant dysfunction, and falling hemoglobin are not. Others expand progressively within the retroperitoneal space with inevitable external pressure on the transplant and adverse effect on arterial blood inflow or venous outflow. Ultrasound examination is appropriate to assess transplant perfusion but because of surrounding bowel gas is unreliable for assessment of hematoma size. Indications for surgical exploration of the transplanted kidney include symptoms, progression of size, ongoing blood loss, and transplant dysfunction. Surgical exploration in the first day or so after transplantation for hematoma evacuation might locate active bleeding from a hilar vessel, a retroperitoneal vein, or divided abdominal wall muscle. Bruising in dependent subcutaneous areas lateral to and below the transplant, such as the labia or the scrotum, is often seen several days later. The risk of hematoma formation is increased by the use of anticoagulants, particularly in patients receiving heparin by infusion for prophylaxis against vascular thrombosis. The reported risk of need for surgical intervention in patients heparinized after transplantation is 30% to 60%. They are prescribed increasingly on a long-term basis by cardiologists and nephrologists in patients with significant cardiovascular disease or in attempts to improve fistula patency. However, they do reduce the margin for surgical error and dictate the need for meticulous hemostasis at time of surgery. Compared with other forms of vascular surgery, the incidence of thrombosis is low, perhaps because of the highly vascular nature of the kidney. The low incidence may also support the traditional view that renal failure is associated with a bleeding tendency secondary to platelet and clotting factor dysfunction. Interruption of the venous drainage can be spectacular with graft rupture and bleeding. It has an equally disappointing prospect for kidney salvage because of the rapidity of the process after occlusion of the renal vein has occurred. Thrombotic complications are minimized by identification and management of risk at the time of transplantation. Thrombosis of the kidney vasculature is the end result of stasis, endothelial changes, and procoagulant factors and can be multifactorial. Causes of stasis are largely technical in nature and readily identifiable at the time of transplant exploration. They include poorly constructed anastomoses, malpositioning of the transplant, rotation of the kidney, or external compression.
Abstinence from chemical dependency would be regarded as essential for acceptance to the transplant waiting list by most transplant programs diabetes type 1 financial help cheap 100 mg januvia otc, but it is difficult to assure and monitor in practice. It is important to optimize control of the features of renal bone disease, with special attention to attempting to normalize the calcium phosphate product to minimize hyperparathyroidism, osteoporosis, and vascular calcification after transplantation. Duration before considering transplantation = the period after apparent successful cure of the individual cancer when transplantation may be considered if investigations substantiate cure of the cancer. Recurrence of cancer has been recorded despite disease-free periods exceeding those suggested here. Each individual patient must be assessed individually and these intervals may be too long or too short for individual circumstances. Multiple myeloma needs specific consideration of prior bone marrow transplantation. Transmission of tropical and geographically restricted infections during solid-organ transplantation. The incidence of untreated Helicobacter pylori/peptic ulcer disease is now quite low and many units use either low dose or complete avoidance of steroids combined with a proton pump inhibitor to prevent peptic ulceration, despite the potential for interaction with immunosuppressant drug absorption. Although the results in those specialized centers are encouraging there is still insufficient evidence to lead to widespread adoption of islet transplants outside of clinical trials. The procedure is more demanding on both surgeon and patient, it takes longer, and involves the additional risk of pancreas exocrine drainage either into the bladder or, more commonly, into the bowel. Postoperative recovery takes longer because of the ileus induced by the bowel surgery and immunosuppression is on the whole more intense than for a simple kidney transplant. Against these issues, the patient must set the benefits of good glucose control without exogenous insulin administration, reduced long-term complications of diabetes, and improved survival compared with a deceased donor kidney alone. The role of islet transplantation is still evolving such that Type 2 Diabetes Mellitus Transplantation of the majority of patients with end-stage renal failure resulting from type 2 diabetes represents a challenge to both surgical and medical expertise. The epidemic of type 2 diabetes that is sweeping both the developed and developing world has led to more than threefold increases in the number of people commencing renal replacement therapy. Obesity is being tackled in some centers by pretransplant bariatric surgery, with some success in motivated patients. The exceptions to this rule are from recurrent disease in primary oxalosis and in the presence of antiglomerular basement membrane antibodies in Goodpasture syndrome. The causes of renal failure in Australian patients commencing dialysis and those receiving a renal transplant are shown in Table 4. It is important to distinguish between the risk of recurrence and the prognosis of the graft with recurrence. Risk factors for recurrence include young age of the recipient, the duration of native disease from onset to development of end-stage renal failure, mesangial proliferative pathology, and the possibility that the risk is higher in related donor grafts. The disease may result from a circulating glomerular permeability factor, encouraging use of plasma exchange to control disease. Recurrence rates are high, especially if sought in renal biopsies after transplantation using specific identification of IgA deposits in the glomeruli. IgA is thus risk of de novo antiglomerular basement membrane antibody-mediated Goodpasture syndrome. There have been substantial advances in the understanding of a range of diseases that produce hemolytic uremic syndromes. The option of posttransplant treatment of such patients with eculizumab has released these patients from a life of failed transplants and dialysis. There is very little recent experience of recurrence of Goodpasture syndrome after transplantation because of the early and convincing reports of recurrence in the presence of circulating antibody and advice to await clearance before transplantation. Primary oxalosis has a high recurrence rate after transplantation and is now best treated by combined kidney and liver transplantation, correcting the metabolic abnormality simultaneously. The former leads to recurrent disease in the transplant but the latter only to extrarenal deposition of cystine. Both are, to a certain extent, treatable and recurrent diseases that should be preventable with recombinant alpha-galactosidase A enzyme replacement and oral analogs of cysteamine, respectively. More subtle problems that may be encountered include asymptomatic prostatic enlargement in an anuric dialysis dependent patient and the very small capacity bladder that will be encountered in long-term dialysis patients who have been anuric for many years. Creation of alternative bladder conduits is less popular than in the past because of the morbidity of the surgical procedures required. Indwelling or suprapubic catheters followed by prostatectomy or self-catheterization are the standard approaches today for the majority of patients with bladder dysfunction. Recurrent urinary tract infection and reflux nephropathy seldom lead to life-threatening septicemia before transplantation, but when the pretransplant experience of an individual demonstrates otherwise, bilateral nephrectomy can be justified if antibiotic prophylaxis fails to ameliorate the risk. Recurrent urinary sepsis is much more common after transplantation despite prophylactic measures and may threaten both the graft and the patient. Bilateral native nephrectomy thus becomes the lesser risk in a few patients after transplantation. The size of polycystic kidneys must be evaluated before transplant surgery, preferably by the surgeon who will be implanting the new kidney. Unilateral nephrectomy may be needed between the onset of dialysis therapy and a renal transplant, precluding preemptive transplantation, though concurrent transplant and nephrectomy is also advocated. Pretransplant recognition of the patient with bladder dysfunction is important to avoid immediate problems during and after surgery. Patients with the triad syndrome or other congenital obstructive uropathy, spina bifida, and diabetes are at easily recognizable risk of poor Coagulation Disorders Hemorrhage during the transplant and coagulation of the graft or other vital vascular conduit after the operation require careful prediction and management. Coagulation disorders and the risk of thrombosis are much more predictable today through screening tests (Box 4. Use of heparin starting soon after transplantation in those identified as having a possible thrombotic tendency seems to reduce the risk of thrombosis. Iatrogenic hemorrhage is much more common than inherited disorder such as hemophilia, especially with the widespread use of anticoagulation for atrial fibrillation and after vascular stenting.
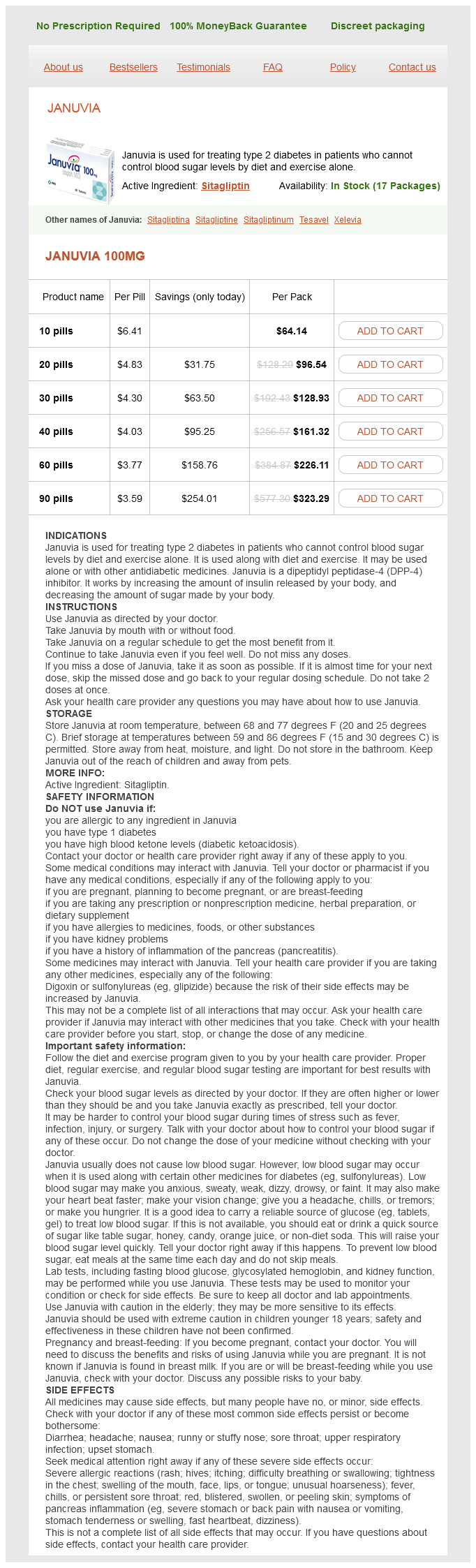
Januvia Dosage and Price
Januvia 100mg
- 10 pills - $64.14
- 20 pills - $96.54
- 30 pills - $128.93
- 40 pills - $161.32
- 60 pills - $226.11
- 90 pills - $323.29
The management of communityacquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America diabetes quality measures discount januvia 100 mg with amex. A randomized, prospective study of pediatric patients with community-acquired pneumonia treated with ceftaroline versus ceftriaxone. Incidence and severity of childhood pneumonia in the first year of life in a South African birth cohort: the Drakenstein Child Health Study. Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Burden of disease caused by Haemophilus influenzae type b in children younger than 5 years: global estimates. Macronutrients during pregnancy and life-threatening respiratory syncytial virus infections in children. Role of Mycoplasma pneumoniae and Chlamydia pneumoniae in children with community-acquired lower respiratory tract infections. Characteristics of Streptococcus pneumoniae and atypical bacterial infections in children 25 years of age with community-acquired pneumonia. Early impact of 13-valent pneumococcal conjugate vaccine on community-acquired pneumonia in children. Serotype distribution and antimicrobial resistance patterns in Streptococcus pneumoniae isolates from hospitalized pediatric patients with respiratory infections in Shanghai, China. Haemophilus influenzae type-b and non-b-type invasive diseases in urban children (<5years) of Bangladesh: implications for therapy and vaccination. Aetiology of childhood pneumonia in a well vaccinated South African birth cohort: a nested casecontrol study of the Drakenstein Child Health Study. Impact and effectiveness of 10 and 13-valent pneumococcal conjugate vaccines on hospitalization and mortality in children aged less than 5 years in Latin American countries: a systematic review. Epidemiology of invasive group a streptococcus disease in the United States, 19951999. Community-acquired necrotizing pneumonia due to methicillin-sensitive Staphylococcus aureus secreting Panton-Valentine leukocidin: a review of case reports. Necrotising pneumonia is an increasingly detected complication of pneumonia in children. The microbiome of the human lower airways: a next generation sequencing perspective. Aspiration and non-aspiration pneumonia in hospitalized children with neurologic impairment. Cytokine concentrations in plasma from children with severe and non-severe community acquired pneumonia. Pneumonia caused by Mycoplasma pneumoniae and Chlamydophila pneumoniae in children-comparative analysis of clinical picture. Can we predict which children with clinically suspected pneumonia will have the presence of focal infiltrates on chest radiographs Clinical features for diagnosis of pneumonia in children younger than 5 years: a systematic review and meta-analysis. A systematic review on the diagnosis of pediatric bacterial pneumonia: when gold is bronze. Clinical symptoms and signs for the diagnosis of Mycoplasma pneumoniae in children and adolescents with community-acquired pneumonia. Uncomplicated pneumonia in healthy Canadian children and youth: practice points for management. Diagnosis and management of community-acquired pneumonia in childhood-South African Thoracic Society guidelines: clinical guideline. Management of community-acquired pediatric pneumonia in an era of increasing antibiotic resistance and conjugate vaccines. Ambulatory short-course high-dose oral amoxicillin for treatment of severe pneumonia in children: a randomised equivalency trial. Clinical efficacy of 3 days versus 5 days of oral amoxicillin for treatment of childhood pneumonia: a multicentre double-blind trial. Short-course versus long-course intravenous therapy with the same antibiotic for severe community-acquired pneumonia in children aged two months to 59 months. Nasopharyngeal colonization and penicillin resistance among pneumococcal strains: a worldwide 2004 update. Decreasing rates of resistance to penicillin, but not erythromycin, in Streptococcus pneumoniae after introduction of a policy to restrict antibiotic usage in Taiwan. Rationale for revised penicillin susceptibility breakpoints versus Streptococcus pneumoniae: coping with antimicrobial susceptibility in an era of resistance. Pediatric invasive pneumococcal disease in the United States in the era of pneumococcal conjugate vaccines. Azithromycin iv pharmacodynamic parameters predicting Streptococcus pneumoniae killing in epithelial lining fluid versus serum: an in vitro pharmacodynamic simulation. Usefulness of consecutive C-reactive protein measurements in follow-up of severe communityacquired pneumonia. Interobserver agreement in the radiological diagnosis of lower respiratory tract infections in children. Intraobserver and interobserver agreement of the interpretation of pediatric chest radiographs. Does the lateral chest radiograph help pediatric emergency physicians diagnose pneumonia Occult pneumonias: empiric chest radiographs in febrile children with leukocytosis. Randomised controlled trial of clinical outcome after chest radiograph in ambulatory acute lowerrespiratory infection in children.