Kamagra Polo
General Information about Kamagra Polo
Kamagra Polo is an oral medication that's specifically designed to deal with ED and its symptoms. It is a chewable version of the well-known medication, Viagra, and is manufactured by Ajanta Pharma, a renowned pharmaceutical firm. Kamagra Polo accommodates the active ingredient Sildenafil Citrate, which belongs to a gaggle of medicines called phosphodiesterase sort 5 (PDE5) inhibitors. It works by rising blood circulate to the penis, permitting for a stronger and longer-lasting erection.
Kamagra Polo: A Revolutionary Solution for Erectile Dysfunction
Erectile dysfunction (ED) is a typical downside affecting men of all ages. It refers again to the lack of ability to realize or preserve an erection that's firm enough for sexual activity. This condition could cause important distress and have a unfavorable impression on a person's self-esteem and their intimate relationships. Fortunately, there are various remedy choices available, and one such resolution is Kamagra Polo.
Moreover, Kamagra Polo has an extended duration of action, with results lasting as much as 6 hours. This implies that men can take pleasure in multiple sexual encounters within a quick time, with out having to fret about losing their erection. However, it's important to note that Kamagra Polo will not trigger an erection unless there's sexual stimulation present.
Kamagra Polo can additionally be a cost-effective option for treating ED. It is significantly cheaper than the branded Viagra, without compromising on its efficacy and safety. This makes it a more accessible option for males who cannot afford or don't have insurance coverage coverage for costly ED medicines.
Like any medicine, Kamagra Polo could trigger some side effects, which are often delicate and temporary. The most common side effects embody headaches, dizziness, facial flushing, and indigestion. These unwanted side effects usually subside because the treatment wears off, and they can be easily managed by staying hydrated and avoiding alcohol consumption. It is significant to consult a physician earlier than taking Kamagra Polo, especially if a person has any underlying medical situations or is taking another medications.
In conclusion, Kamagra Polo is a revolutionary answer for erectile dysfunction. It is a secure, efficient, and handy treatment option that gives men with quick and long-lasting reduction from ED. With its unique kind, quick onset of motion, and longer duration of effect, Kamagra Polo has gained recognition worldwide as a reliable selection for males coping with ED. If you may be fighting this condition, do not hesitate to talk to your physician about Kamagra Polo and see how it can enhance your sexual health and overall well-being.
One of the principle benefits of Kamagra Polo is its convenient and discreet type. The tablet is shaped like a polo mint, and it might be easily chewed and swallowed, without the need for water. This makes it an ideal choice for males who have problem swallowing pills. Additionally, it is available in varied fruity flavors corresponding to pineapple, orange, strawberry, and mint, making it more interesting for individuals who dislike the bitter style of standard ED drugs.
Kamagra Polo has a fast onset of motion, with results kicking in inside 15-30 minutes after consumption. This is much faster than different ED medicines, which may take as a lot as an hour to begin working. This attribute makes it the proper selection for spontaneous sexual exercise, offering men with the confidence and reassurance they should perform sexually.
The purpose of this chapter is to provide an overview of this expanded perspective erectile dysfunction johnson city tn order kamagra polo with a visa. Each unique tissue-engineered device requires a distinctive set of experiments to determine its biological responses and biocompatibility. This article presents an overview of host responses that must be considered in determining the biocompatibility of tissue-engineered devices that employ biomaterials. The three major responses that must be considered for biocompatibility assessment are inflammation, wound healing, and immunological reactions or immunity. For the purposes of biological response evaluation, immunological reactions or immunity are considered to be immunotoxicity. Pathologists use the terminology of inflammation and immunity to describe adverse tissue reactions, whereas immunologists commonly refer to inflammation as innate immunity and activation of the immune system as being acquired immunity. Tissueematerial interactions are a series of responses that are initiated by the implantation procedure, as well as by the presence of the biomaterial, medical device, or tissue-engineered device. In this article, we divide the series of tissueematerial responses into inflammation (innate immunity) and wound healing, and immunotoxicity. After implantation, early, transient tissueematerial responses include injury (implantation), bloodematerials interactions, provisional matrix formation, and the temporal sequence of inflammation and wound healing including acute inflammation, chronic inflammation, granulation tissue development, foreign body reaction, and ultimately fibrosis or fibrous capsule (scar) development. Immunotoxicity is any adverse effect on the function or structure of the immune system or other systems as a result of an immune system dysfunction. Two significant failure mechanisms of tissue-engineered devices are fibrosis or fibrous capsule (scar) development surrounding and infiltrating the tissue-engineered device, or the initiation of acquired or cellular immunity by the biological component of the tissue-engineered device. Also, the biological component and the biomaterial component in a tissueengineered device may act in concert or synergistically to facilitate either of these failure mechanisms. This injury and the subsequent perturbation of homeostatic mechanisms lead to inflammatory responses, foreign body reaction, and wound healing. The response to injury depends on multiple factors that include the extent of injury, loss of basement membrane structures, bloodematerial interactions, provisional matrix formation, the extent or degree of cellular necrosis, and the extent of the inflammatory response. The organ or tissue undergoing implantation may have a significant role in the response. These events, in turn, may affect the extent or degree of granulation tissue formation, foreign body reaction, and fibrosis or fibrous capsule (scar) development [9]. These dependencies thus provide perspectives on the biological response evaluation and the ultimate determination of biocompatibility. The reactions occur or are initiated early (that is, within 2e3 weeks of the time of implantation) and undergo resolution quickly, leading to fibrosis or fibrous capsule formation. BloodeMaterial Interactions and Initiation of the Inflammatory Response Bloodematerial interactions and the inflammatory response are intimately linked; in fact, early responses to injury involve mainly blood and the vasculature [1e8]. Regardless of the tissue into which a biomaterial is implanted, the initial inflammatory response is activated by injury to vascularized connective tissue. Because blood and its components are involved in the initial inflammatory responses, thrombus, blood clot, or both also form. Thrombus formation involves activation of the extrinsic and intrinsic coagulation systems, the complement system, the fibrinolytic system, the kinin-generating system, and platelets. Thrombus or blood clot formation on the surface of a biomaterial is related to the well-known Vroman effect of protein adsorption. From a wound healing perspective, blood protein deposition on a biomaterial surface is described as provisional matrix formation. Although injury initiates the inflammatory response, released chemicals from plasma, cells, and injured tissue mediate the response [4,6,10,11]. Important classes of chemical mediators of inflammation are presented in Table 39. Several important points must be noted to understand the inflammatory response and how it relates to biomaterials. First, although chemical mediators are classified on a structural or functional basis, different mediator systems interact and provide a system of checks and balances regarding their respective activities and functions. Second, chemical mediators are quickly inactivated or destroyed, which suggests that their action is predominantly local. Third, generally acid, lysosomal proteases, and oxygen-derived free radicals produce the most significant damage or injury. Phagolysosomes in macrophages can have acidity as low as pH 4, and direct microelectrode studies of this acidic environment have determined pH levels to be as low as 3. Moreover, only several hours are necessary to achieve these acid levels after adhesion of macrophages [12e14]. The predominant cell type present in the inflammatory response varies with the age of the injury. In general, neutrophils, commonly called polymorphonuclear leukocytes or polys, predominate during the first several days after injury and then are replaced by monocytes as the predominant cell type. After emigration from the vasculature, monocytes differentiate into macrophages, and these cells are very long-lived (up to months) [3]. Monocyte emigration may continue for days to weeks, depending on the injury and implanted biomaterial, and chemotactic factors for monocytes are activated over longer periods of time. Provisional Matrix Formation Injury to vascularized tissue in the implantation procedure leads to immediate development of the provisional matrix at the implant site. This provisional matrix consists of fibrin, produced by activation of the coagulative and thrombosis systems, and inflammatory products released by the complement system, activated platelets, inflammatory cells, and endothelial cells [15e18].
Because of the increasing resolution and speed of bioprinters erectile dysfunction hypogonadism buy cheap kamagra polo 100 mg on line, the structures that may be fabricated are becoming highly complex. The ability to precisely reproduce the structural and biochemical microarchitecture of tissues will most certainly result in more physiologically normal cellular function in bioprinted constructs. Several biological constructs have been fabricated using current bioprinting technology. Liver organoids have been generated using microextrusion bioprinting technology that includes several liver cell types suspended in a supportive hydrogel. These constructs demonstrated exceptionally high levels of liver tissue function and maintained viability in the long term, which makes them ideal candidates for tissue-on-a-chip applications [36]. Skin substitutes have also been created using a laser-based bioprinting technology, which allowed the precise placement of cells associated with specific layers of the skin. The resulting skin constructs were implanted into rodent wound models and demonstrated robust neovascularization, differentiation of mature keratinocytes, and the generation of a normal dermal basal lamina, all hallmarks of native skin [37]. Logistical obstacles continue to limit applications in whole-organ biofabrication. However, the speed, reproducibility, and scalability of bioprinting make it an ideal complement to body-on-a-chip modeling. Liver-on-a-Chip Early tissue/organoid-on-a-chip devices were geometrically designed to drive cell aggregation, thereby creating multicellular organoids. For example, devices were designed with microwells with a convergent geometry that terminated in a cell substrate of some type. Based on the microwell design, liver-derived cell lines could be formed into either spheroid or cylindrical constructs in a highly controlled manner. These 3D constructs maintained much better cellular function than did 2D controls [38,39]. In another example, spheroids were created from a cell line using an array of channels connecting inverted, pyramid-shaped microwells, allowing for the delivery of cells and test compound to multiple chambers simultaneously. This integration of microfluidics with an array of microreactors greatly increased the throughput potential for drug screening [40]. They often employ controlled fluid flow to address nutrient circulation, drug or toxin administration, sample collection, and the integration of liver organoids with other tissue types. Our group employed a versatile photopolymerizable hyaluronic acid biopolymer system for in situ photopatterning of HepG2 cells to generate 3D liver constructs. The constructs were formed in parallel channel fluidic devices that were fabricated by soft lithography and molded polydimethylsiloxane. This system was used for toxicity screening by administering multiple alcohol concentrations within each chip. As expected, alcohol administration resulted in a dose-dependent decrease in viability and cellular function [14]. Efforts within our group are focused on miniaturizing this and other systems to increase throughput further. Miniaturization and microfabrication approaches can be employed to generate more intricate biological microarchitecture such as liver sinusoids. Precise seeding and layering of hepatocytes and endothelial cells within microfluidic circuits can be used to generate structures with the resolution required to produce sinusoid-like models [42]. Another approach to generating biologically relevant microarchitecture involves mating synthetic and biological components. As an example, semiporous membrane to separate two adjacent chambers may be used to partition human hepatocytes from sinusoidal endothelial cells. Such a design was shown to generate higher albumin and urea production compared with traditional hepatocyte cultures; it demonstrates another strategy for recapitulating normal microarchitecture to increase cell function [43]. Vessel-on-a-Chip the term "microfluidics" carries with it the assumption of controlled fluid routing. Moreover, because drugs are generally introduced directly to the bloodstream or enter the bloodstream shortly after oral or airway introduction, fluidic systems that mimic the role of the 774 44. A substantial number of vascular-like fluidic devices have been developed, including both straight channels devices [44,45] and fluidic devices with more complex, branching features [46,47]. One major role of the vascular system, beyond transporting nutrients and oxygen among tissues, is to transport drugs and other molecules to sites throughout the body, where they pass through the endothelium into adjacent tissues. Many microfluidic systems have been designed to model the transendothelial delivery of test compounds to a target tissue. As an example, a device was developed that includes two perpendicular channels that cross at a single point. A semipermeable membrane colonized with an endothelial cell monolayer was positioned at the point where the two channels cross. Fluorescently labeled albumin was introduced into one channel and transport through the endothelial monolayer was quantified by laser excitation of the fluorophore in the other channel [48]. In another example, an endothelialized construct was designed with a mechanism to control shear stress experienced by the endothelial cells. The device was used to determine the effect of fluid shear on nanoparticle translocation across the endothelial monolayer. These studies were intended to define the ability of flow and shear stress to model different types of vasculature in terms of the contribution to pharmacokinetics and drug biodistribution [49]. Other microfluidic devices with integrated vasculature have been developed to determine how the atomic structure of drugs and nanoparticles can influence the rate of translocation across an endothelium [50]. The integration of vascular function in organ-on-a-chip microfluidic design shows great promise in providing more accurate modeling of drug pharmacology in next-generation in vitro cell platforms. Lung-on-a-Chip the lungs, which represent a fluideair interface between the aqueous in vivo environment and the extracorporeal environment, serve as a common port of entry for drugs, toxins, pathogens, and other xenobiotic compounds. Accurate modeling of the lung in organ-on-a-chip systems is likely important for relevant modeling of the effects of agents that enter the circulation through the alveoli. Significant advancements have been made in the on-chip modeling of lung tissue [51].
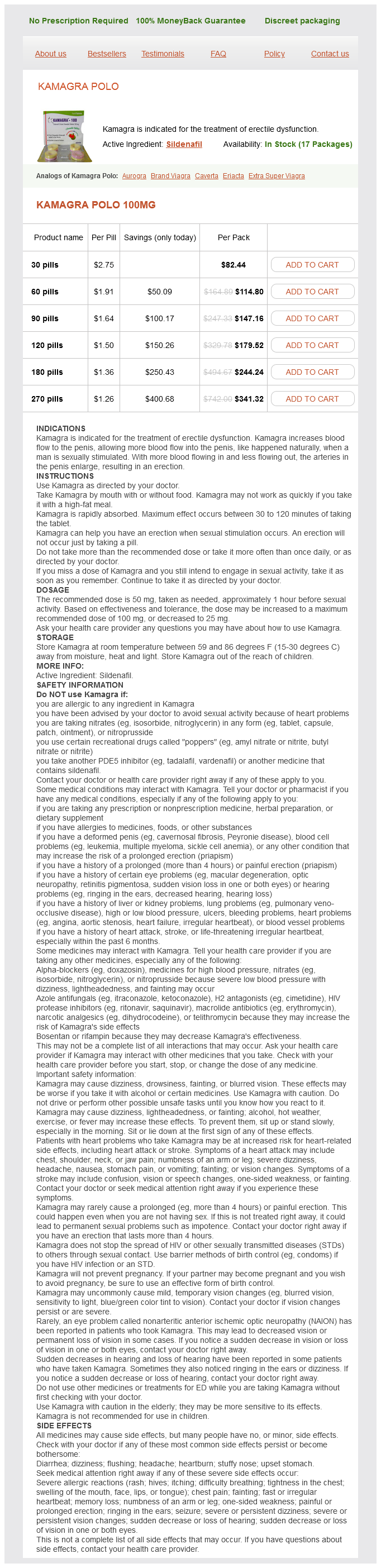
Kamagra Polo Dosage and Price
Kamagra Polo 100mg
- 30 pills - $82.44
- 60 pills - $114.80
- 90 pills - $147.16
- 120 pills - $179.52
- 180 pills - $244.24
- 270 pills - $341.32
Mechanically xylitol erectile dysfunction 100 mg kamagra polo purchase mastercard, they are weak and not stiff, and they have a tendency to degrade quickly. Silk Silks are proteins that are synthesized by Lepidoptera larvae such as silkworms and spiders. They are biosynthesized in epithelial cells and secreted into the lumen of specialized glands, where they are stored and subsequently spun into fibers. The properties of silk vary considerably with their source, with different amino acid sequences and mechanical properties that are fine-tuned to their specific function. The most widely used and investigated silks with respect to biomaterials applications are derived from the domesticated silkworm, Bombyx mori, and from spiders such as Nephila clavipes and Araneus diadematus. Silkworm silk is popular and has been used for medical devices such as sutures for many years; for general textiles, it has been used even longer. This silk has two major fibroin proteins, light (25-kDa) and heavy kDa chains, where the core sequence repeats include alanine-glycine with serine or tyrosine. Spider silk proteins range from 70 to 700 kDa; many such silks are characterized by polyalanine and glycine regions. Spider silk is not easy to harvest, and much emphasis has been placed on the use of genetic engineering techniques to produce synthetic versions. Silk fibers have significant hydrophobic regions and high crystallinity with extensive hydrogen bonding, which give good environmental stability and mechanical properties. The biocompatibility of silk products varies, largely because of the varying levels of nonfibroin components such as the sericin. When used as a suture material, silk elicits a greater inflammatory response than do most synthetic polymers. Proteases such as chymotrypsin can cleave proteins to peptides, especially in amorphous regions. Various silks have found utility in tissue engineering applications because they are often able to support cell growth [70]. Sponges made by freeze-drying or porogen leaching techniques are easily produced and give good porosity, although the precise design of architecture is difficult. Fibers may be prepared by electrospinning, although reproducibility is problematic. Self-assembled Peptides An increasingly important class of hydrogels for regenerative medicine is those made from self-assembled peptides [72]. These are polypeptides that assemble under specific conditions to form nanoscale structures. One prominent example is the class of self-assembled peptides made from amphiphilic molecules, derived from polypeptides linked to a polycarbon chain. The polypeptide region is typically hydrophilic whereas the hydrocarbon chain is hydrophobic. They can self-assemble into rod structures because of the arrangement of the hydrophobic regions as well as the charge shielding of the hydrophilic end groups by ionic molecules in the solution. These molecules can be decorated with functional groups to facilitate cellular adhesion and signaling. A number of other self-assembling peptides have been produced with advantages such as the ease in which gels are formed and functionalization. The significance of these engineered peptide hydrogels is that they epitomize this direction toward materials that can replicate cell niches, referred to earlier as the most important specification for tissue engineering templates. Peptide materials can be designed at a molecular level to bestow combined structural and biological activity characteristics that start to address these niche characteristics. These engineered, self-assembled peptides contain relatively short chains of amino acids. Through the careful choice of amino acid monomer sequences, the peptides can fold into secondary structures such as b-sheets, which themselves 646 36. Sericin can also be fabricated into different biomaterials such as scaffolds, films, hydrogels, nanofibers, and particles. Images courtesy of Professor Kundu, Indian Institute of Technology Kharagpur, India. These fibrous hydrogels replicate the required cell niches far better than do other materials. It is possible that such structures may be reinforced by other nanoscale structures to give robust templates. Several forms of self-assembled peptides have reached advanced stages of development, with good biocompatibility and degradation properties and without immunogenicity [72]. For example, templates consisting of alternating amino acids that contain 50% charged residues may be prepared. Such peptide structures support the cell attachment of a variety of mammalian cells. It is recognized that the chemicals used in preparing hydrogels may have some toxicity, and care has to be taken if the degree of conversion is not 100%; initiators, organic solvents, stabilizers, emulsifiers, unreacted monomers, cross-linking agents, and other substances have to be considered in this light and such chemicals may need to be removed. Synthesis typically should be followed by purification processes such as solvent washing or dialysis. When any of the materials are derived from natural sources, they may carry the risk of batch-to-batch variation, which also has to be taken into account. Synthetic hydrogels have some important advantages over natural biopolymer-based hydrogels, including easier large-scale production and fine-tunable and consistent properties. However, many are made using harsh synthetic chemistry, which requires care to ensure that contaminants and unreacted reagents present during synthesis are then removed.