Karela
General Information about Karela
One of the main advantages of Karela is its capacity to handle diabetes. Studies have shown that it can help in reducing blood sugar ranges and enhance insulin sensitivity. This is as a result of bitter gourd contains a compound called polypeptide-p, which has an insulin-like impact on the physique. This makes Karela a secure and pure alternative to traditional diabetes medication.
Apart from these, Karela has also been discovered to have anti-cancer properties. It accommodates compounds which have the potential to forestall the growth and spread of most cancers cells. Some studies have additionally shown that Karela may help in lowering the risk of certain forms of cancer, such as breast, prostate, and colon most cancers.
Karela can also be recognized for its digestive benefits. It helps in maintaining a wholesome intestine by selling the production of digestive enzymes and reducing irritation. Regular consumption of this vegetable also can help in bettering digestion and relieving constipation.
Karela is a pure and herbal formulation that is loaded with important nutrients, minerals, and nutritional vitamins. It is wealthy in iron, magnesium, and vitamin C, making it a strong ingredient to spice up immunity. This vegetable can additionally be known to have antioxidant, anti-inflammatory, antibacterial, and antiviral properties.
Unlike many different medications, Karela is a natural and protected choice for managing various health circumstances. It doesn't have any recognized unwanted facet effects, making it appropriate for individuals of all ages. However, it's always advisable to consult a physician before adding Karela to your food plan, especially if you're on any medicine.
Karela, also called bitter gourd or bitter melon, is a vegetable that is extensively used in many conventional cuisines. It is a popular vegetable in India, China, and different Asian nations. However, it's not solely recognized for its unique style and texture but additionally for its quite a few health benefits. In latest years, Karela has gained a lot of consideration for its potential use in managing diabetes, selling weight loss, and bettering overall health. Let us explore extra about this bitter vegetable and its benefits.
Another notable benefit of Karela is its impact on pores and skin health. It is rich in antioxidants and vitamin C, which are important for sustaining healthy and youthful-looking pores and skin. It might help in lowering acne, improving skin texture, and preventing untimely aging.
In conclusion, Karela is a vegetable with a bitter but powerful punch. It is not only full of important nutrients but also has quite a few well being benefits. From managing diabetes to promoting weight loss, this vegetable has proven promising results in bettering total well being. So, subsequent time you come across this bitter vegetable, do not let its style discourage you. Embrace it as a natural and natural approach to enhance your well being.
Moreover, Karela has been discovered to be beneficial in promoting weight reduction. It is a low-calorie and nutrient-dense vegetable, making it a wonderful meals alternative for these trying to lose weight. It additionally contains compounds that can assist in reducing urge for food and cravings, making it easier to stick to a nutritious diet.
In the late 1970s symptoms nausea headache fatigue discount generic karela canada, it was demonstrated in animal models that removal of mature T lymphocytes from the graft obtained from mismatched marrow allowed successful reconstitution upon injection into lethally irradiated recipient animals. In the case of mismatched transplantation, bone marrow cells are usually T cell depleted in vitro (see below); stem cells are then enumerated and injected intravenously. In this case, stem cells can also be purified by positive selection (see below), enumerated, and injected. Whenever sufficient compatibility is identified between a patient and stored cord blood, the latter is thawed and injected into the recipient without further manipulation. More recently, in vitro expansion of cord blood stem cells, and transplantations with multiple cord blood units, have been attempted to overcome this limitation. Bone marrow stem cells are most commonly obtained by multiple aspirations along the iliac crests, usually while the donor is under general anesthesia. In the past, the method of soybean lectin agglutination and E-rosetting was frequently used. With this method, soybean lectin allowed agglutination of the majority of mature marrow cells, which were removed by sedimentation. Further depletion of T lymphocytes was achieved by rosetting with sheep erythrocytes (E-rosetting technique) and density gradient centrifugation. Importantly, T-cell depletion by soybean lectin agglutination and E-rosetting maintains all immature marrow cells in the final preparation. T-cell depletion can also be achieved by incubation of bone marrow with monoclonal antibodies (mAbs) to T lymphocytes plus complement. In general, the donor is represented by one of the parents, since the volume of bone marrow that can be collected is much higher than it would be if a haploidentical sibling were to serve as donor. Methods for T-cell depletion of the bone marrow include use of soybean lectin agglutination and E-rosetting, depletion with monoclonal antibodies (mAbs), and positive selection of stem cells. However, the volume of cord blood is limited, so its use is mainly restricted to young patients. However, the probability of finding a suitable donor is lower for selected ethnic or racial groups that are poorly represented among volunteer donors. However, the number of cells contained in any defined unit is still a major limitation of cord blood. Finally, the leukopenia predisposes the patient to an increased risk of life-threatening bacterial or fungal infections. The frequency and severity of these complications depend on the type of transplant, the possible use of a conditioning regimen, and specific considerations related to the underlying disorder and to the clinical status of the recipient before transplantation. However, infants and children with preexisting organ damage are highly sensitive to the toxic effects of drugs. In the most severe cases, leakage of intravascular fluids into the interstitium (so-called third space filling) leads to generalized edema. These clinical manifestations include skin changes (scleroderma-like lesions, hyperpigmentation, hyperkeratosis, skin atrophy, ulcerations), tissue fibrosis and limitation of joint motility, fibrosis of exocrine glands ("sicca syndrome"), fibrosis of lungs and liver, increased susceptibility to infections, immune dysregulation, and autoimmunity. Newer regimens substitute another calcineurin inhibitor, tacrolimus, for cyclosporine. Systemic steroids have been shown to improve survival, but at the risk of significant adverse effects. Extracorporeal photopheresis can be used with the goal to induce tolerance; typically, its benefits, if present, are delayed until 23 months after initiation of treatment. Filtering of blood derivatives removes leukocytes and thus reduces the risk of transfusion-associated infections. Bacterial infections are usually amenable to successful treatment, if the pathogen is identified, and appropriate and aggressive use of antibiotics is initiated. Cyclophosphamide can cause hemorrhagic cystitis, a syndrome of inappropriate antidiuretic hormone secretion, or more rarely, cardiac disturbances. Delayed or incomplete tooth eruption is also a possible consequence of conditioning regimens. Effects on final height and growth, as well as long-term neurocognitive effects, are emerging as more children are treated and followed up. Therefore no chemotherapy is required in these patients in order to achieve T-cell reconstitution following stem cell transplantation. The quality and the kinetics of T-cell reconstitution following stem cell transplantation depend on the type of transplant. Consequently, following haploidentical transplantation, there is a prolonged period during which the recipient remains lymphopenic and at high risk of infections. Furthermore, donor-derived lymphoid progenitor cells have a striking advantage for in vivo T-cell differentiation. Consequently, use of pretransplantation chemotherapy and immune suppression is not required to attain T-cell reconstitution. Although use of conditioning chemotherapy carries the risk of drug-related toxicity, it favors the engraftment of donor-derived stem cells and may lead to a better recovery of humoral immunity and of improved thymopoiesis. The decline of T-cell function that is observed at 10 years or more after transplantation remains a concern and may cause clinical problems. Therefore there is a need for improvements in the procedures used to facilitate and sustain stem cell engraftment and/or to boost donorderived immunity. Reduced-intensity conditioning regimens have been often used in these patients, in the attempt to reduce the risks of drug-related toxicity. Transplantation of hematopoietic stem cells and long-term survival for primary immunodeficiencies in Europe: entering a new century, do we do better The kinetics of T-lymphocyte reconstitution differs substantially, depending on the type of transplant.
Giant cell arteritis: epidemiological clues to its pathogenesis and an update on its treatment medications 8 rights karela 60caps purchase online. Selective up-regulation of the soluble pattern-recognition receptor pentraxin 3 and of vascular endothelial growth factor in giant cell arteritis: relevance for recent optic nerve ischemia. Investigational analysis reveals a potential role for neutrophils in giant-cell arteritis disease progression. Correlation of interleukin-6 production and disease activity in polymyalgia rheumatica and giant cell arteritis. Treatment of giant cell arteritis: interleukin-6 as a biologic marker of disease activity. Regulation of inflammation and angiogenesis in giant cell arteritis by acute-phase serum amyloid A. Activation of arterial wall dendritic cells and breakdown of self-tolerance in giant cell arteritis. Trapping of misdirected dendritic cells in the granulomatous lesions of giant cell arteritis. The immunopathology of giant cell arteritis: diagnostic and therapeutic implications. Correlation of the topographical arrangement and the functional pattern of tissue-infiltrating macrophages in giant cell arteritis. Distinct vascular lesions in giant cell arteritis share identical T cell clonotypes. How does previous corticosteroid treatment affect the biopsy findings in giant cell (temporal) arteritis Treatment of giant cell arteritis using induction therapy with high-dose glucocorticoids: a double-blind, placebo-controlled, randomized prospective clinical trial. Recent advances in the clinical management of giant cell arteritis and Takayasu arteritis. Infliximab for maintenance of glucocorticosteroid-induced remission of giant cell arteritis: a randomized trial. Adjunctive methotrexate for treatment of giant cell arteritis: an individual patient data meta-analysis. A 27-year old female presents with a 6-weeks history of intermittent fever, arthralgias and weight loss. She should be scheduled for temporal artery biopsy, to rule out giant cell arteritis. Autoinflammation is a term that has been used since the late 1990s to illustrate the difference between autoimmune disorders and diseases characterized by exuberant inflammation. Typically, autoinflammatory diseases do not show features of excess adaptive immune system activation, and autoantigens or auto-antigen specific T-cells are not present in these diseases. It is now recognized that autoinflammation and autoimmunity form two ends of a spectrum of inappropriate immune system activation and share several common features. For many of the recently described autoinflammatory diseases, no genetic cause has been found yet. It has also become clear that autoinflammation is at least partially involved in the pathogenesis of other, more common diseases, such as gout, Crohn disease, and ulcerative colitis. Their pathophysiological mechanisms are understood to a much higher degree than in many newer autoinflammatory diseases, and their clinical presentations have been described precisely. The cornerstone of diagnosing an autoinflammatory disease is the clinical assessment of the patient. This includes a detailed medical and family history and direct observation of an inflammatory episode. The first step in the diagnostic process is to exclude other more common causes of recurrent inflammation, including infections, malignancy and paraneoplastic phenomena, and autoimmune disease. It is most common in individuals originating from around the Mediterranean basin, such as Turks, Jews (primarily non-Ashkenazi), Arabs, and in Armenians. Over 200 patients have now been identified, most of Western European and Caucasian ancestry. This could be partly explained by increased awareness for this disease among physicians in that part of the world. Disease awareness and recognition among clinicians have improved because of the availability of effective treatment for this disease. Schnitzler syndrome, first described by the French dermatologist Schnitzler in 1972,7 is an acquired autoinflammatory disorder with a median age of onset of 51 years. Typically, attacks are characterized by abrupt onset of high fever, peaking soon after onset and lasting for 12 hours to 3 days. The pain, which is caused by sterile peritonitis, may initially be focal and progress to more diffuse pain. At surgery, intraabdominal adhesions, a result of recurrent peritonitis, may be found. Pleuritis, presenting as thoracic pain, is experienced by approximately 40% of patients. Synovitis with monoarthritis of knee, ankle, or wrist occurs in one-half to three-quarters of patients. Emotional stress or menstruation may increase the frequency of attacks; some patients are able to report specific triggers for their attacks. Attacks may be as frequent as 23 times each month and as rare as less than once a year. The most consistent finding is that carriers of the M694V/ M694V genotype have more severe disease, with earlier onset and higher frequency of arthritis and long-term complications. There is no genotypephenotype association, suggesting a role for other yet undiscovered disease modifying factors. It is characterized by recurrent urticaria-like rash, arthralgia, myalgia, headache, and fever.
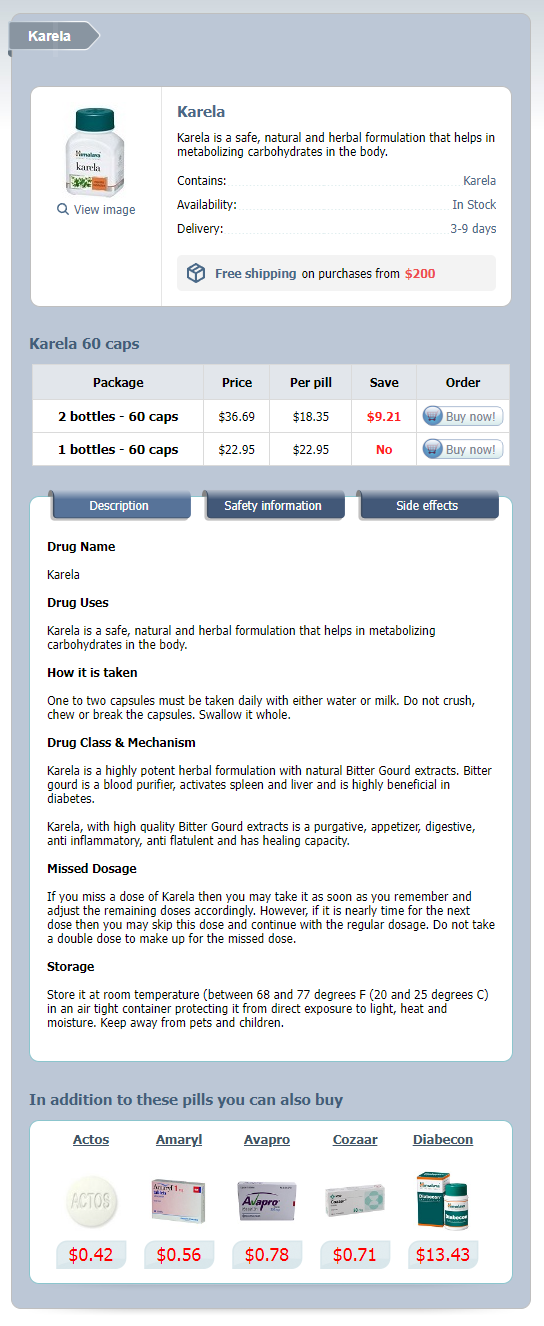
Karela Dosage and Price
Karela 60 caps
- 2 bottles - $36.69
- 1 bottles - $22.95
Studies also indicated that opioid use disorder is associated with white matter (and gray matter) changes in brain regions implicated in addiction including 258 Addiction and Substance Use Disorders those involved in the regulation of affect and impulse control treatment solutions discount karela 60caps, as well as in reward and motivational functions (Upadhyay et al. Collectively, these findings suggest that addiction is associated with significant reductions in white matter and future research is needed to better understand the molecular changes that lead to these reductions. Receptors and Transporters In addition to changes synaptic plasticity, dendritic morphology, and gray and white matter, addiction and substance use disorder is associated with changes in presynaptic transporters and postsynaptic receptors. For example, several studies have found decreased density of postsynaptic dopamine receptors (D2) in participants with substance use disorder relative to controls, however, studies have been mixed with respect to density of dopamine transporter proteins. Results revealed decreased levels of D2 receptors in individuals with alcohol use disorder relative to controls; however, no differences were found in the density of dopamine transporters. Other neuroimaging and postmortem studies have reported mean density of the dopamine transporters naturally decline with age in control participants relative to those with alcohol use disorder (Tupala et al. Still other studies have reported lower dopamine transporter density in participants with substance use disorder relative to controls (Tiihonen et al. Collectively, these studies implicate the D2 receptor in the pathophysiology of alcohol use disorder; however, questions remain regarding the role of dopamine transporter proteins. With regard to other substance use disorders, including cocaine and opioids, studies have been mixed with some reporting reduced dopamine receptor and transporter density in the striatum of participants addicted to opioids or stimulants while others have not (Cosgrove et al. The authors interpreted the findings as supporting that dysfunction of the dopaminergic system is a common mechanism underlying the alterations of reward processing observed in patients with mental health disorders. Chang, Alicata, and Volkow (2007) concluded that the majority of studies found reduced dopamine transporter density and reduced dopamine D2 receptors in the striatum of participants addicted to methamphetamine. Collectively, current findings support involvement of the dopamine transporter and postsynaptic receptors in addiction; however, questions remain regarding the extent of their involvement across addictive substances. In addition, it is important to note that other neurotransmitter receptors and transporters. Glial Cells As discussed in previous chapters, astrocytes are the most abundant glial cell type in the central nervous system and administration of cocaine, amphetamines, and psychostimulants has been found to induce activation of astrocytes. Morphological changes in the end feet of astrocytes that connect with blood vessels have also been found with drug administration, leading to reductions in fluids and other substances passing from the blood supply to the astrocytes (Fan et al. Functional changes in other types of glial cells have more recently been implicated in addition, including microglia and oligodendrocytes (McCarthy et al. Specifically, with repeated drug exposure, neurons adapt over time, and these cellular changes are believed to be responsible for tolerance, addiction, and withdrawal (Volkow, et al. A number of studies have reported that substance disorder is associated with a number of internal structural changes including a significant decrease in the amount of neurofilament proteins (GarciaSevilla et al. Neurofilament proteins are the major components of the neuronal cytoskelton and are important in maintaining the structure of the cell and the transport of substances from the soma to the terminal button. These same intracellular changes are associated with other drugs of abuse such as cocaine, methamphetamine, and alcohol (Wille-Bille et al. For example, when the mu receptor is occupied by opiates, the conductance of the K+ channels is increased, and second-messenger systems are activated. When the second-messenger system is activated, a cascade of events occurs, the details of which are not fully understood. One example is the increased production of the transcription factors dynorphin and delta FosB. Dynorphin levels have been found to increase with chronic drug use and are associated with the decreased rewarding effects of drugs and tolerance (Kreek et al. Another intracellular protein, delta FosB, also increases with chronic drug use and levels remain elevated after prolonged abstinence. These prolonged changes in delta FosB activity are associated with increased sensitivity to environmental cues and the rewarding effects of drugs and likely contribute to drug craving and relapse (Nestler, Barrot, & Self, 2001). An additional effect of chronic exposure to drugs is a decreased sensitivity of neuron receptors to the drug, which means larger amounts of the drug are required to achieve a desired effect (tolerance). In summary, addictive drugs are believed to produce complex, long-lasting intracellular changes that are associated with drug tolerance, dependence, and withdrawal. It is important to note, however, that the majority of molecular and intracellular studies concerning addiction are based on other animal models and questions arise concerning the generalization and application of these findings to humans. Physiological Changes Associated With Drug Tolerance Copyright Blausen Medical Communications. Detoxification options include abrupt cessation of the opiate ("cold turkey"), tapering with other drugs used to minimize withdrawal symptoms, pharmacological substitution. Rapid detox involves a medical procedure designed to avoid the physiological discomfort associated with withdrawal. Specifically, rapid detox requires hospitalization and the administration of general anesthesia. Rapid detox programs vary with respect to length of hospital stay, safety, cost, pre-evaluation measures, follow-up interventions, and the actual detox method. According to McCabe (2000), a typical detox procedure lasts from 4 to 6 hours and following the procedure patients are technically detoxified from the opiate. To reduce cravings and the likelihood of relapse, an opiate antagonist is generally prescribed for several weeks to a year post-detox. Although rapid detox is a method that avoids the distressing effects of withdrawal, it is an invasive procedure that carries all the risks associated with general anesthesia. In addition, rapid detox is a medical procedure and psychological treatment is often needed to address the emotional and behavioral aspects of addiction. Unfortunately, little empirical information is available concerning the long-term safety and efficacy of rapid detox relative to other treatment methods for opioid addiction and studies that are available or not encouraging. Rabinowitz, Cohen, and Atias (2002), for example, compared the relapse rates of 30 opiatedependent individuals who underwent rapid detox and a 9-month, follow-up course of naltrexone and a similar group of opiate-dependent individuals who detoxified in a 30-day inpatient program and did not receive naltrexone. Result indicated that 34% of the subjects overall relapsed within 13 months of detox and there was no significant difference in relapse rates between the two groups. More research is needed to understand the benefits and limitations of rapid detoxification as a treatment approach to opioid use disorder (Praveen et al.