Keflex
General Information about Keflex
Keflex works by interfering with the formation of the bacterial cell wall, causing it to weaken and eventually rupture. This results in the dying of the micro organism and permits the physique's pure immune system to fight off the an infection. Unlike some other antibiotics, Keflex isn't effective towards viral infections such as the frequent chilly or flu.
One of the primary uses of Keflex is to deal with infections of the higher respiratory tract, together with sinusitis, tonsillitis, and bronchitis. It is also commonly used to deal with ear infections, attributable to bacteria such as Streptococcus pneumoniae or Staphylococcus aureus. Keflex is also effective in treating skin infections, such as cellulitis, impetigo, and wound infections. In addition, it's typically prescribed for urinary tract infections attributable to E.coli or other bacteria.
In conclusion, Keflex is a broadly used antibiotic that's efficient in treating a range of bacterial infections. Like all medications, it should be taken as directed and solely used when prescribed for a bacterial infection. While there are potential side effects, they are normally delicate and may be managed by consulting a healthcare professional. When used appropriately, Keflex could be a useful software in fighting bacterial infections and selling overall well being.
The dosage and length of treatment for Keflex will vary relying on the sort and severity of the infection. It is on the market in numerous types, including tablets, capsules, and oral suspension, and is normally taken two to four times a day. It is essential to complete the complete course of remedy as prescribed, even if signs enhance, to ensure that the infection is totally eradicated.
In addition to potential unwanted aspect effects, the overuse or misuse of antibiotics can contribute to the event of antibiotic-resistant micro organism. It is important to only use Keflex when prescribed by a doctor for a bacterial an infection, and to by no means share your treatment with others. It can additionally be important to comply with good hygiene practices to stop the spread of bacteria.
As with any treatment, there are potential unwanted effects associated with Keflex. These can embrace nausea, diarrhea, upset stomach, and allergic reactions. It is essential to seek the assistance of a health care provider if any unwanted effects are skilled, as they could point out an allergy or a more serious opposed reaction.
Keflex should not be utilized by individuals with a identified allergy to cephalosporins or penicillin. It can also be essential to tell your doctor of another drugs you take, as Keflex may interact with sure drugs, together with blood thinners and oral contraceptives.
Keflex, also called cephalexin, is a commonly prescribed antibiotic that's used to treat a wide range of bacterial infections. It is part of a category of antibiotics called cephalosporins, which are comparable in structure to penicillin. Keflex is out there as a generic and beneath model names similar to Biocef, Daxbia, and Keflet.
It belongs to a class of antibiotics called cephalosporins, and is intently associated to different drugs on this class similar to Ceftin and Rocephin.
A 50% reduction in the dose is recommended for serum bilirubin concentrations of 1 virus del papiloma humano order keflex with a mastercard. Acute shortness of breath and bronchospasm can occur when vincristine or vinblastine is given in conjunction with mitomycin C. Because asparaginase may impair the hepatic clearance of vincristine, it is preferable to administer the vincristine 12 to 24 hours before L-asparaginase. Vincristine may decrease the absorption and plasma levels of orally administered drugs such as digoxin. Dilantin may increase the cytotoxicity of vincristine in multidrug-resistant tumor cells; however, this remains to be demonstrated in the clinic. When concurrently administered, erythromycin may increase the toxicity of vinca alkaloids, especially vinblastine. Therapeutic Indications in Hematology: the vinca alkaloids are among the most important drugs in the treatment of hematologic malignancies. Preparation and Administration: Vincristine is commercially available in 1-, 2-, and 5-mg vials. Vincristine is a powerful vesicant that should be administered only intravenously into a freely running infusion of normal saline or dextrose solution. In case of extravasation, infusion should be discontinued and any residual drug aspirated through the line. The manufacturer also recommends infiltrating the area with 1 to 2 mL of hyaluronidase, 150 U/ mL, and then applying warm compresses for 72 hours to facilitate dispersion of the drug. Vinblastine is commercially available as a lyophilized powder and a 1-mg/mL solution in 10-mg vials. The lyophilized drug is reconstituted by adding sodium chloride for injection (which may be preserved with either phenol or benzyl alcohol) to the 10-mg vial. Administration of vinblastine should follow the same guidelines described for vincristine. Similar to other vinca alkaloids, it also binds to tubulin, inhibits microtubule assembly, and produces a mitotic arrest of cells. These occur at concentrations that relatively spare axonal microtubules, which may reduce neurotoxicity. Peripheral neurotoxicity usually manifests as sensory impairment, decreased deep tendon reflexes, and paresthesias. Less commonly, severe painful dysesthesias, ataxia, foot drop, and cranial nerve palsy. Autonomic neurotoxicities include constipation, abdominal cramps, and ileus, which infusions of 30 mg/m2 produce peak plasma concentrations approximately 1. Rapid (<5 minutes) and (49-168 minutes) half-lives result in a rapid decline in the plasma concentration in the first hour posttreatment followed by a prolonged terminal half-life of 18 to 49 hours, reflecting slow efflux from the peripheral compartment. The major site of metabolism is the liver, with 33% to 80% of the drug excretion in feces and approximately 20% in urine. Preparation and Administration: Vinorelbine is available for injection in single use as 10 mg/mL in 1- or 5-mL vials without preservatives. Preparation and Administration: Paclitaxel is available as a Toxic Effects: Vinorelbine shares many of the principal toxicities of vinblastine. Myelosuppression is dose limiting but not cumulative, with nadirs occurring 7 to 10 days after administration. Because of lower affinity for axonal versus spindle microtubules, neurotoxicity is less prominent with vinorelbine. Mild to moderate peripheral neuropathy and constipation occur in approximately 30% of patients, and the incidence of neuropathy increases with the duration of treatment. Among the miscellaneous side effects noted are chest pain with or without electrocardiographic changes (6%, most with underlying cardiac disease), as well as bronchospasm and dyspnea (5%). Docetaxel for injection is available as a concentrate in polysorbate 80 in two vial contents (23. Adding diluent that is 13% (w/w) ethanol in water for injection to the concentrate produces a final premix concentration of 10 mg docetaxel/mL. After binding to the N-terminal 31 amino acids of the -tubulin subunit in the tubulin oligomers or polymers, these taxanes kinetically stabilize microtubule dynamics at plus ends. They also decrease the lag time and shift the equilibrium toward tubulin polymerization into microtubule bundles. The disequilibrium of tubulinmicrotubule polymerization results in mitotic arrest and apoptosis of cells. Depending on the dose and schedule, peak plasma concentrations of paclitaxel range between 0. Its steady-state volume of distribution ranges between 48 and 182 L/m2, with rapid uptake in almost all tissues except the central nervous system and 98% plasma protein binding. This means that paclitaxel dose escalation in shorter schedules may result in disproportionate increases in area under the concentrationtime curve and peak plasma concentration. Total fecal and urinary excretion of paclitaxel and its metabolites is approximately 70% and 10%, respectively. Although dose modification is not necessary for renal insufficiency, a 50% reduction in dose is recommended even for moderate hyperbilirubinemia or significant elevations in hepatocellular enzymes. The drug or its metabolites also have high fecal (80%) and low urinary elimination (5%). Neutropenia is the main toxicity of paclitaxel and docetaxel, but it is not cumulative. With higher doses of paclitaxel (250 mg/m2 over 24 hours), this can be ameliorated with subsequent administration of granulocyte colony-stimulating factor. Symmetric, distal, peripheral sensory neuropathy is usually seen with higher doses or multiple doses of paclitaxel.
Spicules from an aspirate may be surprisingly cellular in some patients despite overall marrow hypocellularity as most patients will have residual pockets of ongoing hematopoiesis standard antibiotics for sinus infection purchase 250 mg keflex. The risk of morbidity and mortality from aplastic anemia correlates best with the severity of the cytopenias rather than bone marrow cellularity. D: High-power view of bone marrow from patient in C showing small blast population. After stabilization of the patient, blood products should be used judiciously to prevent cardiopulmonary compromise and to reduce the risk of hemorrhage; a platelet goal of 10,000/mL will suffice for most patients, although some patients will tolerate even lower platelet goals without bleeding or petechiae. However, for patients with absolute neutrophil counts that are consistently <200mL, prophylaxis with oral antibiotics, such as a quinolone and a triazole antifungal, is reasonable. Patients with febrile neutropenia should be treated promptly with broad-spectrum antibiotics; in patients with persistent fever after the initiation of antibacterial antibiotics, aspergillus coverage should be added. Alternative regimens using fludarabine, cyclophosphamide and antithymocyte globulin are increasingly being used. Growth Factors Hematopoietic growth factor deficiency (such as erythropoietin, granulocyte colony-stimulating factor, thrombopoietin, or granulocytemonocyte colony-stimulating factor) is not responsible for the bone marrow failure in aplastic anemia; levels of measurable hematopoietic growth factors are markedly elevated in aplastic anemia patients in a compensatory attempt to increase blood production. Hematopoietic growth factors are often used after immunosuppressive therapy or high-dose cyclophosphamide therapy to accelerate hematopoietic recovery, but their use has not been shown to improve survival. DeFinitiVe tReAtment Nonsevere (Moderate) aplastic anemia There are limited data on the long-term prognosis of patients with moderate aplastic anemia. Although moderate aplastic anemia can progress, many patients will remain stable for years, and some may spontaneously improve, even in the absence of specific treatment. Thus, bone marrow transplantation from unrelated or mismatched donors is usually reserved for patients who fail to respond to one or more courses of immunosuppressive therapy. The best results with unrelated and mismatched transplants are seen in patients under 21 with disease duration of less than 1 year. The probability of graft failure was 20% and the survival probability at 5 years was less than 40%. At 10 years, the overall actuarial survival, response rate, and event-free survival was 88%, 71%, and 58%, respectively, for the 44 treatment-naïve patients. Relapse occurred in just 2 of the treatmentnaïve patients, one of whom was retreated with high-dose cyclophosphamide into a second complete remission. Despite the high response rate and low risk of relapse and secondary clonal disease, many investigators are unwilling to accept the relatively long period of aplasia associated with this therapy. Additional large series and/or future randomized trials will be necessary to fully define the role of this promising therapy. Interestingly, 10-year survival (84%) in patients with autologous recovery was equivalent or better than in patients who engrafted (74%). The major mechanism of cyclophosphamide detoxification appears to be inactivation of aldophosphamide by cellular aldehyde dehydrogenase to form the inert compound, carboxyphosphamide. High-dose cyclophosphamide is therefore highly immunosuppressive, but not myeloablative, allowing endogenous hematopoietic stem cells to reconstitute hematopoiesis. However, no stopping rules were met, and there were no statistical differences in response rate, survival, or secondary clonal disorders. They reported a 70% response rate with immunosuppressive therapy and an 88% overall survival at 10 years. Careful monitoring of liver function tests and vigilance for other hepatic complications (adenomas, tumors, etc. Haploinsufficiency of telomerase reverse transcriptase leads to anticipation in autosomal dominant dyskeratosis congenita. Aplastic anemia in rural Thailand: its association with grain farming and agricultural pesticide exposure. A single point mutation leading to loss of catalytic activity in human thiopurine S-methyltransferase. Results of transplanting bone marrow from genetically identical twins into patients with aplastic anemia [see comments]. Suppression of erythroid-colony formation by lymphocytes from patients with aplastic anemia. Bone marrow and peripheral blood lymphocyte phenotype in patients with bone marrow failure. T cells selectively infiltrate bone marrow areas with residual haemopoiesis of patients with acquired aplastic anaemia. Interferon-gamma gene expression in unstimulated bone marrow mononuclear cells predicts a good response to cyclosporine therapy in aplastic anemia. Diazepam-binding inhibitor-related protein 1: a candidate autoantigen in acquired aplastic anemia patients harboring a minor population of paroxysmal nocturnal hemoglobinuria-type cells. Quantitative analysis of cobblestone area-forming cells in bone marrow of patients with aplastic anemia by limiting dilution assay. Complete remission in acquired severe aplastic anemia following high-dose cyclophosphamide. Multilineage glycosylphosphatidylinositol anchor deficient hematopoiesis in untreated aplastic anemia. Myelodysplastic syndrome and acute myelogenous leukemia as a late clonal complication in children with acquired aplastic anemia. Narrative review: paroxysmal nocturnal hemoglobinuria: the physiology of complement-related hemolytic anemia. Clinical significance of a minor population of paroxysmal nocturnal hemoglobinuria-type cells in bone marrow failure syndrome. Genetic defects underlying paroxysmal nocturnal hemoglobinuria that arises out of aplastic anemia. Paroxysmal nocturnal hemoglobinuria clones in severe aplastic anemia patients treated with horse antithymocyte globulin plus cyclosporine. Natural history of paroxysmal nocturnal hemoglobinuria clones in patients presenting as aplastic anemia.
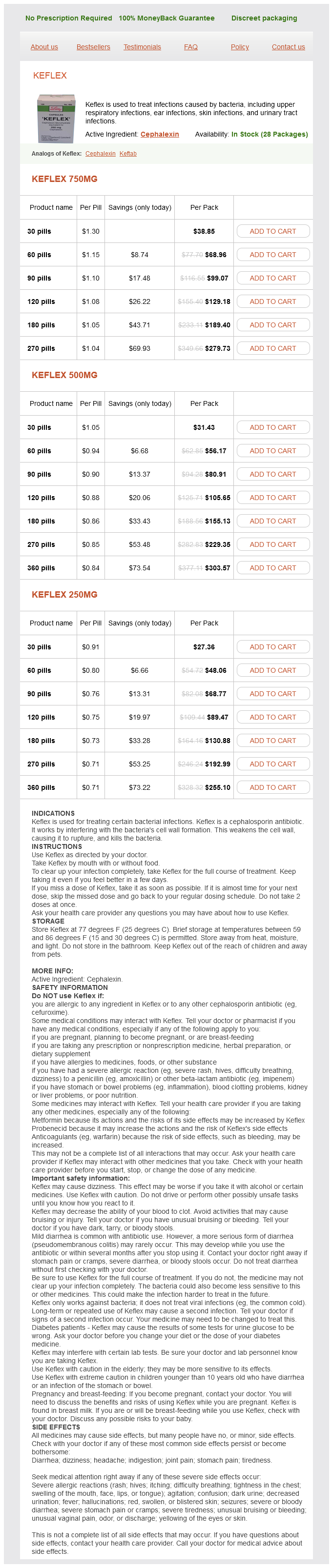
Keflex Dosage and Price
Keflex 750mg
- 30 pills - $38.85
- 60 pills - $68.96
- 90 pills - $99.07
- 120 pills - $129.18
- 180 pills - $189.40
- 270 pills - $279.73
Keflex 500mg
- 30 pills - $31.43
- 60 pills - $56.17
- 90 pills - $80.91
- 120 pills - $105.65
- 180 pills - $155.13
- 270 pills - $229.35
- 360 pills - $303.57
Keflex 250mg
- 30 pills - $27.36
- 60 pills - $48.06
- 90 pills - $68.77
- 120 pills - $89.47
- 180 pills - $130.88
- 270 pills - $192.99
- 360 pills - $255.10
Etoposide must be administered slowly over more than 30 minutes to prevent hypotension xeloda antibiotics discount generic keflex uk. Etoposide phosphate is available commercially as single-dose vials containing etoposide phosphate equivalent to 100 mg of etoposide. When it is diluted with water, 5% dextrose, or normal saline to a concentration of 10 to 20 mg/mL, it can be administered without dilution over 5 to 10 minutes. When reconstituted, etoposide phosphate is stable for 24 hours at room temperature or under refrigeration. Currently, no oral preparation is available in the market; however, for investigational purposes, each 50-mg vial may be dissolved in 50 to 100 mL of syrup or juice. To achieve optimal absorption, a single oral dose of 60 mg/m2, which may be repeated at 6-hour intervals, is advised. It is rapidly metabolized in the liver, where approximately 25% of the drug concentrates and has a half-life of 20 to 50 hours. The principal metabolite is daunorubicinol, which also displays antineoplastic activity. Biliary excretion accounts for approximately 75% of the drug and metabolite elimination. Patients with significant hepatic dysfunction should receive an attenuated dose of daunorubicin. Preparation and Administration: Daunorubicin is supplied with 100 mg of mannitol in 20-mg vials, from which it is Chapter 55 Pharmacology and Molecular Mechanisms of Antineoplastic Agents for Hematologic Malignancies 831 reconstituted with 4 mL of sterile water for injection. In the event of extravasation, as much infiltrated drug as possible should be aspirated from the tissue, and cold compresses should be maintained on the site for several hours. The patient should be informed that daunorubicin may impart a red color to the urine for up to 72 hours after administration. Erythematous streaking along the vein is often an indication that the administration rate is too rapid. The drug is a powerful vesicant, and in case of extravasation, the measures described for daunorubicin should be followed. It is important to emphasize that weekly low-dose regimens or administration by continuous infusion can decrease the risk of cardiotoxicity with doxorubicin. Toxic Effects: Myelosuppression, predominantly leukopenia, is Potential Drug Interactions: When used in combination with the dose-limiting toxic effect. Erythematous streaking near the site of injection occurs as a benign local allergic reaction and should not be confused with extravasation. Cardiac toxicity is a unique characteristic of the anthracycline antibiotics and can be acute or chronic. Transient reduction in the ejection fraction can also occur acutely and is often associated with pericarditis (pericarditis-myocarditis syndrome). The chronic form of anthracycline cardiac toxicity is related to the cumulative dose. The dose limit of doxorubicin is generally considered to be 450 to 500 mg/m2, where the risk of clinical cardiotoxicity is between 1% and 10%. The cardiac toxicity is clinically characterized by congestive heart failure, usually refractory to medical therapy. Cardiac irradiation or the administration of cyclophosphamide may increase the risk of cardiotoxicity. The cardioprotective agent dexrazoxane (Zinecard) is now available and recommended to be started at a doxorubicin cumulative dose greater than 350 mg/m2. Barbiturates may increase the plasma clearance of doxorubicin and decrease its cytotoxic effect. Therapeutic Indications in Hematology: Doxorubicin is one of the most important drugs in the treatment of hematologic malignancies. Absorption, Fate, and Excretion: the elimination half-life of Potential Drug Interactions: Daunorubicin is not physically the parent compound is 11. The oral bioavailability of this drug is approximately 30%; 80% of the drug is excreted in the urine as 13-epirubicinol. The drug interactions described for doxorubicin (description follows) probably occur with daunorubicin as well. Doxorubicin (Adriamycin) Chemistry and Mechanism of Action: Doxorubicin is also an anthracycline glycoside antibiotic. It differs from daunorubicin at C-8, in which a hydroxyacetyl group replaces an acetyl group. Toxic Effects: the side effects of idarubicin are similar to those of daunorubicin and doxorubicin but are of lesser intensity at equal myelosuppressive doses. Absorption, Fate, and Excretion: Doxorubicin has a triphasic plasma clearance with a half-life of approximately 30 hours. The drug is extensively metabolized in the liver to yield an active metabolite (doxorubicinol) and a number of inactive metabolites (aglycones). Within 7 days, more than 50% of an injected dose is excreted in the bile, but only 5% to 10% of the drug is excreted in the urine. Mitoxantrone (Novantrone) Chemistry and Mechanism of Action: Mitoxantrone is a synthetic anthracenedione. Its reduced potential for free radical formation may explain the decreased cardiotoxicity of this drug. Preparation and Administration: Doxorubicin is commercially available in vials of 10, 20, 50, 150, and 200 mg. The lyophilized powder is reconstituted with either normal saline or sterile water for injection to yield a 2-mg/mL solution.