Labetalol
General Information about Labetalol
Labetalol can be used in the remedy of preeclampsia, a situation that occurs during pregnancy and is characterised by hypertension and increased protein within the urine. It is normally a life-threatening condition if left untreated. Labetalol is secure to make use of throughout pregnancy and is often thought of the first-line treatment for preeclampsia.
It is essential to take labetalol precisely as prescribed and to not stop taking it without consulting a physician. Suddenly stopping labetalol can lead to a fast enhance in blood stress and different critical side effects. It can additionally be important to avoid consuming alcohol whereas taking labetalol, as it could enhance the sedative results of the treatment.
In abstract, labetalol is a generally prescribed medication for the therapy of high blood pressure. Its capacity to lower blood strain, control irregular coronary heart rhythms, and its safety in being pregnant make it a flexible and essential medicine in the management of various circumstances. However, as with every medication, it's essential to make use of labetalol under the steerage and supervision of a doctor to make sure correct dosing and monitoring of potential unwanted side effects.
One of the main makes use of of labetalol is in the management of hypertension, or hypertension. This situation affects tens of millions of people worldwide and is a major risk issue for serious health problems corresponding to coronary heart attack, stroke, and kidney disease. Labetalol works by blocking the beta receptors within the coronary heart and blood vessels, which reduces the heart price and relaxes the blood vessels, allowing blood to flow more simply and lowering blood pressure.
Labetalol, also known by its model name Trandate, is a medication commonly used for the treatment of high blood pressure. It belongs to a class of medications known as beta-blockers, which work by blocking the effects of the hormone epinephrine, also called adrenaline. This ends in the dilation of blood vessels and a decrease in heart price, ultimately resulting in a lower in blood stress.
Like any medication, labetalol might cause some unwanted effects. The most common unwanted aspect effects embody dizziness, fatigue, nausea, and headache. Other much less widespread unwanted side effects could embrace gradual coronary heart rate, low blood pressure, and shortness of breath. It is necessary to speak to a healthcare supplier if any of these side effects turn into severe or bothersome.
In addition to its results on blood strain, labetalol also has antiarrhythmic properties, meaning it helps to control abnormal coronary heart rhythms. This makes it a helpful treatment for people with certain kinds of irregular heartbeats.
Labetalol should be used with caution in folks with asthma, diabetes, coronary heart failure, and certain forms of circulation problems. It can also interact with different medicines, so you will want to inform the physician or pharmacist of all the medicines being taken, including over-the-counter medicine, vitamins, and dietary supplements.
Labetalol is often taken orally within the type of tablets, and the dose might vary depending on the individual's situation and response to remedy. It is normally really helpful to take labetalol twice a day, and it can be taken with or without food. In some cases, labetalol could additionally be given as an intravenous injection in a hospital setting for folks with severe hypertension or preeclampsia.
The most common type of pulsion diverticula is an epiphrenic diverticula blood pressure of 90/60 labetalol 100 mg order overnight delivery, which is located near the diaphragmatic hiatus. About 80% of epiphrenic diverticula are associated with esophageal motility disorders such as achalasia or distal esophageal spasm, which are discussed in Chapter 43. Endoscopic techniques are suitable for patients with medium-sized diverticula (2 to 5 cm). The diverticuloscope provides visualization of the lumen of the esophagus and diverticulum and the septum between them. The septum is then divided and stapled with 2 rows of staples on each side of the division line. The Zenker diverticulum must be at least 3 cm in length to be able to seat an adequate length of the stapler. Modifications of the stapler and other techniques may improve results in short diverticula. In a review of rigid endoscopic treatment of Zenker diverticulum, combining 11 studies of 494 patients, the median initial success rate was 95%, with a 4% rate of conversion to open surgery, a 3% rate of major morbidity, with recurrence of symptoms in 5% over a median follow-up of 16 months. In a review of 20 studies of flexible endoscopic treatment of 813 patients with Zenker diverticula, the initial success rate was 91%, with an 11% adverse event rate, and an 11% recurrence rate after a median of 23 months of follow-up. When symptoms occur, the most common are dysphagia, food regurgitation, reflux, weight loss, and chest discomfort. An epiphrenic diverticulum may be mistaken for a diaphragmatic hernia or duplication cyst on chest radiography. Diagnosis is best made by barium swallow, which serves to visualize the diverticulum and localizes it more precisely than endoscopy It must be understood that the symptoms are usually related to the underlying motility disorder and not the diverticulum itself. Therefore, treating the underlying condition, usually with myotomy, is the key component of the surgery. To prevent gastroesophageal reflux after myotomy, a partial posterior (Toupet) or anterior (Dor) fundoplication may be performed. They are thought to be acquired and are often associated with conditions that cause chronic esophageal inflammation. The esophageal pseudodiverticula are localized in most cases but are diffusely scattered throughout the esophagus in 40% of cases. Complications Squamous cell carcinoma has been reported in epiphrenic diverticula. Only patients with symptoms clearly related to their diverticula should be treated. It can be difficult to pass a manometry catheter beyond the diverticulum and into the stomach, but documentation of achalasia or distal esophageal spasm is helpful for guiding treatment. Given the high prevalence of associated motility disorders such as achalasia, esophageal myotomy is performed in most cases. A, Endoscopic view of a large esophageal diverticulum with food and liquid (arrows). C, Laparoscopic resection of a large diverticulum (arrows) of the esophagus (arrowheads). Tiny openings of the pseudodiverticula are seen in this patient, who also has a distal esophageal peptic stricture. This wide-mouthed diverticulum (arrows) was seen on a retroflexed view of the cardia. In addition, 57% required repeat dilation due to recurrence of dysphagia symptoms. Epidemiology, Etiology, and Pathophysiology Gastric diverticula are found in only 0. These are most often located near the gastroesophageal junction on the posterior aspect of the lesser curvature. Intramural or partial gastric diverticula are formed by projection of the stomach mucosa through the muscularis. Gastric diverticula have been reported as a complication of obesity surgery, particularly from vertical banded gastroplasty, although they have also been seen after Roux-en-Y gastric bypass. A clear association with a specific symptom complex should be firmly established before considering resection, because more common diagnoses If a patient with a juxtacardiac diverticulum is referred for surgery, it may be prudent to place an endoscopic tattoo near the diverticulum, to assist with localization during surgery. Laparoscopic diverticulectomy can be used for simple resections for symptoms or perforation. Proximal diverticula near the esophagogastric junction are handled with care to avoid narrowing this area with the stapler. Clinical Features and Diagnosis Juxtacardiac diverticula are almost always asymptomatic. Rarely, patients may complain of pain or dyspepsia attributable to a diverticulum. The combination of air and fluid leads the radiologist to consider a pancreatic abscess in the differential. Resection of duodenal diverticula should never be performed for vague abdominal complaints. Bleeding, diverticulitis, and perforation are the most common problems associated with duodenal diverticula. Endoscopic control of bleeding from diverticula has been accomplished using various techniques, including bipolar cautery, epinephrine injection, and hemoclips. Many patients with duodenal perforation or diverticulitis undergo surgery for diagnosis and treatment including drainage and resection of the involved diverticulum, if feasible.
In addition 1 discount labetalol 100 mg online, the risk of gastric bleeding or perforation during chemotherapy is lower than 5% and only a few of those who bleed require urgent gastrectomy. Retrospective studies have shown similar outcomes in patients treated with surgery alone versus chemotherapy alone. Whether the treatment included surgery was left to the discretion of each participating center. Thus, standard management of gastric large B cell lymphoma follows standard management of nodal large B cell lymphomas. This regimen is primarily based on retrospective data, which shows increasing numbers of complete remissions achieved with this regimen and patients achieving complete remission having the best chance of long-term disease-free survival. Although durable remissions are being seen with this treatment, long-term data on treatment outcomes is being discerned. However, the developing consensus seems to favor combined chemotherapy and radiation and avoidance of surgery (see text). Uncommon Gastric Lymphomas B cell lymphomas other than marginal zone or diffuse large B cell may involve the stomach uncommonly T cell lymphomas of the small intestine are usually enteropathy-type intestinal T cell lymphomas; other forms of T cell lymphoma have been rarely reported. Patients may present with abdominal pain, weight loss, obstruction, abdominal mass, bleeding, and/or perforation. Approximately half of patients have localized disease, and half have disease spread to regional or distant nodes. Prognosis depends on disease stage and patient factors, such as age and performance status. Patients typically present with widespread adenopathy and frequently have bone marrow and extranodal involvement. The disease usually presents as a single annular or exophytic tumor,124 which may be present anywhere in the small intestine; disease is usually confined to the intestine or to local nodes. Some patients have received chemotherapy, but few data are available regarding regimens and outcome. It should be noted that in nodal marginal zone lymphoma, chemotherapy is usually reserved for patients with symptoms, because the disease is slow-growing and sensitive to chemotherapy, but not curable by it. As in gastric marginal zone B cell lymphoma, the small intestinal variety may have varying components of large cell transformation. Additional synchronous and metachronous lesions were present or later developed in the ileum and the duodenum, as well as the rectum and sigmoid colon. B, Low-power photomicrograph of ileum shows multiple discrete sites of mucosal and submucosal involvement by lymphomatous polyposis. Neoplastic lymphoid follicles are evident, involving the wall of the small intestine and effacing the normal architecture (Hematoxylin and eosin, low power). The disease is characterized by t(14;18)(q24;q32), a translocation that results in overexpression of the bcl-2 gene. Chemotherapy and radiation are sometimes indicated for the management of this indolent but incurable disorder. Due to the excellent prognosis (median survival >12 years) associated with this disorder, most experts recommend a "wait and watch" strategy to management. Burkitt tumor cells are monomorphic, medium-sized cells with round nuclei, multiple nucleoli, and basophilic cytoplasm. The involved lymphoid tissue microscopically has a starry sky appearance caused by numerous benign macrophages that have ingested apoptotic tumor cells. Most cases have a translocation of the c-myc gene on chromosome 8, either to the immunoglobulin heavy-chain region on chromosome 14 or to one of the immunoglobulin light-chain regions on chromosomes 2 or 22, resulting in a t(8;14), t(2;8), or t(8;22) translocation. The disease is characterized by t(11;14)(q13;q32), a translocation that results in rearrangement and overexpression of the bcl-1 gene encoding the protooncogene cyclin D1. As noted, patients with this diagnosis may also present with the gross appearance of multiple lymphomatous polyposis. A diagnosis in North America or Europe should be questioned, unless the patient has previously lived in an endemic area. The disease occurs in individuals with lower socioeconomic status who live in conditions of poor hygiene and sanitation. This loss of antigen dependence is associated with the development of more aggressive clinical features. Pathology Gross lesions are generally confined to the proximal small intestine, with adenopathy of adjacent mesenteric nodes. Although grossly only the proximal bowel wall is involved, histologically the disease is characterized by a dense mucosal and submucosal cellular infiltrate that extends continuously throughout the length of the small intestine. However, as already noted, various studies assessing immunoglobulin gene rearrangements or light chain restriction have suggested that even the earliest infiltrate is monoclonal. This early infiltrate broadens villi and shortens and separates crypts, but epithelial cells remain intact. A histologic variant, the follicular lymphoid type, has been described in some patients This variant features a diffuse involvement of the mucosa, with lymphoid follicle-like structures. As the disease progresses to intermediate and late stages, the villi are further broadened and may become completely effaced, crypts are fewer, and the immunoproliferation extends more deeply. Atypical lymphoid cells infiltrate the benign-appearing plasma cells and lymphoplasmacytic cells. Mesenteric lymph nodes are enlarged in early lesions, with preserved architecture, although follicles may be encroached on by a histologically benign-appearing lymphocytic or plasmacytic infiltrate. As the disease progresses, the lymph node may acquire a more dysplastic appearance. Centrocyte-like cells proliferating deeper in the mucosa have mainly cytoplasmic chain protein. It is likely that these centrocyte-like cells, stimulated by microbial antigens, differentiate into the plasma cells that secrete the chain protein characteristic of the disease.
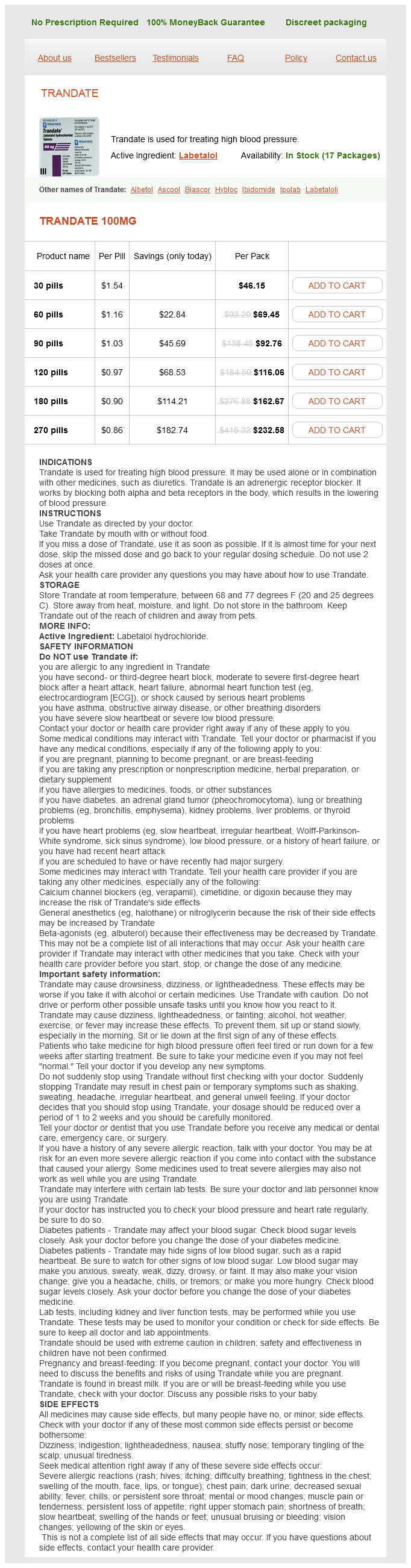
Labetalol Dosage and Price
Trandate 100mg
- 30 pills - $46.15
- 60 pills - $69.45
- 90 pills - $92.76
- 120 pills - $116.06
- 180 pills - $162.67
- 270 pills - $232.58
Another study attempted to estimate intraobserver variability by submitting 51 pancreatograms to 4 expert endoscopists on 3 separate occasions arteria axilar order labetalol 100 mg with visa. These features may be individually classified as none, minimal, moderate, or extensive but in practice are generally only graded as present or absent, and the total number of features is used as the score. The sensitivity and specificity of the test is determined by the threshold total score used to define chronic pancreatitis. Most studies have used the presence of 3 or more features to define a positive result. In the Rosemont system, the diagnostic strata are as follows: Most consistent with chronic pancreatitis 1 Major A feature and 3 minor features or 1 Major A feature and 1 Major B feature or 2 Major A features 1 Major A feature and <3 minor features or Major B feature and 3 minor features or 5 minor features 3-4 minor features or Major B feature with <3 minor features 2 minor features Suggestive of chronic pancreatitis Indeterminate for chronic pancreatitis Normal through expert consensus and includes major and minor criteria, with an attempt to provide semi-quantification of severity. Initial studies of these new criteria have not documented improvements in interobserver agreement or test accuracy. In a subgroup with more advanced histologic evidence of chronic pancreatitis by histology, the sensitivity was 83% and specificity 80%. In the analysis, more than half of those with a normal Rosemont score had histologic evidence of chronic pancreatitis, whereas 80% of those with "indeterminate" features had chronic pancreatitis, and almost all of those with "suggestive" features had chronic pancreatitis. The agreement between these tests varies widely in these studies, ranging from 10% to 90%. The edema associated with a recent episode of acute pancreatitis can make duct margins and intralobular septa more apparent, which will reduce specificity. The initial evaluation of pain should focus on identifying associated conditions for which specific therapy exists. These conditions can include pancreatic pseudocyst, duodenal (and possibly bile duct) compression, superimposed pancreatic carcinoma, and gastroparesis. Cross-sectional imaging can be helpful in identifying some of these complications in addition to assessing for alternative diagnoses that might mimic chronic pancreatitis. Identifying patients with a dilated pancreatic duct is useful in differentiating those patients who are most likely to benefit from endoscopic or surgical therapy. Very few randomized trials, and even fewer placebocontrolled trials of therapy for pain exist, so the evidence base supporting most interventions is quite weak. The markers on the dilated pancreatic duct demonstrate hyperechoic margins, one of the diagnostic features of chronic pancreatitis. The parenchyma surrounding these markers demonstrates hyperechoic strands and foci, additional features of chronic pancreatitis. Medical Therapy Analgesics the majority of patients with chronic pancreatitis require some form of analgesia. The risk of addiction is not defined and is estimated to be about 10% to 30%,147 but may be higher. Efforts to minimize narcotic use are appropriate, but narcotics should not be withheld in patients with severe pain. Strategies to minimize the risk of overuse of narcotics and addiction include having a single physician take responsibility for prescriptions, ongoing counseling, monitoring of prescriptions, and regular clinic visits. Pain management clinics that focus on non-narcotic approaches are most useful in patients with chronic pancreatitis. If non-narcotic agents fail, it is appropriate to begin with lowerpotency opioid agents like tramadol. Tramadol is a dual-action analgesic, with mu-opioid agonistic and monoaminergic properties. High dosages of tramadol are equivalent to oral morphine in treating chronic pancreatitis, with fewer effects on gut motility. Adjunctive agents can also be considered in patients who need more potent narcotics. Many of these patients are depressed, and coexistent depression lowers pain threshold. Chronic pancreatic pain can lead to abnormal spinal cord gating in nociceptive neurons, a centrally sensitized pain state, with hyperalgesia and allodynia. In one randomized trial in patients with chronic pancreatitis requiring narcotics for pain control, pregabalin reduced chronic pancreatitis unlikely. In the subgroup with suspected exocrine or endocrine insufficiency, the disease is likely to be long-standing, and most available diagnostic tests will be able to detect this relatively far-advanced disease. Because other conditions may mimic chronic pancreatitis (pancreatic malignancy, intraductal papillary mucinous neoplasms, cystic neoplasms) a high-quality cross-sectional imaging test is necessary to rule out these other possible diseases. If the diagnosis remains in doubt, follow-up over time with periodic re-assessment may be the only diagnostic approach. New diagnostic biomarkers are needed, and large studies are underway to identify predictors of the development of chronic pancreatitis and its complications. The other adjunctive agents have not been rigorously studied, but they are commonly used in patients with continued severe pain from chronic pancreatitis, in an attempt to improve pain control and minimize the dosage and potency of narcotics. Given the increasing recognition of neuropathic mechanisms of pain in chronic pancreatitis using these types of agents appears reasonable. Cessation of Alcohol and Tobacco Continued alcohol abuse hastens the development of pancreatic dysfunction in patients with chronic pancreatitis, although even complete abstinence does not prevent progression. Most studies, but not all, have documented an apparent decrease in pain or painful relapses in patients who stop drinking alcohol. In a summary of these studies, pain continued in 26% of abstinent patients, compared with 53% of those who continued to drink. Cessation of smoking appears to have even more benefits, in both preventing tobacco-induced illness and in reducing the risk of secondary pancreatic carcinoma. Antioxidants Damage by free radicals is one mechanism for pancreatic damage in alcoholic and other forms of chronic pancreatitis. Patients with chronic pancreatitis (particularly alcoholic) have evidence of oxidant stress and reduced antioxidant capacity. This trial recruited subjects who were relatively young, underweight, and suffered from mainly idiopathic or tropical pancreatitis.