Lagevrio
General Information about Lagevrio
These promising outcomes prompted Merck to request emergency use authorization from the us Food and Drug Administration (FDA). In October 2021, the FDA granted emergency use authorization for Lagevrio for the treatment of mild to moderate COVID-19 in adults who are at high threat for extreme disease or hospitalization. This authorization marks a big step forward in the fight towards COVID-19, as it is the first oral antiviral drug accredited to be used in treating the virus.
One of the major benefits of Lagevrio is its technique of administration. Being an oral drug, it can be easily taken at house, making it a extra convenient possibility for patients than different treatments, such because the monoclonal antibody infusion therapy, which requires sufferers to go to a healthcare facility to receive the remedy. Additionally, Lagevrio does not must be given early in the center of the an infection, as it works in any respect levels of the illness.
Despite its promising outcomes, Lagevrio nonetheless has its limitations. It will not be suitable for use in patients with extreme or critical COVID-19, as they may require more intensive treatments. Additionally, the drug is not recommended for use in pregnant or lactating ladies, in addition to patients with extreme liver or kidney issues. More analysis is required to grasp the potential side effects and long-term effects of Lagevrio.
The approval and availability of Lagevrio supplies a brand new tool in the fight towards COVID-19. It has the potential to alleviate the burden on hospitals and healthcare methods by providing a safe and effective therapy possibility for non-hospitalized patients. However, this does not mean that we should let our guard down. Vaccines stay the best method to forestall extreme sickness and death from COVID-19, and we should proceed to follow public well being tips corresponding to carrying masks and social distancing.
Lagevrio is an oral antiviral drug developed by the pharmaceutical firm Merck & Co. It was initially created to treat one other viral an infection, influenza, however has now been repurposed for COVID-19. The drug works by inhibiting the replication of the virus, preventing it from spreading and inflicting more harm to the physique.
In the face of a world pandemic, the development of Lagevrio is a big achievement. It is simply one of many ongoing efforts to seek out effective remedies for COVID-19. The approval of Lagevrio highlights the importance of research and collaboration in overcoming the challenges posed by the virus. Hopefully, with continued efforts and developments, we'll soon be ready to put an end to this pandemic.
The efficacy of Lagevrio isn't limited to treating the virus but in addition has shown potential in stopping the unfold of the virus. Recent research have shown that the drug can cut back the amount of virus particles in a affected person's saliva, doubtlessly decreasing their contagiousness and talent to spread the virus to others.
Since the beginning of the COVID-19 pandemic, scientists and researchers have been tirelessly working to search out an efficient remedy for the virus. One of the newest promising developments is the antiviral drug Lagevrio, also identified as Lagevrio, which has proven promising ends in its medical trials.
In preclinical studies, Lagevrio has shown exercise towards a broad range of viruses, including SARS-CoV-2, the virus responsible for COVID-19. This led to its analysis in a phase 2/3 scientific trial, which enrolled over 1,seven-hundred non-hospitalized adult patients with delicate to reasonable COVID-19 signs. The study confirmed that Lagevrio lowered the danger of hospitalization or dying by roughly 50% in comparability with placebo.
During insertion of a sigmoidoscope hiv infection emedicine discount 200 mg lagevrio fast delivery, the curvatures of the rectum and its acute flexion at the rectosigmoid junction have to be kept in mind so the patient does not undergo unnecessary discomfort. The operator must also know that the transverse rectal folds, which provide useful landmarks for the procedure, may temporarily impede passage of these instruments. Urinary bladder: the superior and inferior portions of the urinary bladder are quite distinct anatomically and functionally. Urethra: the male urethra consists of four parts, two of which are the intramural and prostatic parts. It is surrounded by the prostate, the muscular anterior "lobe" that includes the trough-like superior extension of the external urethral sphincter anteriorly, and by the glandular lobes posteriorly. It is firmly attached to and indents the anterior vaginal wall centrally and distally. Male Internal Genital Organs the male internal genital organs include the testes, epididymides (singular = epididymis), ductus deferentes (singular = ductus deferens), seminal glands, ejaculatory ducts, prostate, and bulbo-urethral glands. The testes and epididymides (described in Chapter 5, Abdomen) are considered internal genital 1396 organs on the basis of their developmental position and homology with the internal female ovaries. However, because of their external position postnatally and because in dissection these organs are encountered during the dissection of the inguinal region of the anterior abdominal wall, they are considered with the abdomen in Chapter 5. The genital organs are demonstrated: testis, epididymis, ductus deferens, ejaculatory duct, and penis, with the accessory glandular structures (seminal gland, prostate, and bulbo-urethral gland). The ductus deferens has relatively thick muscular walls and a minute lumen, giving it a cord-like firmness. During the pelvic part of its course, the ductus deferens maintains direct contact with the peritoneum; no other structure intervenes between them. The ductus crosses superior to the ureter near the posterolateral angle of the urinary bladder, running between the ureter and the peritoneum of the ureteric fold to reach the fundus of the bladder. The relationship of the ductus deferens to the ureter in the male is similar, although of lesser clinical importance, to that of the uterine artery to the ureter in the female. Posterior to the bladder, the ductus deferens at first lies superior to the seminal gland and then descends medial to the ureter and the gland. Here, the ductus deferens enlarges to form the ampulla of the ductus deferens before its termination. During development, as the testis descends inferiorly and laterally from its original position (medial to the site of the kidneys on the posterior abdominal wall) to and then through the inguinal canal, the ureter is crossed by testicular vessels in the abdomen and by the ductus deferens in the pelvis. The umbilical ligaments, like the urinary bladder, are embedded in extraperitoneal or subperitoneal fascia (mostly removed in this dissection). The ejaculatory ducts are formed by the merger of the duct of the seminal gland and the ductus deferens. The 1400 vestigial prostatic utricle, usually seen as an invagination in an anterior view, appears in this posterior dissection as an evagination lying between the ejaculatory ducts. The tiny artery to the ductus deferens usually arises from a superior (sometimes inferior) vesical artery. Veins from most of the ductus drain into the testicular vein, including the distal pampiniform plexus. They secrete a thick alkaline fluid with fructose (an energy source for sperms) and a coagulating agent that mixes with the sperms as they pass into the ejaculatory ducts and urethra. Pelvic part of ureters, urinary bladder, seminal glands, terminal parts of ductus deferens, and prostate. The left seminal gland and ampulla of the ductus deferens are dissected free and sliced open. The perineal membrane lies between the external genitalia and the deep part of the perineum (anterior recess of ischio-anal fossa). It is pierced by the urethra, ducts of the bulbo-urethral glands, dorsal and deep arteries of the penis, cavernous nerves, and the dorsal nerve of the penis. The superior ends of the seminal glands are covered with peritoneum and lie posterior to the ureters, where the peritoneum of the rectovesical pouch separates them from the rectum. The inferior ends of the seminal glands are closely related to the rectum and are separated from it only by the rectovesical septum. The duct of the seminal gland joins the ductus deferens to form the ejaculatory duct. The arteries to the seminal glands derive from the inferior vesical and middle rectal arteries. The ejaculatory ducts converge and open on the seminal colliculus by tiny, slit-like apertures on, or just within, the opening of the prostatic utricle. Although the ejaculatory ducts traverse the glandular prostate, prostatic secretions do not join the seminal fluid until the ejaculatory ducts have terminated in the prostatic urethra. The arteries to the ductus deferens, usually branches of the superior (but frequently inferior) vesical arteries, supply the ejaculatory ducts. The glandular part makes up approximately two thirds of the prostate; the other third is fibromuscular. The fibrous capsule of the prostate is dense and neurovascular, incorporating the prostatic plexuses of veins and nerves. All of this is surrounded by the visceral layer of the pelvic fascia, forming a fibrous prostatic sheath that is thin anteriorly, continuous anterolaterally with the puboprostatic ligaments, and dense posteriorly where it blends with the rectovesical septum. The anterior surface is separated from the pubic symphysis by retroperitoneal fat in the retropubic space. Although not clearly distinct anatomically, the following lobes of the prostate are traditionally described. Lobules and zones of prostate demonstrated by anatomical section and ultrasonographic imaging. The ducts of the glands in the peripheral zone open into the prostatic sinuses, whereas the ducts of the glands in the central (internal) zone open into the 1404 prostatic sinuses and the seminal colliculus. The isthmus of the prostate (commissure of prostate; historically, the anterior "lobe") lies anterior to the urethra.
During expiration hiv infection without ejaculation purchase lagevrio 200mg line, the right dome reaches as high as the 5th rib and the left dome ascends to the 5th intercostal space. The level of the domes of the diaphragm varies according to the phase of respiration (inspiration or expiration). The muscular part of the diaphragm is situated peripherally with fibers that converge radially on the trifoliate central aponeurotic part, the central tendon. The central tendon has no bony attachments and is 1253 incompletely divided into three leaves, resembling a wide cloverleaf. Although it lies near the center of the diaphragm, the central tendon is closer to the anterior part of the thorax. The surrounding muscular part of the diaphragm forms a continuous sheet; however, for descriptive purposes, it is divided into three parts, based on the peripheral attachments: Sternal part: consisting of two muscular slips that attach to the posterior aspect of the xiphoid process; this part is not always present. Costal part: consisting of wide muscular slips that attach to the internal surfaces of the inferior six costal cartilages and their adjoining ribs on each side; the costal parts form the right and left domes. Lumbar part: arising from two aponeurotic arches, the medial and lateral arcuate ligaments, and the three superior lumbar vertebrae; the lumbar part forms right and left muscular crura that ascend to the central tendon. The right crus, larger and longer than the left crus, arises from the first three or four lumbar vertebrae. Because it lies to the left of the midline, it is surprising to find that the esophageal hiatus is a formation in the right crus; however, if the muscular fibers bounding each side of the hiatus are traced inferiorly, it will be seen that they pass to the right of the aortic hiatus. The right and left crura and the fibrous median arcuate ligament, which unites them as it arches over the anterior aspect of the aorta, form the aortic hiatus. The medial arcuate ligament is a thickening of the fascia covering the psoas major, spanning between the lumbar vertebral bodies and the tip of the transverse process of L1. The lateral arcuate ligament covers the quadratus lumborum muscles, continuing from the L12 transverse process to the tip of the 12th rib. The superior aspect of the central tendon of the diaphragm is fused with the inferior surface of the fibrous pericardium, the strong, external part of the 1254 fibroserous pericardial sac that encloses the heart. Vessels and Nerves of Diaphragm the arteries of the diaphragm form a branch-like pattern on both its superior (thoracic) and inferior (abdominal) surfaces. The arteries supplying the inferior surface of the diaphragm are the inferior phrenic arteries, which typically are the first branches of the abdominal aorta; however, they may arise from the celiac trunk. Some veins from the posterior curvature of the diaphragm drain into the azygos and hemi-azygos veins (see Chapter 4, Thorax). The veins draining the inferior surface of the diaphragm are the inferior phrenic veins. The lymphatic plexuses on the superior and inferior surfaces of the diaphragm communicate freely. The anterior and posterior diaphragmatic lymph nodes are on the superior surface of the diaphragm. Lymph from these nodes drains into the parasternal, posterior mediastinal, and phrenic lymph nodes. Lymphatic vessels from the inferior surface of the diaphragm drain into the anterior diaphragmatic, phrenic, and superior lumbar (caval/aortic) lymph nodes. Lymphatic capillaries are dense on the inferior surface of the diaphragm, constituting the primary means for absorption of peritoneal fluid and substances introduced by intraperitoneal (I. Lymphatic vessels are formed in two plexuses, one on the superior surface of the diaphragm and the other on its inferior surface; the plexuses communicate freely. The phrenic nerves supply all of the motor and most of the sensory innervation to the diaphragm. The lower six or seven intercostal and subcostal nerves provide sensory innervation peripherally. The entire motor supply to the diaphragm is from the right and left phrenic nerves, each of which arises from the anterior rami of C3C5 segments of the spinal cord and is distributed to the ipsilateral half of the diaphragm from its inferior surface. Sensory innervation (pain and proprioception) to the diaphragm is also mostly from the phrenic nerves. Peripheral parts of the diaphragm receive their sensory nerve supply from the intercostal nerves (lower six or seven) and the subcostal nerves. Diaphragmatic Apertures the diaphragmatic apertures (openings, hiatus) permit structures (vessels, nerves, and lymphatics) to pass between the thorax and abdomen. Also passing through the caval opening are terminal branches of the right phrenic nerve and a few lymphatic vessels on their way from the liver to the middle phrenic and mediastinal lymph nodes. The esophageal hiatus also transmits the anterior and posterior vagal trunks, esophageal branches of the left gastric vessels, and a few lymphatic vessels. The fibers of the right crus of the diaphragm decussate (cross one another) inferior to the hiatus, forming a muscular sphincter for the esophagus that constricts it when the diaphragm contracts. In most individuals (70%), both margins of the hiatus are formed by muscular bundles of the right crus. In others (30%), a superficial muscular bundle from the left crus contributes to the formation of the right margin of the hiatus. Because the aorta does not pierce the diaphragm, movements of the diaphragm do not affect blood flow through the aorta during respiration. The aorta passes between the crura of the diaphragm posterior to the median arcuate ligament, which is at the level of the inferior border of the T12 vertebra. The aortic hiatus also transmits the thoracic duct and sometimes the azygos and hemi-azygos veins. This triangle transmits lymphatic vessels from the diaphragmatic surface of the liver and the superior epigastric vessels.
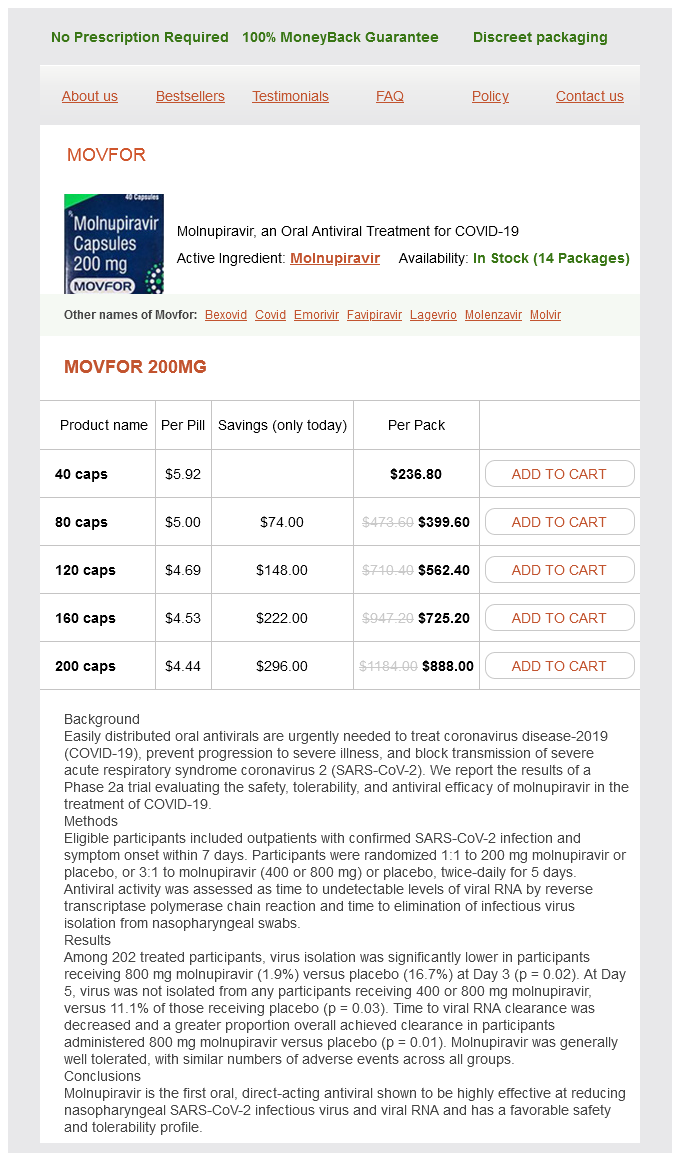
Lagevrio Dosage and Price
Movfor 200mg
- 40 caps - $236.80
- 80 caps - $399.60
- 120 caps - $562.40
- 160 caps - $725.20
- 200 caps - $888.00
Carotid/jugular blood vessels are the major structures commonly injured in penetrating wounds of the neck hiv infection chart buy lagevrio 200mg on line. The brachial plexuses of nerves originate in the neck and pass inferolaterally to enter the axillae and continue 2216 into and supply the upper limbs. In the middle of the anterior aspect of the neck is the thyroid cartilage, the largest of the cartilages of the larynx, and the trachea. These bones are parts of the axial skeleton except the clavicles, which are part of the appendicular skeleton. The 3rd6th vertebrae are "typical" cervical vertebrae; the 1st, 2nd, and 7th are "atypical. Typical cervical vertebra demonstrating a 2218 rectangular body with articular unci (uncinate processes) on its lateral aspects, a triangular vertebral foramen, a bifid spinous process, and foramina transversaria. The bony and cartilaginous landmarks of the neck are the vertebrae, mastoid and styloid processes, angles of the mandible, hyoid bone, thyroid cartilage, clavicle, and manubrium of the sternum. Cervical Vertebrae Seven cervical vertebrae form the cervical region of the vertebral column, which encloses the spinal cord and meninges. The transverse processes of all cervical vertebrae (typical or atypical) include foramina transversaria for the vertebral vessels (the vertebral veins and, except for vertebra C7, the vertebral arteries). The superior facets of the articular processes are directed superoposteriorly, and the inferior facets are directed inferoposteriorly. Their spinous processes are short and, in individuals of European heritage, bifid. The C1 vertebra or atlas: a ring-like, kidney-shaped bone lacking a spinous process or body and consisting of two lateral masses connected by anterior and posterior arches. The C2 vertebra or axis: a peg-like den (odontoid process) projects superiorly from its body. The vertebra prominens (C7): so-named because of its long spinous process, which is not bifid. Hyoid Bone the mobile hyoid bone (or simply, the hyoid) lies in the anterior part of the neck at the level of the C3 vertebra in the angle between the mandible and the thyroid cartilage. The hyoid is suspended by muscles that connect it to the mandible, styloid processes, thyroid cartilage, manubrium of the sternum, and scapulae. The hyoid is unique among bones for its isolation from the remainder of the skeleton. The U-shaped hyoid derives its name from the Greek word hyoeidçs, meaning "shaped like the letter upsilon," the 20th letter in the Greek alphabet. It is suspended from the styloid processes of the temporal bones by the stylohyoid ligaments. Functionally, the hyoid serves as an 2220 attachment for anterior neck muscles and a prop to keep the airway open. Its anterior convex surface projects anterosuperiorly; its posterior concave surface projects postero-inferiorly. Each end of its body is united to a greater horn that projects posterosuperiorly and laterally from the body. Each lesser horn is a small bony projection from the superior part of the body of the hyoid near its union with the greater horn. It is connected to the body of the hyoid by fibrous tissue and sometimes to the greater horn by a synovial joint. Cervical pain is usually affected by movement of the head and neck, and it may be exaggerated during coughing or sneezing, for example. Injuries of Cervical Vertebral Column Fractures and dislocations of the cervical vertebra may injure the spinal cord 2221 and/or the vertebral arteries and sympathetic plexuses passing through the foramina transversaria. Fracture of Hyoid Bone Fracture of the hyoid (or of the styloid processes of the temporal bone; see Chapter 8, Head) occurs in people who are manually strangled by compression of the throat. Inability to elevate the hyoid and move it anteriorly beneath the tongue makes swallowing and maintenance of the separation of the alimentary and respiratory tracts difficult and may result in aspiration pneumonia. Hyoid bone: Unique in terms of its isolation from the rest of the skeleton, the U-shaped hyoid is suspended between the body of the mandible superiorly and the manubrium of the sternum inferiorly. Cervical Subcutaneous Tissue and Platysma the cervical subcutaneous tissue (superficial cervical fascia) is a layer of fatty connective tissue that lies between the dermis of the skin and the investing layer of deep cervical fascia. The cervical subcutaneous tissue is usually thinner than in other regions, especially anteriorly. It contains cutaneous nerves, blood and lymphatic vessels, superficial lymph nodes, and variable amounts of fat. This transverse section of the neck passes through the isthmus of the thyroid gland at the C7 vertebral level, as indicated in part (A). The investing layer and its embedded muscles 2224 surround two main fascial columns. The pretracheal (visceral) layer encloses muscles and viscera in the anterior neck; the prevertebral (musculoskeletal) layer encircles the vertebral column and associated muscles. The fascial compartments of the neck are shown to demonstrate an anterior midline approach to the thyroid gland. Although the larynx, trachea, and thyroid gland are nearly subcutaneous in the midline, two layers of deep cervical fascia (the investing and pretracheal layers) must be incised to reach them. The thin platysma muscle spreads subcutaneously like a sheet, passes over the clavicles, and is pierced by cutaneous nerves. Its fibers arise in the deep fascia covering the superior parts of the deltoid and pectoralis major muscles and sweep superomedially over the clavicle to the inferior border of the mandible.