Lincocin
General Information about Lincocin
In conclusion, Lincocin is a potent antibiotic that's efficient against a broad vary of bacteria. Its ability to inhibit protein synthesis makes it a priceless choice in the remedy of infections attributable to gram-positive micro organism and penicillin-resistant strains. With proper use and monitoring, Lincocin can provide reduction and aid in the recovery of individuals suffering from bacterial infections.
One of the major benefits of Lincocin is its effectiveness towards penicillin-resistant bacteria. This is especially important in the treatment of infections attributable to Streptococcus pneumoniae, a standard bacterium that has developed resistance to many antibiotics. Lincocin has been shown to be effective in opposition to these resistant strains, making it a useful possibility within the therapy of these infections.
Like all antibiotics, Lincocin might cause side effects in some individuals. These can embody gastrointestinal symptoms such as nausea, vomiting, and diarrhea, in addition to allergic reactions. It is important to tell your physician should you experience any side effects while taking Lincocin.
Lincocin is an antibiotic that is produced by the bacteria Streptomyces lincolniensis. It is commonly used to deal with a wide range of bacterial infections due to its bacteriostatic effect. This means that it inhibits the growth and reproduction of micro organism, without destroying them fully.
In addition to its antibacterial properties, Lincocin additionally has anti-inflammatory results. This makes it a useful selection within the therapy of conditions corresponding to pimples, where inflammation is a distinguished feature. By reducing irritation, Lincocin may help to improve the symptoms related to such conditions and aid within the healing process.
Lincocin has a broad spectrum of exercise against a selection of micro organism, together with gram-positive cocci such as Streptococcus species (including Streptococcus pneumoniae), Haemophilus influenzae, Bacillus anthracis, Mycoplasma species, Bacteroides species, Corynebacterium diphtheriae, Clostridium perfringens, and Clostridium tetani. This big selection of protection makes it an effective choice for treating quite so much of infections caused by these micro organism.
The mechanism of motion of Lincocin entails the reversible binding to the 50S subunit of ribosomes in bacteria. Ribosomes are responsible for protein synthesis, and by binding to this subunit, Lincocin disrupts the formation of peptide bonds. This leads to the inhibition of bacterial protein synthesis, in the end preventing the growth and replication of micro organism.
Lincocin is available in various types, together with tablets, capsules, and injectable solutions. The dosage and period of therapy range relying on the kind and severity of the an infection being handled. It is essential to comply with the prescribing physician's directions and full the complete course of remedy to ensure the absolute best consequence.
A 90% reduction in oocyte formation still results in viable sporozoites and would allow for ongoing transmission symptoms 14 days after iui lincocin 500mg purchase on-line. Vaccines Vaccines have been promoted as the most cost-effective method to combat malaria, and efforts have been underway to develop a malaria vaccine for more than 50 years. The Plasmodium parasite has many adaptations to avoid the human immune system, several of which also increase the difficulty of designing an effective vaccine. Although the host is able to develop clinical immunity after multiple exposures and avoid severe disease, sterilizing immunity never develops naturally. Malaria vaccines can be divided into three categories, based on the life cycle of the antigen targeted: pre-erythrocytic, blood stage, or transmission blocking. Proof of principle for immunity against this stage of the parasite was provided more than 50 years ago when the bite of multiple mosquitoes infected with irradiated sporozoites proved to be protective against subsequent challenge. An alternate approach to irradiation is the genetic manipulation of the sporozoite, which also can limit the development of the sporozoite and may elicit different immune responses. The vaccine has been in development since the 1980s and was licensed in Europe in 2015. These vaccines would not prevent the initial liver-stage infection, but if completely effective could abort the infection by effecting the clearance of the erythrocytic phase. This would effectively block transmission, as gametocytes would not have the Plasmodium ovale P. The persistent, low-density parasitemia in otherwise healthy individuals may produce distinctive clinical features, or individuals may be so asymptomatic that they qualify as blood donors. Effect of transmission intensity on hotspots and micro-epidemiology of malaria in sub-Saharan Africa. Changes in the burden of malaria following scale up of malaria control interventions in Mutasa district, Zimbabwe. Factors determining the occurrence of submicroscopic malaria infections and their relevance for control. Malaria risk factors in Butajira area, south-central Ethiopia: a multilevel analysis. Resistance to malaria through structural variation of red blood cell invasion receptors. Microvascular sequestration of parasitized erythrocytes in human falciparum malaria: a pathological study. Malaria: mechanisms of erythrocytic infection and pathological correlates of severe disease. Epidemiology, pathophysiology, management and outcome of renal dysfunction associated with plasmodia infection. Sporadic human infections were the rule61 until a 2004 outbreak of "hyperparasitemic P. Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Clinical features and prognostic indicators in paediatric cerebral malaria: a study of 131 comatose Malawian children. Alterations in systemic extracellular heme and hemopexin are associated with adverse clinical outcomes in Ugandan children with severe malaria. Predicting the clinical outcome of severe falciparum malaria in African children: findings from a large randomized trial. Attributable fraction estimates and case definitions for malaria in endemic areas. Impact of introduction of rapid diagnostic tests for malaria on antibiotic prescribing: analysis of observational and randomised studies in public and private healthcare settings. Plasmodium ovale curtisi and Plasmodium ovale wallikeri circulate simultaneously in African communities. Meta-analysis: accuracy of rapid tests for malaria in travelers returning from endemic areas. Rapid immunochromatographic malarial antigen detection unreliable for detecting Plasmodium malariae and Plasmodium ovale. Safety of lumbar puncture in comatose children with clinical features of cerebral malaria. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Distinguishing malaria from severe pneumonia among hospitalized children who fulfilled integrated management of childhood illness criteria for both diseases: a hospital-based study in Mozambique. Postartesunate delayed hemolysis is a predictable event related to the lifesaving effect of artemisinins. Global extent of chloroquine-resistant Plasmodium vivax: a systematic review and meta-analysis. Effect of paracetamol on parasite clearance time in Plasmodium falciparum malaria. Febrile temperatures induce cytoadherence of ring-stage plasmodium falciparum-infected erythrocytes. Plasmodium malariae infection in an asymptomatic 74-year-old Greek woman with splenomegaly. Reactivation of Plasmodium malariae infection in a Trinidadian man after neurosurgery. Possible aetiological role of Plasmodium malariae in "nephrotic syndrome" in Nigerian children.
Humoral and cell-mediated immunity to the intracellular pathogen Francisella tularensis symptoms 4 dpo bfp purchase line lincocin. Histologic and molecular diagnosis of tularemia: a potential bioterrorism agent endemic to North America. Francisella tularensis Susceptibility to Antibiotics: A Comprehensive Review of the Data Obtained In vitro and in Animal Models. Bichat guidelines for the clinical management of tularaemia and bioterrorism-related tularaemia. Tularemia epidemic in northwestern Spain: clinical description and therapeutic response. Streptomycin and alternative agents for the treatment of tularemia: review of the literature. Carrier rates of over 50% have been measured in Norway rats, which shed massive numbers of organisms for life without showing clinical illness. For example, the serovar Icterohaemorrhagiae is primarily associated with the Norway rat, Canicola with dogs, and Pomona with swine and cattle. However, a particular host species may serve as a reservoir for one or more serovars, and a particular serovar may colonize different animal species. Transmission of infection from animal to human usually occurs through contact with contaminated water or moist soil. Organisms enter humans through abrasions of the skin or through the mucosal surface of the eye, mouth, nasopharynx, or esophagus. Crowded cities that are flood-prone and have large rat populations provide ideal conditions for disease transmission. Escalating migration of the rural poor to urban slums is likely to further exacerbate the risks of leptospirosis transmission. An outbreak in Nicaragua in 199512 and an urban epidemic in Salvador, Brazil, in 19995 were associated with particularly heavy rains and flooding. Special clinics to treat the disease were set up in evacuation centers, and an estimated 1. Intense exposure to leptospires has been documented in rice, sugar cane, and rubber plantation workers. Less frequently, leptospirosis is acquired by direct contact with the blood, urine, or tissues of infected animals. Measuring incidence by active surveillance confirms that leptospirosis is surprisingly common. Antibody positivity rates of 37% have been recorded in rural Belize, 23% in Vietnam, and 18% in inner city Baltimore, Maryland. Human leptospirosis is an important disease in China, Southeast Asia, India, Africa, and South and Central America. It is also of significance in eastern and southern Europe, Australia, and New Zealand. In the United States, the disease is primarily of veterinary importance, with only 50 to 150 human cases reported annually. In 1916 Inada isolated spirochetes in pure culture, subsequently delineated Leptospira, identified them as the etiologic agent of leptospirosis, and linked rats to disease transmission. This genus contains more than 35 species classified on the basis of comparative genomic analysis10,11 and more than 300 serovars based on diverse agglutinating lipopolysaccharide antigens. Leptospires colonize proximal renal tubules of mammalian hosts and are shed in the urine. They can survive for several months in the environment under moist conditions, particularly in the presence of warmth (above 22°C) and neutral pH (pH 6. These conditions occur all year round in the tropics but only during the summer and autumn months in temperate climates. It is unclear why renal failure predominates as the principal cause of death in some places, whereas pulmonary hemorrhage is the major cause in others, even where the most common infecting serovars are the same. Patients who survive severe leptospirosis have complete recovery of hepatic and renal function, consistent with the lack of structural damage to these organs. Subclinical infection is common, and less than 10% of symptomatic infections result in severe, icteric illness. Even relatively virulent serovars, such as Copenhageni/ Icterohaemorrhagiae, lead more often to anicteric than to icteric disease. Once symptoms develop, they may or may not follow a biphasic course; after an initial febrile illness there is defervescence and symptomatic improvement followed by a second period of disease refractory to antibiotics. However, a clear demarcation between the first and second stages may not be observed in icteric leptospirosis and, in mild cases, the distinction can be unclear or the second stage may never occur. The diagnostic usefulness of a history of a biphasic illness has been overemphasized. Conjunctival suffusion is a helpful diagnostic clue that usually appears 2 or 3 days after the onset of fever and involves the bulbar conjunctiva. Pus and serous secretions are absent, and there is no matting of the eyelashes and eyelids. Less common and less distinctive signs include pharyngeal injection, splenomegaly, hepatomegaly, lymphadenopathy, and skin lesions. Manifestations of the second stage are more variable and mild than those of the initial illness and usually last 2 to 4 days. Aseptic meningitis is the hallmark of this stage of leptospirosis but is not associated with mortality.
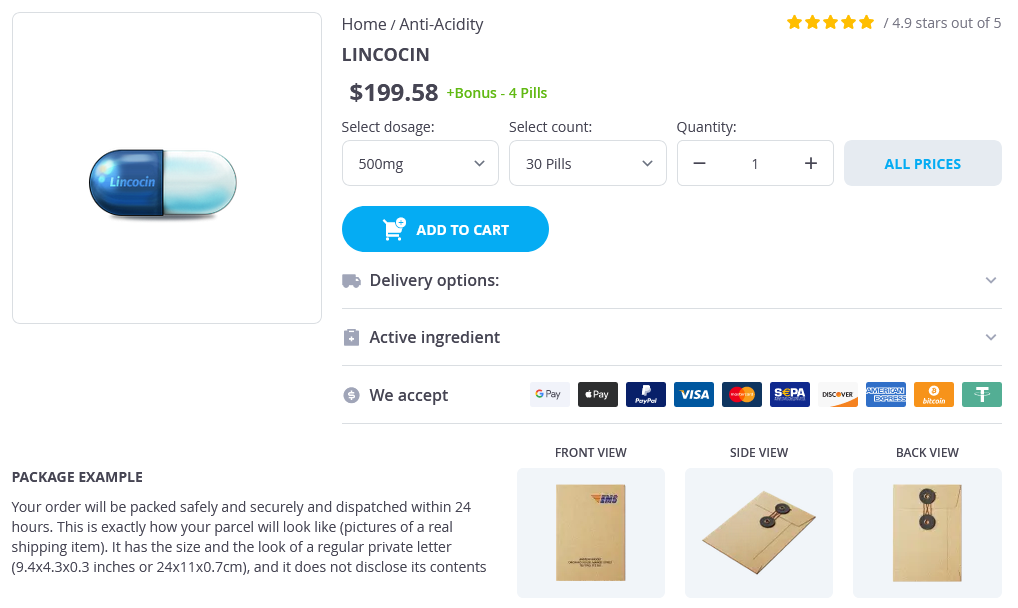
Lincocin Dosage and Price
Lincocin 500mg
- 30 pills - $221.76
- 60 pills - $310.46
Destruction of anatomic boundaries in treatment online 500mg lincocin order otc, marked enlargement of draining lymph nodes of the neck, and spread to distant sites are more typical of carcinomas and sarcomas. Meta-analysis: cysticidal drugs for neurocysticercosis: albendazole and praziquantel. Miltefosine:A review of its pharmacology and therapeutic efficacy in the treatment of leishmaniasis. With a median follow-up of 41 months, overallsurvivalat5yearswas59%anddisease-specificsurvival was73%. Locoregional recurrences develop in 30% to 40% of patients, distant metastases in 20% to 30%. Patients with recurrent small tumors, particularly of the larynx and nasopharynx, can be treated for cure with surgery or repeat irradiation. Effective post-operative rehabilitation will require a multi-disciplinary team of surgeons and other medical and allied medical specialists to restore function, manage infections, maintain nutrition, and enhance well-being. Diagnosticaccuracyoffine-needle aspiration cytology versus frozen section in solitary thyroid nodules. Concurrentchemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. Richard Coughlin in the availability of water and electricity, number of care providers. Significant costs are also imposed on the victims: direct and indirect costs for care and prolonged absence from gainful work can be ruinous for many poor families who are reliant on subsistence farming. Selling of vital assets, severe indebtedness, and removing children from school contribute to the vicious cycle of poverty. The management of injuries depends on type, site, and duration; whether there was prior treatment; the availability of local care providers, including surgeons and anesthesiologists; the presence of a safe surgical environment; and the availability of materials and supplies. Most fractures will heal with conservative management, although not always in the optimal position. Debridement and delayed closure of wounds, either primarily or by graft, are the norm. Pins can be inserted percutaneously, particularly if fluoroscopic imaging is available, to improve and stabilize reduction and then be incorporated in the cast. Skin traction in the pediatric group and skeletal traction in adults are still commonly used for femur fractures. Open reduction and internal fixation of long bone fractures has many advantages: earlier mobilization of the limb and of the patient, earlier return to home and to work, and better functional results with fewer complications such as non-unions or malunions. The biggest drawback is the risk of deep infection, which in orthopedics can be catastrophic, sometimes salvageable only with a life-saving amputation. A clean operating environment, skilled surgeon, trained personnel, adequate instrumentation, and safe anesthesia are prerequisites to perform safe internal fixation of fractures. The surgeon should weigh potential risks and benefits of surgical versus conservative management. Even technically successful procedures, such as repair of lacerated finger flexor tendons, can have disappointing results, as the outcome is largely dependent on availability of good post-operative rehabilitation programs. Improving health care, vaccines, and antibiotics have increased longevity contributing to age-related conditions such as osteoarthritis. In addition, non-communicable disease, such as diabetes, contribute to musculoskeletal conditions. Each section of this chapter addresses key aspects of epidemiology, pathophysiology, clinical investigation, diagnosis, management, and outcomes. This leads to many patients being seen late, with sequelae of neglected trauma such as non-unions or malunions, or even sequelae of treatment such as post-compartment syndrome contractures. The numbers of drivers, passengers, motorized vehicles, and kilometers of paved road are increasing globally, and so are the numbers of high-energy injuries (Table 13. Poor countries are often ill-prepared to manage this growing epidemic due to lack of pre-hospital care systems; deficiencies in infrastructure, human, technologic, and material capacities and resources; and absent or inadequate physical and social rehabilitation services. In poorer countries, lacerations or stab wounds by knife or machete are more common than gunshot wounds. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980 to 2015: a systematic analysis for the Global Burden of Disease Study 2015. Most wounds should be treated with a thorough debridement (sometimes called wound excision) and delayed closure or coverage. Work-related injuries are more common with economic development and industrialization. Safety laws may be absent or unenforced, and there is often no social safety net to help patients who cannot return to employment after their recovery from injury. Injuries to the spine, mostly from falls or crush accidents, and to the fingers and hands are particularly common and disabling. Economic development can also lead to more leisure time and an increase in sports-related injuries. Most soft tissue injuries, no matter how severe, are treated conservatively, and because rehabilitation services are often lacking, the results can be less than optimal. The provider must be aware of the prevalence and distribution of infections to facilitate diagnosis and treatment. Treatment is often empiric, based on the most likely pathogens, and adjusted according to clinical response. Osteomyelitis There are three ways in which bones can become infected: hematogenous dissemination of pathogens, a contiguous focus of infection. Any bone can be affected, but the femur and tibia account for around 50% of cases. As pressure builds up in the purulent material, the endosteal circulation is destroyed.