Linezolid
General Information about Linezolid
Linezolid works by binding to the bacterial ribosomes, which are answerable for protein synthesis. By blocking this course of, the bacteria are unable to develop and multiply, and finally die off. This mechanism of motion, coupled with its broad spectrum of activity, has made Linezolid a go-to medicine for many physicians when confronted with difficult-to-treat infections.
However, like all antibiotics, Linezolid does have its drawbacks. One main concern is the development of resistance. As with any antibiotic, the overuse or misuse of Linezolid can lead to the emergence of drug-resistant micro organism. This is why it is important to use this medicine only when prescribed by a healthcare skilled and to proceed the course of treatment as directed. Additionally, Linezolid can have some side effects, such as nausea, diarrhea, headache, and dizziness. In uncommon instances, it might possibly also trigger a decrease within the number of blood cells, which can result in anemia and different blood-related problems.
One of the key options of Linezolid is its broad spectrum of activity. It is effective in opposition to gram-positive micro organism, together with strains which are proof against different antibiotics similar to methicillin-resistant Staphylococcus aureus (MRSA). This makes it a first-line remedy choice for serious infections caused by these bacteria, corresponding to skin and soft tissue infections, pneumonia, and even sepsis.
Linezolid, generally identified by its model name Zyvox, is a strong antibiotic used to treat infections brought on by Enterococcus and Streptococcus bacteria. It belongs to a category of antibiotics known as oxazolidinones, which work by inhibiting protein synthesis within the bacteria, in the end leading to their dying. Linezolid has been confirmed to be effective against even the most drug-resistant strains of bacteria, making it a life-saving medication for so much of sufferers.
Another benefit of Linezolid is its availability in each oral and intravenous forms. This makes it a versatile antibiotic, as it can be utilized in both hospital and outpatient settings. The oral formulation of Linezolid can be helpful for sufferers who require long-term therapy, as it can be taken at home quite than having to remain in a hospital for intravenous administration.
Despite these potential drawbacks, Linezolid stays a significant medication within the fight against bacterial infections. Its effectiveness against drug-resistant strains of micro organism has made it a crucial tool within the treatment of great infections. Moreover, it has been confirmed to have a low fee of resistance in comparison with other antibiotics, making it a more sustainable option for long-term use.
In conclusion, Linezolid, also referred to as Zyvox, is a robust antibiotic that has revolutionized the treatment of infections brought on by Enterococcus and Streptococcus bacteria. Its broad spectrum of exercise, availability in oral and intravenous forms, and effectiveness against drug-resistant strains have made it an indispensable medicine in the medical area. However, it's essential to use this medicine responsibly to stop the event of resistance and to report any potential unwanted side effects to a healthcare skilled. As with all antibiotics, correct use and consciousness of the potential dangers are essential to maintain this medication efficient.
They may be less familiar with the dissection of the urethra and bladder neck in women antibiotic resistance medical journals generic linezolid 600 mg buy on line. In a standard cystectomy, the bladder and prostate are completely freed off the rectum and mobilized posteriorly before the urethral dissection. If a nerve-sparing approach is planned, the urethra may be divided after the lateral pedicles are taken down to the bladder (anterior branches of the internal iliac vessels). The prostate is then dissected in a retrograde fashion off the rectum and bilateral neurovascular bundles, and the posterior pedicles are divided last. In either approach, all fibroareolar connections along the anterior bladder wall, prostate, and undersurface of the pubic symphysis are divided. The endopelvic fascia is incised adjacent to the prostate, and the levator muscles are gently swept off the lateral and apical portions of the prostate. The superficial branch of the deep dorsal vein is identified, ligated, and divided. The puboprostatic ligaments need to be incised only enough to allow proper apical dissection of the prostate. We use absorbable suture to avoid the risk for erosion of suture, clips, or staples into the urethral anastomosis. Once the venous complex has been ligated, it is divided close to the apex of the prostate. Any bleeding from the transected venous complex can be controlled with an absorbable suture. Care should be taken to avoid deep suture bites into the complex or levator muscles, which could injure the continence mechanism. Six 2-0 absorbable monofilament or woven polyglycolic acid sutures are placed in the urethra circumferentially under direct vision before complete division of the urethra, carefully incorporating only the wall of the urethra without including the levator muscles. Placing the urethral sutures at this time rather than after the bladder has been removed avoids the retraction of the urethra that makes subsequent accurate placement difficult. Two additional sutures are then placed, incorporating the rectourethralis muscle posteriorly and the caudal extent of the Denonvilliers fascia. The urethral sutures are tagged to identify their location and are placed under a towel until the urethroenteric anastomosis is performed. The surgical dissection at the prostatic apex in men and bladder neck in women must be carefully and precisely performed to achieve optimum continence while taking care not to compromise the oncologic effectiveness of the surgery. In both males and females, the urethral sphincter is made up of both smooth and striated muscles. The striated rhabdosphincter appears to be the most critical for continence and is innervated by the pudendal nerve. Careful neuroanatomic dissections with three-dimensional reconstructions of male and female cadavers have defined the anatomy of the urethral sphincter mechanism (Borirakchanyavat et al. No clearly defined line could be identified between the transverse smooth muscle cranially and the striated muscle caudally. Rather, a gradual transition was noted in the middle third of the urethra, with intermingling fibers of both types of muscle. Fluorourodynamic studies performed on women who had undergone orthotopic reconstruction after cystectomy also identified the mid-urethra as the primary continence zone (Grossfeld et al. Branches off the pudendal nerve coursing beneath the levator muscle can be traced to the rhabdosphincter. Delicate fibers from the perineal portion of the pudendal nerve course underneath the urogenital diaphragm, entering the caudal portion of the urethra laterally (Colleselli et al. If there is tumor at the prostatic apex, the urethral stump can be excised or a total urethrectomy may be performed at this time to obtain a negative margin, and a cutaneous diversion constructed. The contribution of prospective nerve-sparing to subsequent continence in male patients is controversial. Retrospective studies suggest continence may be improved if nerve-sparing is attempted, though in all such series it is impossible to control for the impact of selection bias (Turner et al. However, when oncologically safe it is reasonable to attempt never-sparing in a potent patient when a orthotopic diversion is planned. Vagina Urethra Foley balloon at bladder neck Preservation of the Urethra in the Female Patient When orthotopic diversion is considered in female patients, several technical issues should be noted to optimize the continence mechanism (Stein and Skinner, 2004; Stein et al. A standard female cystectomy includes removal of the uterus, cervix, and ovaries (anterior exenteration). However, in selected female patients with clinically lower-stage disease, a number of authors have advocated preservation of the uterus and ovaries (Ali-El-Dein et al. It appears that preserving the uterus and its supportive ligaments eliminates the risk for vaginal fistula, improves sexual function, and may decrease late urinary retention in women undergoing neobladder reconstruction (see later). If the uterus is preserved, the branches of the internal iliac artery feeding the bladder are taken distal to the takeoff of the uterine artery, and the ureteral stump must be dissected from below the uterine artery. Whether the uterus is removed or not, whenever possible the bladder is dissected completely off the anterior vaginal wall rather than excising it. However, a deeply invasive tumor on the posterior bladder or trigone may necessitate excision of a portion of the anterior vaginal wall. This does increase the risk for subsequent pouch-vagina fistula but is not an absolute contraindication to orthotopic reconstruction. A patient with a significant tumor at the bladder neck or with palpable extension into the vaginal wall is a poor candidate for neobladder and should undergo en bloc urethrectomy and cutaneous diversion. In developing the posterior pedicles, if a hysterectomy is planned the posterior vagina is incised at the fornix behind the cervix.
Staple lines are not directly apposing for their entire distance to avoid ischemia between adjacent staple lines bacteria yogurt 600 mg linezolid purchase free shipping. Arrow indicates site of enterotomy where urethroileal anastomosis will be performed. The reabsorption and recirculation of urinary constituents and other metabolites require that liver function be normal and that serum creatinine levels be in the normal range and preferably below the level of 1. There have been isolated reports of malignancy developing earlier, and all patients developing gross or microscopic hematuria should be fully evaluated. For right colon pouches, appendiceal techniques, pseudoappendiceal tubes fashioned from ileum or right colon, and ileocecal valve plication are adaptable. Appendiceal tunneling techniques are the simplest of all to perform in that they use established surgical techniques that are already in the urologic armamentarium. However, some patients have developed rather striking diarrhea and steatorrhea after the loss of the ileocecal valve. The creation of nipple valves is the most technologically demanding of all the continence mechanisms and is associated with the highest complication rate. In this procedure, a small bowel segment is isolated and a reversed intussusception is used to appose the surfaces of the small bowel. Most authors would suggest that bacteriuria in the absence of symptomatology does not warrant antibiotic treatment. It is among the easiest to construct, and it has very low short-term and long-term complications. However, given the complex nature of these diversions, the benefits over an open approach may be limited. Hardt J, Filipas D, Hohenfellner R, et al: Quality of life in patients with bladder carcinoma after cystectomy: first results of a prospective study, Qual Life Res 9:112, 2000. A new antireflux technique for ureteroileal anastomosis: a serous lined extramural tunnel, Urol Res 21:135140, 1993. Austen M, Kalble T: Secondary malignancies in different forms of urinary diversion using isolated gut, J Urol 172:831838, 2004. Bihrle R: the Indiana pouch continent urinary reservoir, Urol Clin North Am 24:773779, 1997. Burger R, Wammack R, Fisch M, et al: the appendix as a continence mechanism, Eur Urol 22:255262, 1992. DeGer S, Peters R, Roigas J, et al: Laparoscopic radical cystectomy with continent urinary diversion (rectosigmoid pouch) performed completely intracorporeally: an intermediate functional and oncologic analysis, Urology 64(5):935939, 2004. Fisch M, Hohenfellner R: Der sigma rektum pouch: eine modifikation der harnleiterdarm implantation, Aktuelle Urol 22:1991. Helal M, Pow-Sang J, Sanford E, et al: Direct (non-tunneled) ureterocolonic reimplantation in association with continent reservoirs, J Urol 150:835837, 1993. Hohenfellner R, Black P, Leissner J, et al: Refluxing ureterointestinal anastomosis for continent cutaneous urinary diversion, Urology 168(3):10131067, 2002. Riedmiller H, Steinbach F, Thüroff J, et al: Continent appendix stoma-a modification of the Mainz pouch technique. Rink M, Kluth L, Eichelberg E, et al: Continent catheterizable pouches for urinary diversion, Eur Urol Suppl 9:754762, 2010. Sinaiko E: Artificial bladder segment of stomach and study of effect of urine on gastric secretion, Surg Gynecol Obstet 102:433, 1956. Stein R, Matani Y, Doi Y, et al: Continent urinary diversion using the Mainz Pouch I technique-ten years later, J Urol 153:251A, 1995. Kristiansen P, Mansson W, Tyger J: Perforation of continent caecal reservoir for urine twice in one patient, Scand J Urol Nephrol 25:279281, 1991. Kristjansson A, Bajc M, Wallin L, et al: Renal function up to 16 years after conduit or continent urinary diversion: renal scarring and location of bacteriuria, Br J Urol 76:546550, 1995. Lampel A, Fisch M, Stein R, et al: Continent diversion with the Mainz pouch, World J Urol 14:8591, 1996. Lampel A, Hohenfellner M, Schultz-Lampel D, et al: In situ tunneled bowel flap tubes: two new techniques of a continent outlet for Mainz pouch cutaneous diversion, J Urol 153:308315, 1995a. Lampel A, Hohenfellner M, Schultz-Lampel D, et al: Submucosal seromuscular tube and submucosal bowel flap tube: two new stoma techniques for Mainz pouch continent cutaneous urinary diversion, J Urol 153:305A, 1995b. LeDuc A, Camey M, Teillac P: An original antireflux ureteroileal implantation technique: long-term follow-up, J Urol 137:11561158, 1987. Mansson W, Colleen S, Forsberg L, et al: Renal function after urinary diversion: a study of continent caecal reservoir, ileal conduit, and colonic conduit, Scand J Urol Nephrol 18:307315, 1984. Mitrofanoff P: Cystostomie continente trans-appendiculaire dans le traitement des vessies neurologiques, Chir Pediatr 21:297305, 1980. Terai A, Arai Y, Kawakita M, et al: Effect of urinary intestinal diversion urinary risk factors for urolithiasis, J Urol 153:3741, 1995. Touma N, Spodek J, Kuan J, et al: Confirming routine stentograms after cystectomy is unnecessary, Can Urol Assoc J 1(2):103105, 2007. Türk I, Deger S, Winkelmann B, et al: Laparoscopic radical cystectomy with continent urinary diversion (rectal sigmoid pouch) performed completely intracorporeally: the initial 5 cases, J Urol 165(6 Pt 1):18631866, 2001. Wiesner C, Bonfig R, Stein R, et al: Continent cutaneous urinary diversion: long-term follow-up of more than 800 patients with ileocecal reservoirs, World J Urol 24:315318, 2006. The objective of bladder substitution is to allow volitional voiding through the urethra while eliminating the need for a cutaneous urinary stoma or intermittent catheterization.
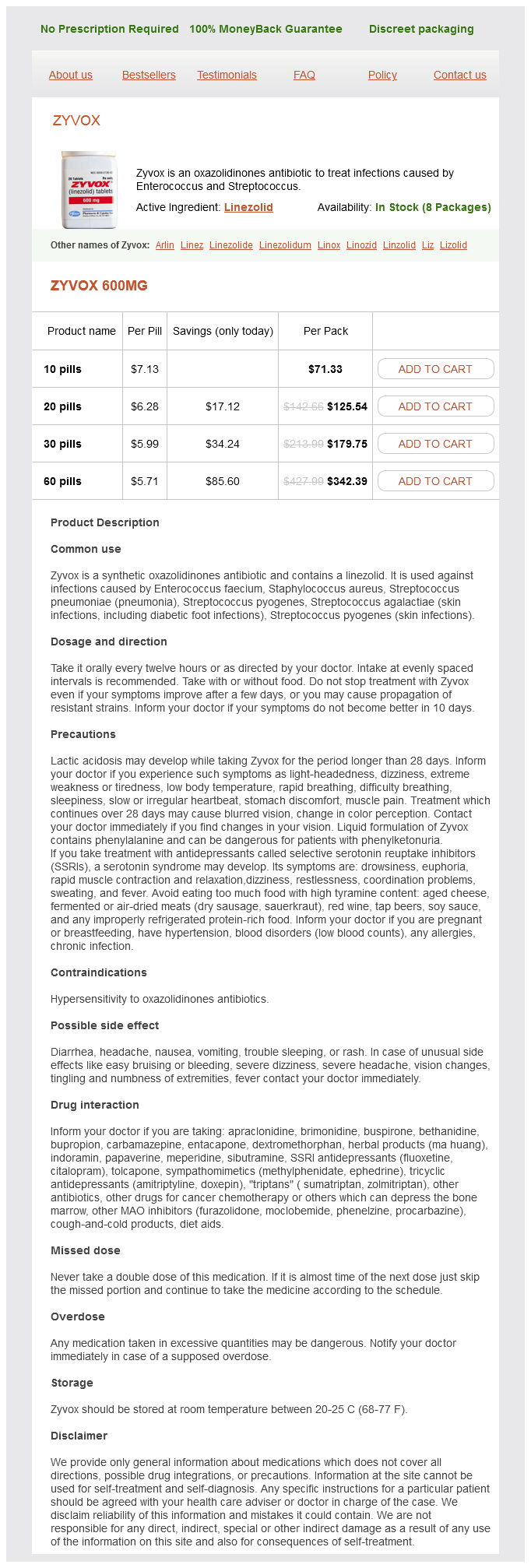
Linezolid Dosage and Price
Zyvox 600mg
- 10 pills - $71.33
- 20 pills - $125.54
- 30 pills - $179.75
- 60 pills - $342.39
Persky L antibiotic resistance join the fight 600 mg linezolid for sale, Rabin R: Experiences with vesicovaginal fistulas, Am J Surg 125(6):763766, 1973. Persky L, Herman G, Guerrier K: Nondelay in vesicovaginal fistula repair, Urology 13(3):273275, 1979. Pettersson S, Hedelin H, Jansson I, et al: Fibrin occlusion of a vesicovaginal fistula, Lancet 1(8122):933, 1979. Porpiglia F, Destefanis P, Fiori C, et al: Preoperative risk factors for surgery female urethral diverticula. Powers K, Grigorescu B, Lazarou G, et al: Neglected pessary causing a rectovaginal fistula: a case report, J Reprod Med 53(3):235237, 2008. Pushkar D: Editorial comment on: transpubic access using pedicle tubularized labial urethroplasty for the treatment of female urethral strictures associated with urethrovaginal fistulas secondary to pelvic fracture, Eur Urol 56(1):200, 2009. Sapmaz E, Celik H, Semercioz A: Omental graft use in Youssef syndrome, Eur J Obstet Gynecol Reprod Biol 109(1):9296, 2003. Schoellnast H, Lindbichler F, Riccabona M: Sonographic diagnosis of urethral anomalies in infants: value of perineal sonography, J Ultrasound Med 23(6):769776, 2004. Shaker H, Saafan A, Yassin M, et al: Obstetric vesico-vaginal fistula repair: should we trim the fistula edges Sherif A, Karacagil S, Magnusson A, et al: Endovascular approach to treating secondary arterioureteral fistula, Scand J Urol Nephrol 36(1):8082, 2002. Starownik R, Michalak J, Bar K, et al: An uncommon case of inflammatory infiltration of the urinary bladder in the long-term process of the purulent inflammation of the cervix and vaginal fornix, complicated with vesicovaginal fistula of unknown etiology, Cent European J Urol 66(1):101103, 2013. Tatar B, Oksay T, Selcen Cebe F, et al: Management of vesicovaginal fistulas after gynecologic surgery, Turk J Obstet Gynecol 14(1):4551, 2017. Thomas C, Jones J, Jager W, et al: Incidence, clinical symptoms and management of rectourethral fistulas after radical prostatectomy, J Urol 183(2):608612, 2010. Turner-Warwick R: the use of the omental pedicle graft in urinary tract reconstruction, Trans Am Assoc Genitourin Surg 67:126132, 1975. Uchida T, Tomonaga T, Kim H, et al: Improved outcomes with advancements in high intensity focused ultrasound devices for the treatment of localized prostate cancer, J Urol 193(1):103110, 2015. Un S, Cakir V, Kose O, et al: Colon perforation during percutaneous nephrolithotomy and fistula closure with Spongostan following conservative therapy, Can Urol Assoc J 9(56):E313E315, 2015. Ungar L, Palfalvi L, Novak Z: Primary pelvic exenteration in cervical cancer patients, Gynecol Oncol 111(2 Suppl):S9S12, 2008. Verbaeys C, Hoebeke P, Oosterlinck W: Complicated postirradiation vesicovaginal fistula in young women: keep off or try reconstruction Wilson A, Pillay S, Greenwell T: How and why to take a Martius labial interposition flap in female urology, Transl Androl Urol 6(Suppl 2):S81S87, 2017. Xiong Y, Tang Y, Huang F, et al: Transperitoneal laparoscopic repair of vesicovaginal fistula for patients with supratrigonal fistula: comparison with open transperitoneal technique, Int Urogynecol J 27(9):14151422, 2016. Xu H, Chen Y, Li Y, et al: Complications of laparoscopic radical hysterectomy and lymphadenectomy for invasive cervical cancer: experience based on 317 procedures, Surg Endosc 21(6):960964, 2007. Yan X, Li G, Shang H, et al: Complications of laparoscopic radical hysterectomy and pelvic lymphadenectomyexperience of 117 patients, Int J Gynecol Cancer 19(5):963967, 2009. Yildirim M, Goktas C, Horuz R, et al: Rectal injury during radical prostatectomy, Ulus Travma Acil Cerrahi Derg 18(3):250254, 2012. Yildiz M, Atan A, Aydoganli L, et al: Renocolic fistula secondary to chronic pyelonephritis, Int Urol Nephrol 25(3):229233, 1993. Ying T, Li Q, Shao C, et al: Value of transrectal ultrasonography in female traumatic urethral injuries, Urology 76(2):319322, 2010. Yu S, Wu H, Xu L, et al: Early surgical repair of iatrogenic ureterovaginal fistula secondary to gynecologic surgery, Int J Gynaecol Obstet 123(2):135 138, 2013. Zhaohui H, Hanqi L, Xiongbing L, et al: Analysis of repeated renal arteriography after percutaneous nephrolithotomy, Urolithiasis 2016. Vaginal approach for repair of vesicovaginal fistulae, Urol Clin North Am 12(2):361 367, 1985. Zmora O, Tulchinsky H, Gur E, et al: Gracilis muscle transposition for fistulas between the rectum and urethra or vagina, Dis Colon Rectum 49:13161321, 2006. Verma A, Vyas S, Patwari S, et al: Magnetic resonance fistulogram demonstration of urethrovesicovaginal fistula in a case of mullerian agenesis due to traumatic urethral coitus, J Minim Invasive Gynecol 19(2):259261, 2012. Vidal Sans J, Pradell Teigell J, Palou Redorta J, et al: Review of 31 vesicointestinal fistulas: diagnosis and management, Eur Urol 12(1):2127, 1986. Vora A, Agarwal V, Singh P, et al: Single-institution comparative study on the outcomes of salvage cryotherapy versus salvage robotic prostatectomy for radio-resistant prostate cancer, Prostate Int 4(1):710, 2016. Waaldijk K: the immediate surgical management of fresh obstetric fistulas with catheter and/or early closure, Int J Gynaecol Obstet 45(1):1116, 1994. Waaldijk K: Immediate indwelling bladder catheterisation at postpartum urine leakage - personal experience of 1200 patients, Trop Doct 27:227228, 1997. Waaldijk K: the immediate management of fresh obstetric fistulas, Am J Obstet Gynecol 191(3):795799, 2004. George Hayward (1791-1863): a forgotten pioneer of reconstructive pelvic surgery, Int Urogynecol J Pelvic Floor Dysfunct 16(5):330333, 2005. This results in a thin-walled, urine-filled structure adjacent to and connecting with the bladder lumen through a variably sized neck, or ostium. A fibrous capsule or pseudocapsule outer shell is often present and may be a useful surgical plane for excision. The outside wall of the bladder diverticulum often contains some residual scattered strands or bundles of smooth muscle; however, these are disorganized and nonfunctional. Therefore bladder diverticula generally empty poorly during micturition, leaving a large postvoid residual urine volume that results in the characteristic findings on presentation and imaging. Classification, Pathophysiology, and Etiology Bladder diverticula may occur in adults or children, but overall approximately 90% of bladder diverticula occur in adults (Psutka and Cendron, 2013).