Lopressor
General Information about Lopressor
One of the principle advantages of Lopressor is its selectivity. Unlike different beta-blockers, it has a higher affinity for β1 receptors than for β2 receptors found in different elements of the physique such as the lungs. This selectivity limits its unwanted facet effects, making it a safer possibility for sufferers. Common beta-blocker side effects, similar to shortness of breath and fatigue, are less prone to happen with the utilization of Lopressor. This makes it an appropriate selection for sufferers who may have underlying respiratory circumstances similar to asthma and chronic obstructive pulmonary illness (COPD).
Furthermore, Lopressor has proven to be an effective medicine for the therapy of hypertension. Research has shown that it can significantly reduce the risk of coronary heart attack, stroke, and general mortality in folks with high blood pressure. It has additionally been discovered to be useful in managing angina and coronary heart arrhythmia, bettering signs and decreasing the chance of significant problems.
To understand how Lopressor works, we should first understand the function of β1 receptors in our body. These receptors play an important position in regulating coronary heart price and blood stress by responding to adrenaline, a hormone that is naturally produced by our our bodies in instances of stress. Adrenaline binds to these receptors, causing an increase in coronary heart fee and blood stress. In individuals with situations such as hypertension, angina, and heart arrhythmia, this response can be exaggerated and probably dangerous. Lopressor works by blocking the β1 receptors, in flip slowing down the heart price and lowering the pressure of every heartbeat, thus reducing blood stress and relieving signs of angina and heart arrhythmia.
However, as with all treatment, Lopressor does include potential unwanted effects. These could include dizziness, weak point, and upset stomach, which usually subside because the body adjusts to the medication. In uncommon instances, extra critical side effects corresponding to sluggish coronary heart rate and problem respiratory could occur. It is essential to seek the guidance of together with your physician should you expertise any of these symptoms.
In addition to its selectivity, Lopressor additionally has an extended half-life compared to other beta-blockers, which means that it stays within the body for a longer time frame. This permits for a once-daily dosage, which is extra handy for sufferers and helps enhance compliance with therapy. Lopressor additionally comes in extended-release formulations, making it a super choice for sufferers who could forget to take their medication or have problem sticking to a strict dosing schedule.
In conclusion, Lopressor has been providing aid for tens of millions of people with hypertension, angina, and coronary heart arrhythmia for over 50 years. Its selectivity, convenience, and proven effectiveness make it a top choice for docs and sufferers alike. However, as with all medicine, you will need to talk about your medical history and any potential risks along with your doctor earlier than beginning Lopressor. With correct use and monitoring, Lopressor can help you regain control over your heart well being and improve your overall well-being.
For millions of individuals around the globe, the words “high blood pressure”, “angina”, and “heart arrhythmia” can evoke a sense of concern and confusion. These are only a few of the numerous circumstances that may affect the well being of our heart, and finding an effective therapy can be life-changing. Fortunately, there’s a medicine that has been offering reduction for these conditions for over five a long time – Lopressor.
Lopressor, also known by its generic name metoprolol, is a beta-blocker that selectively targets the β1 receptors discovered within the coronary heart. It was first marketed in 1969 and has since turn into a broadly prescribed medicine for the therapy of hypertension (high blood pressure), angina (chest pain), and heart arrhythmia (irregular coronary heart rhythm). But what precisely makes Lopressor so effective and why is it the popular alternative for so much of docs and patients?
Bactericidal activity was superior at the 8-week assessment blood pressure chart elderly effective lopressor 12.5 mg, although the predictive utility of that end point remains controversial. Drugs may then be cautiously reintroduced in a stepwise fashion while serum aminotransferase levels are monitored. For patients with peripheral neuropathy, experts recommend increasing pyridoxine dose to 100 mg/day. Although there are no studies that compare five with seven daily doses, extensive experience indicates this would be an effective practice. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Not recommended for children too young for monitoring of vision unless drug resistant. Modified from the 2007 Maryland Guidelines for Prevention and Treatment of Tuberculosis. Extent of disease can be quantified by the mycobacterial content of sputum, with smear- and culture-positive sputum representing most severe disease, smear-negative and culture-positive sputum representing intermediate disease, and smear- and culture-negative sputum representing the least amount of disease. The possibility that the early bactericidal activity of moxifloxacin or gatifloxacin in combinations might permit 4-month regimens in smear-positive, culture-positive cases has, to date, not been confirmed (see "Fluoroquinolones"). These prevent the patient from omitting drugs and taking monotherapy and therefore decrease the risk for resistance. If a suboptimal regimen is prescribed, resistance to additional drugs may emerge and the opportunity for success may be lost. In this setting, 2-month sputum culture conversion rates are improved by adding bedaquiline. Relapse after adequate treatment of drug-sensitive infections is infrequent (2%5%). Prolonged follow-up of appropriately treated patients is not necessary except in the case of unusually extensive disease, slow bacteriologic response to treatment, suspicion of poor compliance, drug-resistant disease, or high-risk patients with intercurrent diseases. Clinical judgment based on experience is critical in re-treatment cases, and testing of susceptibility to first- and second-line drugs is required. The intensive phase of treatment is for 8 months, and the total treatment duration is 20 months. A prolonged course of treatment is necessary, but the optimal duration is unknown. Beginning 1 month after initiation of therapy, three sputum cultures should be obtained monthly to monitor conversion to negative or, if sputum cultures remain positive, to detect treatment failure and the possible emergence of drug resistance. In a minority of patients, sputum smears remain positive after cultures turn negative. Sporadic positive smears for long periods presumably represent inactive bacilli released from caseous foci. When cultures remain positive after 4 months of treatment, it is considered treatment failure. Causes of treatment failure include drug resistance, noncompliance with therapy, and malabsorption of antituberculosis drugs. Sensitivity testing should be performed and consideration given to adding at least two new drugs to which the organism was sensitive at the outset of treatment, at least until sensitivities are known. Adherence to therapy should be ensured and serum drug levels considered to assess absorption. In persons with abnormal hepatic aminotransferase levels at baseline, such laboratory findings should be Other Forms of Treatment Bed rest does not influence outcome when effective chemotherapy is given. Resection still has a role in the salvage of patients in whom treatment fails and who have localized, resectable disease, and extensive drug resistance. Corticosteroids Corticosteroids in conjunction with antituberculosis therapy improve neurologic outcome and mortality in persons with tuberculous meningitis. These interactions 3007 affect the choice of therapy (and appropriate doses) for both diseases. Rifabutin may be used in combination with protease inhibitors, with appropriate dose modification. Although it is preferred to not coadminister these drugs, if it is done, the dose of maraviroc should be increased to 600 mg twice daily. A 4-week course of prednisone improved symptoms and decreased the need for hospitalization in one clinical trial. Paradoxical reactions in previously healthy patients can be confused with uncontrolled infection. Biochemical monitoring of hepatotoxicity during renal failure may be complicated by abnormally low aminotransferase levels in uremia. The selection and dosage of antituberculous agents do not need to be modified in most patients with underlying liver disease, but hepatic aminotransferase and bilirubin levels must be followed closely. Pyridoxine supplementation, 10 to 50 mg daily, is recommended to prevent peripheral neuropathy in persons older than 65 years; pregnant and breastfeeding women; persons with diabetes mellitus, chronic renal failure, or alcoholism; persons undergoing treatment with anticonvulsants; and persons who are malnourished. The number in the elderly was probably falsely low because of a small sample size. Most hepatitis develops within the first 3 months, and the risk for death, once clinical hepatitis develops, is substantial. Many patients with severe biochemical hepatitis would not have been detected with monitoring of symptoms only.
At the genus level hypertension obesity lopressor 25 mg visa, these organisms are biochemically similar to Pasteurella species. They have also been recovered from chlorinated tap water, including hospital water supplies. They occasionally cause soft tissue infections and sepsis in immunocompromised hosts and increasingly have been associated with diarrheal disease and other infections in immunocompetent individuals. Taxonomy of the aeromonads has been revised over the past few decades and continues to be in transition. Aeromonads are broadly divided into the mesophilic group, with optimal growth temperatures of 35°C to 37°C and associated with human infection, and the psychrophilic group, with optimal growth temperatures of 22°C to 25°C and associated with disease in fish. The aerolysin/ hemolysin group of toxins, including Act, are important virulence factors in A. Alt and lateral flagella are notably significantly less prevalent in these species. Reports from diverse geographic locations have associated Aeromonas species with diarrheal disease in humans; in some locales, they are recovered as commonly as Shigella or Campylobacter. Many laboratories do not routinely culture stool for Aeromonas, so the incidence of Aeromonas-associated diarrhea may be underestimated. Evidence supporting a causative role in diarrheal disease includes (1) a higher carriage rate in symptomatic compared with asymptomatic individuals; (2) an absence of other enteric pathogens in most symptomatic patients harboring Aeromonas species; (3) identification of Aeromonas enterotoxins22; (4) improvement of diarrhea with antibiotics active against Aeromonas species and clinical worsening with antibiotics ineffective against the organism; and (5) evidence of a specific secretory immune response coincident with diarrheal disease. Aeromonas caviae is the predominant isolate from diarrheal stools, but in some geographic areas, A. An epidemiologic study was unable to implicate the drinking water supply as the source of diarrheal isolates; Aeromonas isolates from diarrheal stool were genetically unrelated to those from water supplies. Diarrhea is usually watery and self-limited, but some persons develop fever, abdominal pain, and bloody stools. Occasionally, diarrhea may be severe or protracted, and hospitalization may be necessary. Rare cases of ischemic colitis associated with Aeromonas have been reported in healthy children and adults, and chronic colitis developing after acute Aeromonasassociated diarrhea has been reported in adults. Hemolytic-uremic syndrome associated with Aeromonas enterocolitis has been described in infants and adults. The relevance of this finding is supported by in vitro studies demonstrating that preinfection of enterocyte-like cells with rotovirus can increase the capacity of some Aeromonas strains to adhere to enterocytes. Trauma followed by exposure to fresh or brackish water (and not salt water, even though aeromonad density in seawater is similar to that in fresh water) usually, but not invariably, precedes infection. Fasciitis, myonecrosis (occasionally associated with gas formation), and osteomyelitis may develop. In the setting of a rapidly progressive cellulitis after an injury related to water exposure, Aeromonas and Vibrio species infections should be considered in the differential diagnosis. Aeromonas soft tissue infections can develop after exposure to soil, in association with crush injuries, and as a complication of burns, typically when initial management of the burn included immersion in natural water sources. Leeches lack the requisite proteolytic enzymes and are dependent on the symbiotic Aeromonas to digest the blood meal. Aeromonas bacteremia and sepsis are uncommon, but in the largest series reported to date, 143 Aeromonas bacteremias, including 104 that were monomicrobial, occurred in one institution in Taiwan over a 10-year period. Spontaneous bacterial peritonitis was common in cirrhotic patients with abdominal pain. There was a similar distribution of Aeromonas species in a study of 53 Aeromonas blood isolates collected from 27 medical centers in the United States over a 10-year period. The organisms grow well on MacConkey agar (some strains are lactose fermenters and some are not), but growth on thiosulfate citratebile saltssucrose medium is variable. Selective techniques are often necessary for the isolation of Aeromonas species from mixed cultures. The organisms are more difficult to identify in stool cultures because enteric media may be inhibitory for some Aeromonas species. Either blood agar that contains ampicillin (10 or 30 µg/mL) or cefsulodin irgasan novobiocin agar can be used as a selective medium. Aeromonas species are oxidase positive, helping to distinguish these organisms from Enterobacteriaceae. Identification of Aeromonas to the genus level is generally not difficult, but misidentifications, particularly as Vibrio species, may occur with automated systems. Cardiobacterium hominis and Cardiobacterium valvarum are the only two species in the genus Cardiobacterium. Cardiobacterium species have been described as Pasteurella-like organisms; they are part of the microbiota in the nose, mouth, and throat and are present occasionally on other mucous membranes as well as in the gastrointestinal tract. The mortality rate is about 10%, and valve replacement is needed in about 30% of cases. In one of the very rare cases of infection without endocarditis, a patient with adenocarcinoma of the kidney invading the cecum developed an abdominal abscess and bacteremia; abscess and blood cultures grew C. They often have swelling of one or both ends and retain the crystal violet dye at the poles during the Gram stain procedure. Microscopically, the organisms sometimes form rosettes, but short chains, teardrops, pairs, and clusters are also common. Supplementation of the medium with yeast extract results in a loss of the pleomorphism, and most organisms become sticklike, gram-negative rods with rounded ends. Most strains grow better on sheep blood agar than chocolate agar and will grow on Mueller-Hinton agar or trypticase soy agar without blood, but grow poorly on MacConkey agar or similar selective media. However, with some systems, incubation for 5 to 7 days before growth can be confirmed is not unusual, and cultures should be held for this period or longer if C. Susceptibility tests are difficult to perform because of the slow growth of the organism and unusual nutritional requirements, although the Etest appears to be useful. Systemic embolization, mycotic aneurysm, or progressive cardiac failure has necessitated valve replacement in a number of cases.
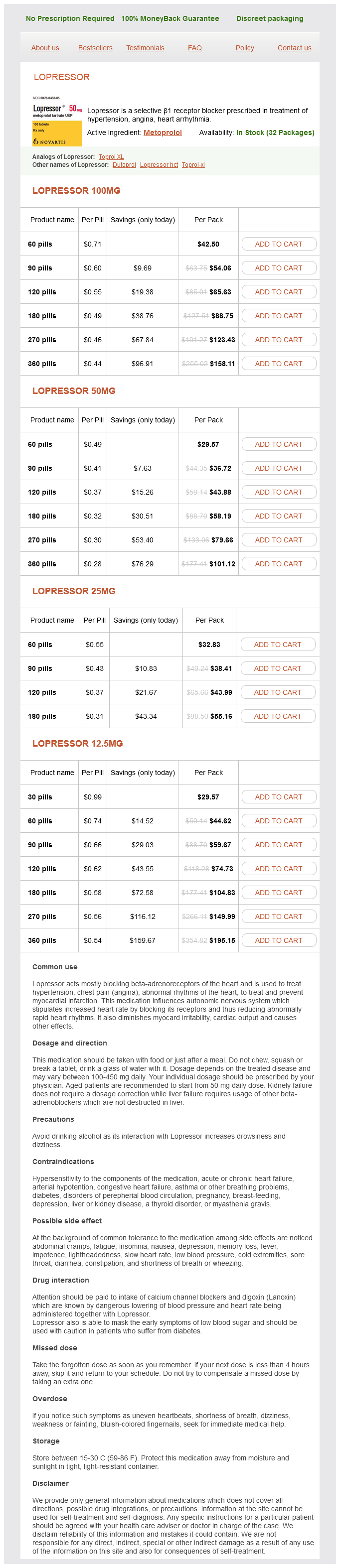
Lopressor Dosage and Price
Lopressor 100mg
- 60 pills - $42.50
- 90 pills - $54.06
- 120 pills - $65.63
- 180 pills - $88.75
- 270 pills - $123.43
- 360 pills - $158.11
Lopressor 50mg
- 60 pills - $29.57
- 90 pills - $36.72
- 120 pills - $43.88
- 180 pills - $58.19
- 270 pills - $79.66
- 360 pills - $101.12
Lopressor 25mg
- 60 pills - $32.83
- 90 pills - $38.41
- 120 pills - $43.99
- 180 pills - $55.16
Lopressor 12.5mg
- 30 pills - $29.57
- 60 pills - $44.62
- 90 pills - $59.67
- 120 pills - $74.73
- 180 pills - $104.83
- 270 pills - $149.99
- 360 pills - $195.15
The production of -lactamases is the most common mechanism among anaerobes hypertension kidney infection buy discount lopressor online, especially among the B. Penicillin G, ampicillin, and amoxicillin are equally active against anaerobic strains that do not produce -lactamase, but the semisynthetic penicillins (methicillin, nafcillin, and oxacillin or dicloxacillin) have unpredictable activity and frequently are inferior to penicillin G. The semisynthetic penicillins-carboxypenicillins (carbenicillin, ticarcillin) and ureidopenicillins (piperacillin, azlocillin, mezlocillin)-generally are administered in high doses and display good activity against most anaerobes in these concentrations; however, up to 30% of B. The cephalosporinases has little or no activity against the cephamycins cefoxitin and cefotetan, which display greater activity against anaerobic organisms, Approximately 85% of B. A study of 396 samples demonstrated the inefficiency of this combination against anaerobes, such as B. Carbapenems (ertapenem, doripenem, meropenem, and imipenem) are equally active against anaerobes, with <1% of B. Higher rates of nonsusceptibility are being reported from some countries (5% in Germany, 8% [to doripenem] in Canada, and 7%12% in Taiwan). Resistance to metronidazole is more prevalent among gram-positive anaerobes, including C. This antibiotic is well tolerated, reaches significant levels in serum, and penetrates abscesses well. Up to 10% resistance was found in Prevotella, Fusobacterium, Porphyromonas, and Peptostreptococcus spp. Fluoroquinolones such as moxifloxacin have the potential to treat mixed aerobic/anaerobic infections. However, a survey in the United States found 38% resistance to moxifloxacin among the B. The macrolides erythromycin, azithromycin, and clarithromycin have moderate-to-good in vitro activity against anaerobic bacteria other than the B. Because anaerobic infections can cause severe tissue damage or result in abscess formation, débridement of necrotic tissue, drainage of abscesses, restoration of airspaces, resection, maintenance of blood supply, or a combination of these interventions is necessary. The antibiotics used to treat anaerobic infections should be active against both aerobic and anaerobic organisms because many of these infections are of mixed etiology. Antibiotic regimens are usually selected empirically on the basis of the type of infection, the species of organisms usually present in such cases, Gram stain results, and knowledge of antimicrobial resistance patterns. Other factors influencing the selection of antibiotics include the need for bactericidal activity and for penetration into certain organs (such as the brain), the risk of toxicity, and consideration of the impact on the normal microbiota. Antibiotic susceptibility testing of anaerobic bacteria is rarely performed in clinical laboratories because of inadequate anaerobic culture techniques, difficulty in obtaining results within a useful time frame, and poor quality control of in vitro susceptibility results. It is accepted that testing is important for patients with serious or prolonged infections or in cases in which antibiotics have not had an impact. Testing is also helpful in monitoring the activity of new drugs and recording current resistance patterns among anaerobic pathogens. A correlation between the antimicrobial resistance of an anaerobic pathogen and a poor clinical outcome has been reported in several retrospective trials. A study of antibiotic-treated patients with Bacteroides isolates from blood found mortality rates of 45% among those whose isolates were deemed resistant to the agent used and 16% among those whose isolates were deemed sensitive. The antibiotics with the greatest activity against nearly all anaerobic bacteria include carbapenems, -lactam/-lactamase inhibitor combinations, metronidazole, and chloramphenicol (Table 242. The major changes have involved the activity of clindamycin, cephamycins, and moxifloxacin against B. Of interest are the higher resistance rates found among the "other Bacteroides" (nonB. Clindamycin no longer recommended for complicated intraabdominal infections Variable and increasing resistance. Cefotetan no longer recommended for complicated intraabdominal infections Good activity against most anaerobes; however, up to 30% of B. Resistance has been reported Variably Resistant Penicillin Inactive versus some or most penicillinase-producing anaerobes, including most of B. Tigecycline, a glycylcycline, is active against anaerobic bacteria, including most Bacteroides spp. Tigecycline has been used as a single-agent treatment for complicated intraabdominal infections; however, resistance (6%) among Bacteroides and nonBacteroides spp. Despite excellent in vitro activity against all clinically important anaerobes, chloramphenicol is less desirable than other active drugs for the treatment of anaerobic infection because of documented clinical failures and bone marrow toxicity. Anaerobic bacteria are intrinsically resistant to aminoglycosides and trimethoprim-sulfamethoxazole. As mentioned previously, resistance among some anaerobes has increased significantly over the past 3 decades. In clinical situations specific regimens must be tailored to the initial site of infection. Antibiotic treatment for intraabdominal infections needs to be directed against Bacteroides spp. Single agents suitable for patients with mildto-moderate community-acquired intraabdominal infections include the carbapenems and -lactam/-lactamase inhibitor combinations, such as piperacillin-tazobactam or ticarcillin-clavulanate. The Surgical Infection Society/Infectious Diseases Society of America 2010 guidelines also list cefoxitin, moxifloxacin, and tigecycline as options, but these agents should usually be avoided because of substantial rates of in vitro resistance to cefoxitin and fluoroquinolones among Bacteroides spp. Moxifloxacin may still be cautiously used for intraabdominal infections, provided that the patient has mild-tomoderate disease and has not been exposed to fluoroquinolones recently. A two-drug regimen is an alternative, with one drug active against coliforms and the other against anaerobes. In addition, if the clinician suspects that gram-positive facultative organisms, such as enterococci, are involved, therapeutic regimens should include ampicillin or vancomycin. Although clindamycin and cefotetan were previously considered acceptable options for intraabdominal infections involving anaerobes, these drugs are no longer recommended because of escalating rates of resistance in the B. Suitable regimens for these infections include clindamycin, -lactam/-lactamase inhibitor combinations, or penicillin together with metronidazole.