Maxolon
General Information about Maxolon
Aside from its antiemetic properties, Maxolon also has prokinetic results, which means it increases the motion and contractions of clean muscular tissues in the digestive system. This is especially useful in cases of gastroparesis, a condition where the abdomen muscle tissue are unable to effectively contract and empty meals into the small intestine. Maxolon stimulates the motion of meals via the digestive tract with out causing diarrhea, making it an efficient remedy for situations such as gastroparesis and biliary dyskinesia.
Another lesser-known however essential property of Maxolon is its capability to stimulate the secretion of prolactin, a hormone concerned in lactation and breast milk manufacturing. This makes it an effective medication for girls who are struggling with low milk provide whereas breastfeeding.
One of the explanation why Maxolon is so in style among medical professionals and sufferers alike is its capability to act as an antiemetic, which implies it helps to stop and deal with nausea and vomiting. The medication works by blocking dopamine receptors within the chemoreceptor trigger zone of the brain, which is responsible for triggering the vomiting reflex. By blocking these receptors, Maxolon reduces the sensation of nausea and likewise prevents vomiting.
Maxolon is a drugs primarily used to alleviate nausea and vomiting brought on by quite a lot of factors, including radiation therapy or cytotoxic drugs consumption, hypotony and atony of the stomach and intestines, biliary dyskinesia, reflux esophagitis, and flatulence. It can also be used to alleviate the symptoms of conditions corresponding to gastric ulcer and duodenal gut, and is often administered earlier than performing contrast studies of the gastrointestinal tract.
Maxolon is out there in pill, liquid, and injectable varieties, making it easily accessible and handy for patients. It is normally taken orally or administered by way of an IV, relying on the situation being treated and the severity of symptoms. In most instances, the medicine has minimal unwanted aspect effects, which can embrace drowsiness, diarrhea, and restlessness. However, these unwanted effects are typically delicate and do not affect most sufferers.
Nausea and vomiting could be debilitating symptoms that may significantly affect the day by day lives of individuals. Whether it is caused by a stomach bug, treatment side effects, or a extra severe medical condition, these signs could be uncomfortable and disruptive. In such cases, Maxolon, also called metoclopramide, has proven to be a dependable and effective symptomatic treatment in opposition to vomiting and nausea of varied origins.
In conclusion, Maxolon is a dependable and efficient medication for relieving symptoms of vomiting and nausea caused by varied elements. Its various vary of uses, such as in chemotherapy-induced nausea and vomiting, biliary dyskinesia, and reflux esophagitis, makes it a preferred choice amongst medical professionals and patients. With its mixture of antiemetic, prokinetic, and hormone-stimulating effects, Maxolon offers a comprehensive and holistic strategy to treating these bothersome signs. However, it's always important to seek the advice of a physician earlier than utilizing any medication, and to debate any potential risks or interactions.
Moreover, Maxolon also helps to cut back the shifting exercise of the esophagus and enhance the tone of the decrease esophageal sphincter, which helps to stop acid reflux disorder and different acid-related circumstances. This could be especially beneficial for individuals who are suffering from reflux esophagitis, a condition where abdomen acid flows back into the esophagus and causes inflammation.
Typical entry criteria for such a protocol would be:14 Labetolol: bolus of 20 mg i gastritis diet book cheap maxolon 10 mg online. Colloid should be infused prior to treatment if the baby is undelivered, to protect the uteroplacental circulation and prevent hypotension and fetal distress [E]. Antenatal complications: maternal eclampsia, or severe hypertension (>170/110 mmHg) with + or >1 g/24 hours proteinuria, or hypertension (>140/90 mmHg) with ++ or >3 g/24 hours proteinuria with an additional complication such Fluid management As women with pre-eclampsia can have a reduced intravascular volume, leaky capillary membranes and low albumin levels, they are prone to pulmonary oedema. Renal failure is a rare complication of pre-eclampsia that usually follows 190 Pre-eclampsia and non-proteinuric pregnancy-induced hypertension acute blood loss, when there has been inadequate transfusion, or as a result of profound hypotension. Oliguria without a rising serum urea or creatinine is a manifestation of severe pre-eclampsia and not of incipient renal failure. Administration of intravenous fluid in response to oliguria must be performed with caution [E]. Most protocols limit fluid intake (in the form of intravenous crystalloid) to approximately 1 mL/kg per hour [E]. In a well-perfused women, oliguria (<400 mL/24 hours) requires no treatment per se. If the creatinine or potassium rises, haemodialysis or haemofiltration may be necessary, and the advice of a renal physician should be sought. The administration of diuretics temporarily improves urine output, but further decreases the circulating volume and exacerbates electrolyte disturbances; frusemide should only be given if there are signs of pulmonary oedema [E]. In particularly difficult cases, pulmonary artery catheterization should be considered. Anaesthesia A general anaesthetic can be dangerous, as endotracheal intubation can cause severe hypertension. Regional blockade is the preferred method of analgesia for labour and of anaesthesia for operative deliveries [E], but a coagulopathy must be excluded. Platelet levels of <80 × 109/L should ensure haemostasis, and most obstetric anaesthetists will insert a regional block under these circumstances. Care must be taken to avoid arterial hypotension (particularly following postpartum haemorrhage) in view of the vasoconstriction and reduced intravascular volume. A low threshold for central invasive monitoring is necessary in women who require a caesarean section [E]. Postpartum care As a third of eclamptic fits occur postpartum, intensive monitoring is required, usually for 48 hours after delivery. Although eclampsia has been reported beyond this time, it is unlikely to be associated with serious morbidity. Anti-hypertensive therapy may therefore need to be continued after discharge home; in the absence of fetal considerations, the most effective therapy can be used and drugs such as methlydopa discontinued. All women who have suffered severe pre-eclampsia should be reviewed at a hospital postnatal clinic 612 weeks after delivery [E]. In addition to blood pressure and urine testing, tests of renal and liver function should be instigated; residual disease may merit referral to a physician. Underlying predispositions to pre-eclampsia, such as an inherited thrombophilia or antiphospholipid syndrome, should be excluded (multiparous women are more likely to have an underlying cause). The postnatal visit is also an excellent opportunity to discuss complications of the pregnancy and the planned management of any future pregnancy. Anticonvulsant therapy Magnesium sulphate can be used to control an eclamptic fit (up to 8 g). An eclamptic fit is usually self-limiting, and prolonged fitting warrants a brain scan to rule out other pathology, such as an intracerebral bleed [E]. If an eclamptic fit occurs, magnesium sulphate is the prophylaxis of choice, as demonstrated by the Eclampsia Trial [B]. Magnesium sulphate acts as a membrane stabilizer and vasodilator and reduces intracerebral ischaemia. It is usually given as a 2 g intravenous loading dose and a maintenance infusion at 12 g/hour. In cases of oliguria, care must be taken, as magnesium sulphate is renally excreted. Toxicity is detected by the absence of patellar reflexes, but ultimately respiratory arrest and muscle paralysis or cardiac arrest will occur. However, the Magpie Trial evaluated magnesium sulphate versus placebo in women with pre-eclampsia and demonstrated a clear benefit of prophylactic therapy [A]. Magnesium sulphate halved the risk of eclampsia and probably reduced the risk of maternal death. There did not appear to be any substantive harmful short-term effects to either the mother or baby. It is plausible that active assessment of cardiovascular risk up to six months postpartum may lead to earlier identification of cardiovascular risk and the potential for lifestyle modification. Both maternal and fetal morbidity and mortality are more likely to occur with early-onset disease. Despite the many tests being investigated, pre-eclampsia cannot be accurately predicted. An abnormal uterine artery Doppler at 20 weeks will increase risk approximately six-fold in both high- and low-risk women. Cerebral haemorrhage and adult respiratory distress are common causes of death in pre-eclampsia; therefore acute management focuses on controlling blood pressure and restricting fluid intake. The use of anti-hypertensive therapy in moderately hypertensive women demonstrates a significant reduction in severe hypertension only; there are no other proven additional benefits.
Assessment before induction commences As with any intervention gastritis complications 10mg maxolon order visa, before proceeding with an induction, it is important to ensure that the indication for induction still exists, and that any specific labour management issues that may occur as a consequence of the intervention are highlighted. The clinician must confirm the fetal lie and presentation by abdominal palpation, and assess the well-being of the fetus (commonly by electronic monitoring of the fetal heart rate). The likelihood of either successful induction or its failure may be most specifically ascertained by assessing the condition of the cervix. The most predictive elements in this system are the station of the presenting part, the length and dilatation of the cervix; as could be predicted, the shorter and more dilated the cervix, the shorter the interventionto-delivery interval. Induction methods traditionally utilized by women Castor oil this medication, when taken orally, stimulates contractions of the large and small intestine via an effect on the smooth muscle within the viscera. Its safety profile for mothers and babies has never been fully investigated and its use should therefore be discouraged. It may potentially increase the incidence of meconium staining of liquor as it has an effect on a term fetus similar to that on the mother [D]. First stage of labour Acupuncture the use of acupuncture for labour induction is based on the traditions of Chinese medicine that date back at least 346 Induction of labour 30 centuries. The published data from western literature are too small to address the issues of efficacy or safety, and its use outside the remits of clinical studies cannot be recommended. Herbal remedies Traditional remedies employed to stimulate the onset of labour rely on products that contain ergot derivatives in various strengths that consequently exhibit a weak uterine stimulant effect. The dose and purity of these compounds are often variable, and there is not sufficient evidence to support their use. The efficacy of raspberry leaf tea, whose potential for labour induction stems from observations on brood mares, is equally dubious. On a population basis, this may result in a decrease in the induction rate of 15 per cent, with no differences in maternal or fetal outcome [A]. However, it is important that before this is undertaken, women understand: the procedure is designed to impact as above; it may be a little uncomfortable; they may experience frequent contractions following the procedure; there may be a little vaginal bleeding following the procedure. Breast and nipple stimulation Breast stimulation is thought to work by stimulating the release of oxytocin from the posterior pituitary. There are case reports of nipple stimulation being associated with uterine hypertonus and fetal bradycardia. These same studies suggest that if nipple stimulation is to be advocated as a method of labour induction, continuous fetal monitoring should be employed at the same time. The studies that look at larger groups employing such techniques are fraught with technical difficulties and at best are difficult to interpret and at worst, meaningless. If the woman gives her consent for a membrane sweep, the procedure should be performed with gentleness and consideration. If consent is not given, the membranes should not be swept under any circumstances. Hygroscopic and mechanical dilators Sexual intercourse Semen is rich in naturally occurring prostaglandins; however, there is little evidence to support the belief that sexual intercourse enhances cervical ripening. This procedure involves passing a finger through the cervical os, sweeping it around the internal surface of the cervix and gently pushing the membrane surface away. It is recommended that all women be offered membrane sweeping prior to induction of labour (see below under Further reading), as it is associated with: increased likelihood of spontaneous labour within 48 hours (63. Hygroscopic dilators work by absorbing water by osmosis, with a resulting change in their size and shape. When placed into the cervical canal over a period of hours (>12 hours often overnight), they produce a mechanical dilatation, which then permits an amniotomy to be performed. These agents may also stimulate the local release of prostaglandins, which may have additional benefits on cervical ripening. Balloon devices and Foley catheters placed within the cervical canal in an attempt to dilate the cervix mechanically have also been investigated. As with the hygroscopic devices, they have been shown to be effective in facilitating cervical dilatation, but overall have not improved the number of successful labour inductions. One or more hygroscopic agents are then inserted into the cervical canal as judged appropriate by the cervical state, and left in situ for the period of time necessary to provide the required improvement in the cervical condition. Synthetic polyvinyl alcohol polymer sponges impregnated with magnesium sulphate (Lamicel) and the polyacrylonitrite tents are more rapidly effective than their naturally occurring counterpart (Laminaria Tent) [B]. Once the cervix has reached the required dilatation, the induction may be advanced by amniotomy and/or the administration of oxytocin. However, with any intracervical device, concerns regarding the introduction of iatrogenic infection have been raised. This risk probably Induction of labour 347 increases in proportion to the duration of retention of any mechanical device, and consequently careful monitoring of the maternal pulse and temperature and the fetal heart rate must be undertaken. While there may appear to be few indications for such interventions, as the efficacy, and safety, of prostaglandins make them almost redundant, their use in situations where prostaglandins have failed makes them a technique worth knowing about. This technique appears to be equally effective at inducing labour as topical prostaglandins, with no difference in the incidence of maternal or neonatal infectious morbidity between the groups. There may be a trend towards an increase in the rate of caesarean section with the infusion intervention, although the studies to date have been too small to assess the clinical significance of this. Not only do they modify the ground substance within the cervix, increasing its compliance, they also stimulate the onset of uterine contractions, and thus induce labour. They are therefore particularly useful for labour induction where the cervix is unfavourable.
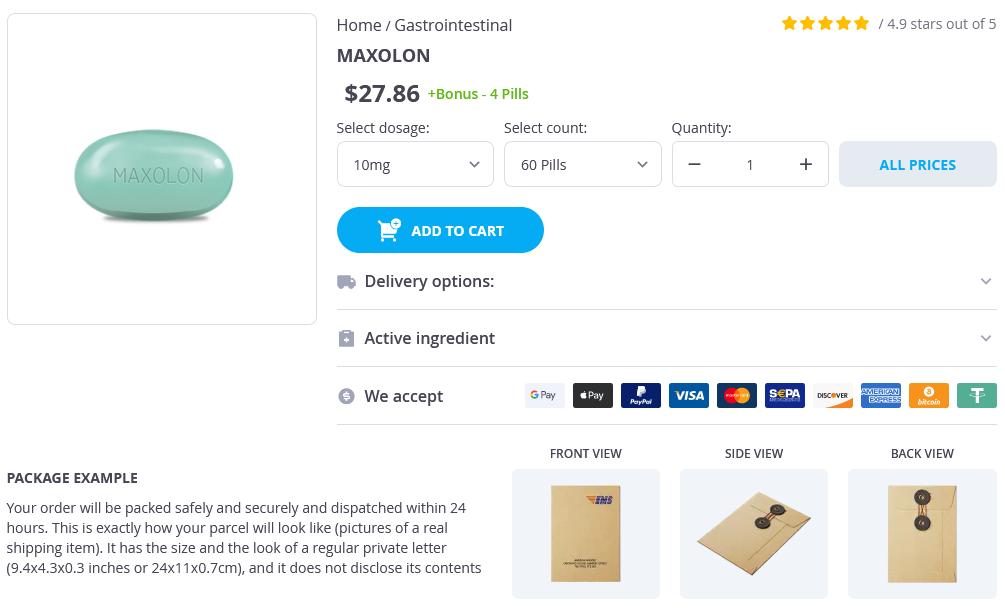
Maxolon Dosage and Price
Maxolon 10mg
- 60 pills - $30.96
- 90 pills - $41.80
- 120 pills - $52.63
- 180 pills - $74.30
- 270 pills - $106.81
- 360 pills - $139.32
Combined images of the upper outer quadrant show the margins of the lipoma (arrows) gastritis diet foods list quality 10mg maxolon. The mass created by the lipoma pushes the thin hyperechoic parenchymal lines (representing lobular regression) superiorly. This image is intended to demonstrate the normal architecture of the fatty breast parenchyma. However, occasionally, a patient is referred for sonography for a palpable fatty mass that has not been mammographically characterized. In these cases it is important to be familiar with the sonographic appearance of fatty masses and recommend mammography to confirm the benign identity of the mass. However, this case emphasizes that lipomas do not have the same internal architecture as normal fatty parenchyma. The echogenic lines within the lipoma do not follow a normal pattern of lobular regression. Histologically, these tumors are composed of mature lipocytes surrounded by a capsule. Upon discovery of a sonographic nodule, mammographic examination has been performed. A well-defined oval nodule corresponds to the palpable lump and the oval mammographic lucency. In real time this heterogeneous mass moves with changes in patient position and floats to the top of the fluid. The oil cyst represents fat necrosis that resulted from removal of the previous implant. When the oil cyst is not calcified, sound transmission is generally increased or unchanged. New York: Thieme; 1997:280316 6 Circumscribed Masses: Medium- or High-Density Masses Case 6. The spot compression views demonstrate that the margins of the right mass are well defined, and the margins of the left mass are ill defined. Pearls and Pitfalls · Uniformly hyperechoic sonographic masses are generally benign, but the category 4 (suspicious) assessment is based upon the information that the masses are new and the left mass is mildly ill-defined mammographically. Microscopically, the mass consists of mature lipocytes associated with an extensive vascular network. Part of its margin is obscured by surrounding dense tissue, and part of the margin is associated with a lucent halo. This entity is considered a physiologic developmental process in which there is cystic dilatation of the terminal duct/lobular units. As a result of this origin, the cysts are lined either with epithelial-myoepithelial cells or by metaplastic apocrine cells. As long as the wall of the cyst is well defined, thin, and hyperechoic, small moving particles within a cyst are generally not clinically significant. Detection and classification of liquid-filled masses in the breast by gray scale echography. Stamford: Appleton and Lange; 1999:115204 Medium- or High-Density Masses 59 Case 6. The fluid collections are anechoic; have well-defined, thin, hyperechoic walls; and have increased acoustic transmission. This process has been identified clinically in about one third of women between 20 and 45 years of age. Autopsy studies have found approximately 54% of normal breasts have histologic evidence of cystic changes. Incidence of chronic cystic disease in so-called normal breasts: a study based on 225 postmortem examinations. Physical Examination · No new breast lumps; both breasts normally lumpy Mammogram Mass. The mammographic mass corresponds to a well-defined sonographic mass that is predominantly isoechoic to fat with a few anechoic oval lucencies within it. Pearls and Pitfalls · Sonography usually is successful in identifying benign cysts. However, if the material does not move, then an intracystic mass should be considered. In these cases, either aspiration or biopsy should be performed to identify intracystic tumors; 75% of solid intracystic masses are benign (mostly papillomas), 20% are malignant, and 5% are phyllodes tumors. With high frequency, the palpable mass attenuates the sound so only a heavily shadowing area is evident. The mass has a predominantly hyperechoic periphery with multiple linear lucencies centrally. Pearls and Pitfalls · Occasionally, diabetes will affect the breast, causing diabetic mastopathy. Microscopically, diabetic mastopathy consists of perivasculitis, keloidlike fibrosis, and ductitis or lobulitis. However, this presentation in a young woman who has had long-term insulin dependence should be a strong clue to the diagnosis. Diabetic mastopathy, complication of type 1 diabetes mellitus: report of two cases and a review of the literature. Physical Examination · Left breast: palpable lump in left lateral breast · Right breast: normal exam Mammogram Mass. The spot compression view demonstrates that the mass has well-defined margins and a lucent halo around part of the C border. Even though this lump was palpable, we chose short term follow up since the mass appeared sonographically to probably be benign. Pearls and Pitfalls · In retrospect, the sonographic appearance of the mass correlates well with the histology as small cysts are evident within the lesion.