Meclizine
General Information about Meclizine
Meclizine works by focusing on the vestibular system, which is liable for sustaining balance and regulating eye actions. By blocking the results of histamine on the vestibular system, Meclizine helps to alleviate the symptoms of motion sickness, making lengthy journeys more bearable for people who endure from it. It can be prescribed for other types of dizziness and vertigo, in addition to for nausea and vomiting related to internal ear diseases and circumstances similar to Meniere's disease.
One of the primary advantages of Meclizine is that it does not trigger drowsiness, in contrast to other drugs used for movement sickness, similar to dimenhydrinate and scopolamine. This makes it a more appropriate possibility for people who need to remain alert while traveling or performing day by day activities. However, drowsiness can occur if greater than recommended doses are taken, so you will need to comply with the instructions of a physician or pharmacist when taking Meclizine.
While Meclizine has been deemed secure and effective for the therapy of motion illness in most individuals, it will not be suitable for everyone. People with certain medical situations, similar to glaucoma, asthma, or enlarged prostate, may have to consult with their doctor earlier than taking Meclizine. It can also interact with other medications, so it is important to tell a doctor about some other drugs being taken.
Another benefit of Meclizine is its long duration of action. A single dose can final for up to 24 hours, making it convenient for lengthy journeys or if symptoms are expected to persist for an prolonged period. It can also be available in several dosage varieties, including tablets, chewable tablets, and oral disintegrating tablets, making it appropriate for adults and children of varying ages.
Meclizine, additionally recognized by its model name Antivert, is a drugs that's extensively used for the prevention and treatment of nausea, vomiting, and dizziness caused by movement sickness. It belongs to a category of medicine referred to as antihistamines, which work by blocking the results of a chemical referred to as histamine within the body. Meclizine is commonly recommended by medical doctors and trusted by travelers as a secure and effective approach to fight the disagreeable symptoms of movement illness.
Motion illness is a standard situation that impacts many people when traveling by automotive, boat, aircraft, or practice. It is brought on by a disagreement between the eyes, inside ear, and sensory nerves, which might happen as a end result of movement, such as the rocking of a boat or the turbulence of a aircraft. This disagreement can lead to symptoms similar to nausea, vomiting, and dizziness, which may make touring a miserable experience for some people.
In conclusion, Meclizine is a broadly used medicine for the prevention and treatment of movement sickness. Its effectiveness, long duration of motion, and minimal side effects have made it a popular alternative among travelers and medical doctors alike. However, it's at all times essential to comply with the directions of a healthcare skilled and to use it responsibly to ensure its most advantages and safety. So, the next time you plan a visit, don't let the concern of motion illness maintain you again. Ask your physician about Meclizine and experience a cushty and pleasant journey.
As the sciatic nerve or its branches cross both the hip and the knee joints treatment ingrown toenail order meclizine with a visa, limited extension and flexion of these joints should be considered. Neither extension nor flexion of the hip increases the risk of femoral neuropathy. Chest rolls should be used in the laterally positioned patients, which might decrease the risk of upper extremity neuropathy. Padding at the fibular head (peroneal nerve) may decrease the risk of peroneal neuropathy. Equipment: the use of an adequately fit and properly functioning automated blood pressure cuff on the arm placed above the antecubital fossa does not change the risk of upper extremity neuropathy. Shoulder braces used during a steep, head-down position may increase the risk of perioperative neuropathies. Management Unresolved nerve injuries should be managed by consulting a neurologist within 48 h. Perioperative Peripheral Neuropathies from Surgical Positioning Nerve injury related to positioning while under anesthesia is a significant source of morbidity for patients. The most common nerve injury in a lower extremity associated with the lithotomy positioning is the superficial peroneal nerve that is vulnerable to compression from stirrups along the lateral aspects of the knee. Mechanism of Nerve Injury Nerve injury related to positioning during general anesthesia results from excessive pressure/compression, ischemia, stretching of nerves, toxins, metabolic/microvascular derangements due to coexisting diseases (preexisting neuropathy, diabetes, hypertension, smoking, alcohol dependence), and direct trauma of the nerve and unknown factors. Other risk factors also included the male gender, a very thin or obese body habitus, and a hospital stay greater than 14 days. It is postulated that excessive sternal retraction is a commonly accepted risk factor. Postoperative assessment: A simple postoperative follow-up and assessment of extremity nerve function may lead to early recognition of peripheral neuropathies. Documentation of specific perioperative positioning actions may be useful for continuous improvement processes and may result in improvements to patient care. During open cardiac surgeries proper vigilance should be taken to minimize sternal retraction during internal mammary artery harvesting to reduce brachial plexus injury. Surgical fires can occur with or without warning; they generate tremendous heat, oftentimes leading to burns. The fire triangle includes that of an oxidizer, fuel, and an ignition source [14]. A common characteristic of a surgical fire is the use of supplemental oxygen via an open delivery system into an enclosed space (drapes), thus creating an oxygen-rich atmosphere close to an ignition source: 5 Oxidizer: oxygen and nitrous oxide supports combustion. Prevention Management Within 48 h, unresolved nerve injuries should be managed effectively by a consulting neurologist and followed up with nerve conduction studies to rule out pre-existing neuropathy. The anesthesiologist should identify an oxygen-rich environment and assess the need by considering the risk benefit ratio to minimize the fraction of inspired oxygen (FiO2). During laser surgeries, the surgeon needs to minimize misdirection of the laser both inside and outside of the operative field. Fire secondary to the use of carbon dioxide absorbents can be avoided by replacing desiccated absorbent. Nerve Injury Related to Peripheral Nerve Block the incidence of a nerve injury from a peripheral nerve block is low, ranging from 2:1000 to 4:1000. The common nerves damaged in descending order are the brachial plexus, median, ulnar, and radial. Mechanisms of nerve injury include mechanical and injection injury (traumatic), vascular (ischemic), chemical (neurotoxic), and inflammatory injuries. Risk factors for peripheral nerve injury includes anesthetic risk factors, surgical factors and patient factors: 5 Anesthetic factors Needle injury, intraneural injection, catheter trauma, hematoma, epinephrine use, and local anesthetic toxicity. Intraneural injections can cause direct needle and injection trauma, rupture of the perineurium, and loss of the protective environment within fascicle, with consequent myelin and axonal degeneration. Ultrasound guidance has not proven to reduce the incidence of peripheral nerve injuries associated with regional anesthesia. However, there is evidence of ultrasound guidance reducing the incidence and intensity of hemidiaphragmatic paresis, but not eliminating it [13]. However, no studies have proven that exposure to a trace concentration of currently used inhalational anesthetics including isoflurane, sevoflurane, desflurane, and nitrous oxide result in adverse health effects. For halogenated agents, no worker should be exposed to concentrations of those gases greater than 2 ppm for a period of more than 1 h. As the core temperature decreases at a slower rate and proceeds in a linear manner as heat lost from the body through radiation, evaporation, conduction, and convection exceeds heat production. Adverse effects of perioperative hypothermia [19] are as follows: 5 Cardiovascular morbidity. Mild hypothermia can result in tachycardia, hypertension, increased peripheral vascular resistance, and myocardia ischemia. Use of patient warming systems, such as forced-air and resistive heating, fluid warmers, to warm fluids being given to patients 28. Core temperature monitoring sites include the pulmonary artery, tympanic membrane, distal end of esophagus, and the nasopharynx. Hypothermia is classified into mild (3235 °C or 3236 °C), moderate (28 32 °C), and severe hypothermia (< 28 °C). It is the most common perioperative temperature disturbance that results from a combination of exposure to a cold operating room environment and anesthetic-impaired thermoregulation.
Gas-Collecting Assembly the gas-collecting assemblies are the points of waste gas exit from the breathing circuit to the transfer tubing my medicine buy meclizine 25 mg with amex. Transfer Tubing the transfer tubing carries excess gas from the gas-collecting assembly to the scavenging interface. The tubing must have 30-mm connectors on either end, which are distinct from the 22-mm connectors on the breathing system tubing. The tubing must be sufficiently rigid to prevent kinking to minimize the chance of occlusion, or it must contain pressure relief in case of occlusion. Occlusion or kinking can increase the pressure in the breathing circuit and barotrauma. Waste-Gas Scavenging Systems the tubing for the scavenging systems has an internal diameter of either 19 mm or 30 mm, compared with the 22-mm anesthesia circuit and ventilator tubing and the 15-mm common gas outlet and tracheal connectors. The scavenging system interfaces with the hospital suction system to remove gas flow from the patient circuit. Thus if the systems are not connected to negative pressure (suction), excess pressure in the interface caused by gas entering it from the circuit would first cause distension of the interface reservoir bag, then the excess would be vented via the position pressure-relief valve at about +5 cm H2O. In the event that excessive suction might be applied to the circuit, the reservoir bag would first be sucked empty, and then 1 (Ohmeda interface) or 2 (North American Dräger closed interface) negative pressure-relief (pop-in) valves (-0. Many contemporary anesthesia machines contain openreservoir scavenging interfaces, are valveless, and use continually open ports to provide pressure relief. Waste gas from the circuit is directed to the bottom of the canister, and the hospital suction system aspirates gas from the bottom of the canister. Therefore, the vacuum rate should exceed the rate of waste gas flow into the chamber, and some room air should also be drawn into the canister through the relief port. This interface system depends on relief ports for pressure relief, so these ports should remain unoccluded at all times. In addition, if vacuum flow is inadequate, waste gas can spill out into the room through the relief ports. Collectively, if the valves in a closed interface or the ports in an open interface become occluded, an excess of positive or negative pressure could develop in the circuit. Gas Disposal Assembly Conduit on Extract Flow the gas disposal assembly conduit conducts waste gas from the scavenging interface to the receiving end of the gas disposal system. It should be collapsible-proof and should run overhead if possible to minimize the chance of accidental occlusion. An Active or Passive Disposal System An active system relies on a hospital central evacuating system to remove gas from the scavenging system. They measure the oxygen concentration within the inspiratory limb of the anesthesia breathing system or within the fresh gas mixture. Hypercarbia 5 Flow from the anesthesia machine inadequate ventilation and hypercarbia (. There are 4 electrical outlets on the anesthesia machine into which additional equipment can be plugged. Variable bypass refers to carefully regulating the concentration of vaporizer output by diluting gas after it is fully saturated with anesthetic agent with a larger flow of gas. Vaporizer concentration control dials are labeled to set vaporizer output in terms of volume percent (v/v%), and the vaporizers are calibrated at sea level. The presence of a wicking system in the vaporizing chamber helps to saturate the fresh gas that is diverted to the chamber. The fresh gas is flowing over the liquid agent therefore it is called flow-over vaporizer. Of note, the vaporizer is agent-specific as the physical properties and clinical concentrations of each agent are unique, therefore the concentration-specific diverting ratios are agent-specific. The evaporation of liquid anesthetic requires energy, which is referred to as the latent heat, which is the number of calories required to change 1 g of liquid into vapor without change in temperature. This energy loss can lead to sig- nificant decreases in temperature within the remaining liquid, which will reduce vapor pressure and subsequent vaporization. Therefore, vaporizers are constructed of metals that have relatively high thermal conductivity, which helps them maintain a uniform internal temperature during evaporation by allowing them to absorb environmental heat more effectively. The modern vaporizers are temperature compensating, therefore they are equipped with an automatic temperature-compensating device that helps maintaing constant vaporizer output over a wide range of operating temperatures by automatically altering the ratio of gas flowing to the bypass and vaporizing champers. When temperature increases, the valve in the bypass opens wider to create a higher splitting ratio (see Appendix) so that more gas flows through and less gas enters the vaporizing chamber. Some older vaporizers had the temperature sensitive valve in the form of a gas-filled bellows linked to a valve in the bypass gas flow. As the temperature increased, the bellows expanded, causing the valve to open more the bypass channel. Contemporary vaporizers use a bimetallic strip for temperature compensation that is incorporated into a flap valve in the bypass machine. This metallic strip is composed of 2 metals with different coefficients of expansion, or change of unit length per unit change of temperature. Nickel and brass have been used in bimetallic strip valves because brass has a greater coefficient of expansion than nickel. As temperature increases, one surface of the flap expands more than the other, causing the flap to bend in a manner that opens the valve orifice wider, increasing the bypass flow. Some machines include a one-way check valve before the breathing circuit inlet to minimize the pumping effect. Impact of Carrier Gas Composition Variable bypass vaporizer output can be influenced by the composition of the fresh gas as a result of differences in solubility of anesthetic vapors specially using nitrous oxide. Nitrous oxide is more soluble than oxygen in the halogenated liquid that results in reducing the carrier gas flow rate vaporizer output. However, once the anesthetic liquid becomes saturated with nitrous oxide, vaporizing chamber output increases, and a new steady state is established. Impact of Gas Flow Rate Vaporizer output can vary with the extreme rates of gas flowing through the vaporizer.
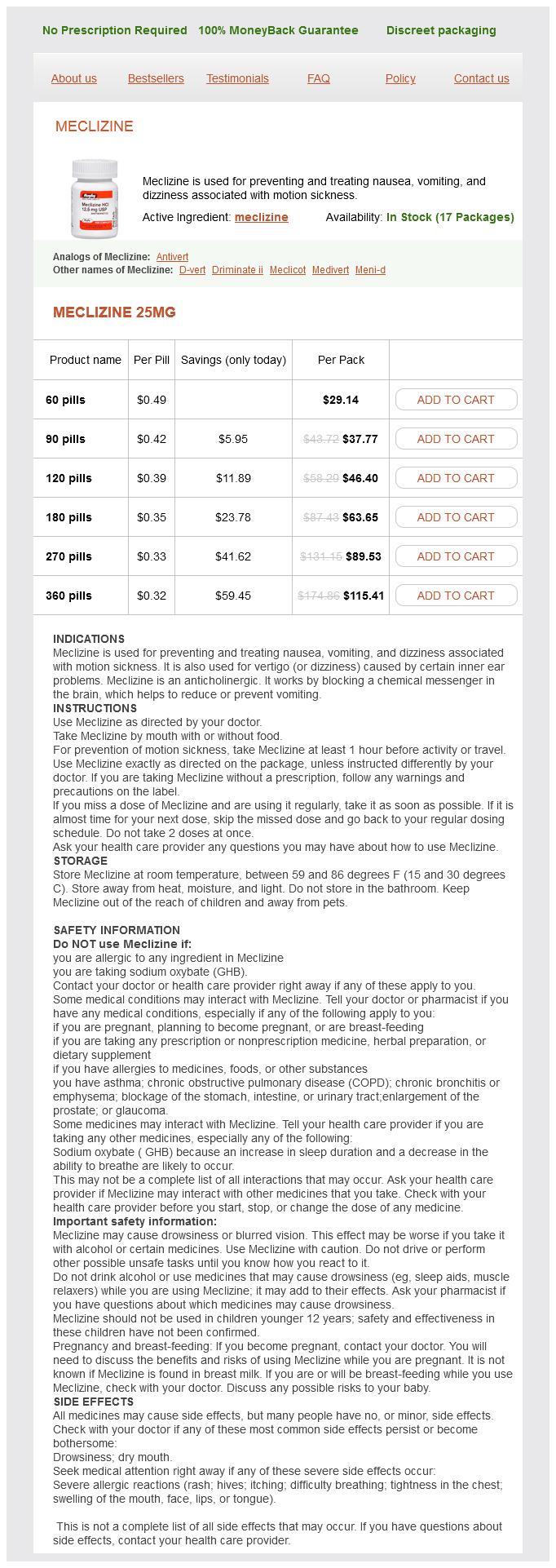
Meclizine Dosage and Price
Meclizine 25mg
- 60 pills - $29.14
- 90 pills - $37.77
- 120 pills - $46.40
- 180 pills - $63.65
- 270 pills - $89.53
- 360 pills - $115.41
Finally medicine 4 you pharma pvt ltd order 25 mg meclizine, the pathway with the shorter refractory period (alternate pathway, pathway B) must conduct impulses more slowly than pathway A. Once an extra impulse (for example, premature contraction) encounters these 2 separate pathways of conduction when pathway A is unable to be depolarized due to being in the refractory period but pathway B is capable of depolarization, the impulse will be conducted via pathway B. The signal then travels to the distal end of pathway A to reconnect with it if it is no longer refractory, then it is conducted retrograde to the site where it reconnects with pathway B. Pathway B has a shorter refractory period and therefore it recovers faster: the impulse will travel into pathway B where it will reenter that portion of the circuit, completing the loop. Macro-reentry occurs via conduction through concealed accessory pathways, such as in Wolff-Parkinson-White syndrome. Classification Class I Class I antiarrhythmic drugs are fast Na-channel inhibitors. Fast sodium channels are blocked during phase 0 (upstroke) and phase 4 depolarization of the action potential with resultant decreases in the amplitude and rate of the action potential and conduction velocity. The most widely used classification system of antiarrhythmic drugs was proposed by Vaughan Williams. This system classifies the antiarrhythmic agents based on their ability of abolishing an arrhythmia by blocking specific ion currents during the action potential. During the upstroke phase (phase 0) of the action potential the channels are in the activated state. During the plateau phase of repolarization (phase 2), the inactivated state occurs: During the effective refractory period channels are unresponsive to new or continued stimulus. The effects on the action potential and the effective refractory period of the cardiac action potential determine the clinical effect of antiarrhythmic drugs. Drugs blocking inward sodium ion flow will slow conduction and result in suppression of the maximum upstroke velocity of the cardiac action potential. L and T type calcium channels are present in the myocardium, and are targets of calcium channel blockers. These drugs lengthen both the action potential and the effective refractory period reflecting sodium channel inhibition and lengthening of repolarization reflecting potassium channel blockade. It increases refractoriness and can prevent accessory pathway re-entry tachycardias. High serum levels may cause direct myocardial depression and bradycardia requiring temporary pacing or administration of beta-agonists. They shorten action potential duration and refractory period in normal ventricular myocytes. In the ischemic tissue, lidocaine may block adenosine triphosphate-dependent channels, preventing ischemicmediated shortening of ventricular depolarization. Lidocaine depresses the slope of phase 4 depolarization in Purkinje fibers and increases the fibrillation threshold in ventricular myocytes. They markedly decrease the rate of phase 0 depolarization and speed of conduction. They have little effect on the duration of the action potential and the effective refractory period in ventricular muscular cells, but do shorten the duration of the action potentials in the Purkinje fibers. This inhomogeneity on the rate of cardiac repolarization plus the slowing of cardiac conduction may contribute to the prodysrhythmic effects of these drugs particularly in patients 204 M. Bauer with history of myocardial infarction, left ventricular dysfunction, or previous sustained ventricular tachycardia. Betaadrenergic receptor antagonists decrease the rate of spontaneous phase 4 depolarization, important in suppression of ventricular arrhythmias during ischemia and reperfusion. They are effective in the treatment of adrenergically mediated disease states, in which increased phase 4 depolarization, enhanced conduction velocity, and a shorter refractory period all contribute to increased automaticity. Beta-blockers decrease the rate of Vmax of the action potential, prolongs its duration as well as the effective refractory period. Druginduced slowing of the heart rate with resulting decreases in myocardial oxygen requirements is desirable in patients with coronary artery disease. Esmolol is used to convert atrial fibrillation with rapid ventricular response to normal sinus rhythm, or to maintain a slow ventricular rate. It also predictably reverses the fibrillation threshold lowering effects of catecholamines. These drugs prolong cardiac repolarization, action potential duration, and the effective refractory period possibly by interference with sodium and calcium exchange. These effects are beneficial in preventing cardiac dysrhythmias by decreasing the proportion of the cardiac cycle during which myocardial cells are excitable and susceptible to a triggering event. Reentrant tachycardias may be suppressed if the action potential duration becomes longer than the cycle length of the tachycardia circuit. It is an - and -receptor antagonist with potent vasodilating and myocardial depressant potential. It may produce sinus bradycardia or heart block, necessitating administration of positive chronotropes or initiation of temporary pacing. Long-term side effects include pulmonary fibrosis, corneal microdeposits, liver cirrhosis, hyperthyroidism, or hypothyroidism. The L isomer of sotalol acts as a beta antagonist, whereas the D isomer may increase mortality in patients with ventricular dysfunction and recent myocardial infarction. Sotalol lacks intrinsic sympathomimetic activity or membrane-stabilizing properties. Prodysrhythmic Effects Prodysrhythmia effects of antiarrhythmic agents describe bradydysrhythmias or tachydysrhythmias that represent new dysrhythmias associated with chronic antidysrhythmic drug treatment. Ventricular tachycardia due to this mechanism is generally slower because of the drug effect, but may be resistant to drugs or electrical therapy. Wide complex rhythm is thought to reflect a reentrant tachycardia and easily degenerates to ventricular fibrillation. The ratio of oxygen consumption to the oxygen available to tissues is the oxygen extraction ratio, which varies for different organs.