Mectizan
General Information about Mectizan
Mectizan belongs to a category of medicine known as macrocyclic lactones, which work by paralyzing and killing the parasites, thus eliminating the infection from the body. It is a broad-spectrum drug, that means it can kill a broad range of parasites. This makes it a extremely versatile and effective drug for treating numerous parasitic infections.
Moreover, Mectizan has also been instrumental in controlling the spread of lymphatic filariasis, a parasitic illness transmitted by mosquito bites. This illness causes extreme and infrequently irreversible swelling of limbs and genitalia, often recognized as elephantiasis. In mixture with another drug, albendazole, Mectizan has been used in mass drug administration programs to stop the transmission of the disease. The success of this strategy has resulted in the World Health Organization (WHO) setting a objective to get rid of lymphatic filariasis by 2020.
Although Mectizan is mostly well-tolerated, it might cause some side effects in some individuals, together with nausea, vomiting, diarrhea, and complications. These unwanted effects are often mild and resolve on their very own. However, it's important to consult a well being care provider in the occasion that they persist or are severe.
Mectizan is an FDA-approved drug and has been used safely in hundreds of thousands of people worldwide. However, it must be prevented in folks with sure medical situations, including liver or kidney illness, and those taking sure medicines like warfarin or rifampicin.
One of probably the most important achievements of Mectizan is its function within the elimination of river blindness (onchocerciasis) in various international locations in Africa and Latin America. This disease, caused by the parasitic worm Onchocerca volvulus, can result in visible impairment and blindness. Mectizan has been broadly used in mass drug administration programs to regulate the unfold of this disease. It is given as a single dose each six to twelve months, and significant progress has been seen in the reduction of circumstances of river blindness in endemic areas.
In addition to those major achievements, Mectizan has also been used to treat different parasitic infections similar to scabies, a pores and skin situation brought on by the microscopic mite Sarcoptes scabiei. It is a extremely contagious illness, usually prevalent in overcrowded and unsanitary living circumstances. Mectizan is an effective treatment for scabies, because it kills the mite and its eggs, providing aid from the intense itching and pores and skin irritation.
As with any medicine, it is crucial to take Mectizan as prescribed and to complete the complete course of remedy. Skipping doses or stopping the treatment prematurely can lead to the reoccurrence of the an infection, and in some instances, the development of drug-resistant parasites.
In conclusion, Mectizan, also referred to as Stromectol, is an essential and highly effective drug for the therapy of parasitic infections. Its success in controlling the spread of ailments like river blindness and lymphatic filariasis has been commendable. With continued efforts and the usage of this drug in mass drug administration programs, it's potential to eradicate these parasitic illnesses and enhance the lives of tens of millions of individuals around the world. However, it's essential that Mectizan is used responsibly and as prescribed to make sure its effectiveness and avoid the event of drug-resistant parasites.
Mectizan, also referred to as Stromectol, is an anthelmintic drug used for the remedy of infections caused by sure parasites. Mectizan has been confirmed to be extremely efficient in treating parasitic infections like river blindness, lymphatic filariasis, and scabies. Since its discovery in the Seventies, Mectizan has been used in varied countries across the globe to combat the risk of parasitic ailments.
Foods that are often incriminated in staphylococcal food poisoning include salads infection blood pressure order 3 mg mectizan amex, especially salads containing mayonnaise and eggs; meat or meat products; poultry; egg products; bakery products with cream fillings; sandwich fillings; and dairy products. Foods kept at room temperature are especially susceptible to higher levels of toxin production when contaminated with toxin-producing staphylococci. The enterotoxins do not cause any detectable odor or change in the appearance or taste of the food. Symptoms appear rapidly (approximately 2 to 8 hours after ingestion of the food) and resolve within 24 to 48 hours. Although no fever is associated with this condition, nausea, vomiting, abdominal pain, and severe cramping are common. Death from staphylococcal food poisoning is rare, although such cases have occurred among elderly patients, infants, and severely debilitated individuals. The organisms gain entrance to the bloodstream via contaminated needles or from a focal lesion present on the skin or in the respiratory or genitourinary tract. These variants are adapted for intracellular growth and are more difficult to detect on laboratory media. Staphylococcal pneumonia has been known to occur secondary to influenza virus infection. Pneumonia, which develops as a contiguous, lower respiratory tract infection or a complication of bacteremia, is characterized by multiple abscesses and focal lesions in the pulmonary parenchyma. Infants and immunocompromised individuals, such as elderly adults and patients receiving chemotherapy or immunosuppressants, are most affected. Septic arthritis can also occur in patients with a history of rheumatoid arthritis, diabetes mellitus, recent joint surgery, skin infections, or intravenous drug abuse. Some predisposing factors for hospital-acquired infection include instrumentation procedures such as catheterization, medical implantation, and immunosuppressive therapy. Infections associated with the use of implants, such as indwelling catheters and prosthetic devices, are often caused by isolates shown to produce a biofilm. Biofilm production is a key component in bacterial pathogenesis and is a complex interaction between host, indwelling device, and bacteria (see Chapter 31). This organism is more virulent than other is known to contain the gene mecA, which encodes oxacillin resistance. Other Coagulase-Negative Staphylococci Species less commonly seen but established as opportunistic pathogens include S. A wide range of infections have been associated with these organisms, including endocarditis, septicemia, and wound infections. Although they are not commonly seen as pathogens, their role in some infections is well established, and they cannot be automatically discarded as contaminants. The first human case was endocarditis in a patient after the implantation of a cardioverter-defibrillator device. Subsequently, other human infections reported sporadically have included surgical site infections, rhinosinusitis, and catheterassociated bacteremia. Normal skin biota contamination can be further reduced by the physician submitting secretion aspirates, tissue samples, or blood culture specimens instead of swabs. Numerous grampositive cocci, along with polymorphonuclear cells in purulent exudates, joint fluids, aspirated secretions, and other body fluids, are easily seen when these sites are infected with staphylococci. An aspirate is the best sample, whereas a single swab would be less satisfactory for both culture and smear results. This bacterium has recently been associated with a variety of infections in humans, including surgical wounds. In the Case in Point, the patient had a history of volunteering with a veterinarian. Laboratory Diagnosis Specimen Collection and Handling Proper specimen collection, transport, and processing are essential elements in the correct diagnosis and interpretation of any bacterial culture result. Clinical materials collected from infected sites should be transported to the laboratory without delay to prevent drying, maintain the proper environment, and minimize the growth of contaminating organisms. Identification of staphylococci on the basis of colony morphology alone should not be done. Identification Methods Staphylococci have been traditionally differentiated from micrococci on the basis of oxidation-fermentation (O/F) reactions produced in O/F glucose medium. Staphylococci ferment glucose, whereas micrococci fail to produce acid under anaerobic conditions. However, the O/F tests do not sufficiently discern certain weak acid producers, such as Micrococcus kristinae, and staphylococci that fail to grow or produce acid anaerobically, such as S. Many commercial multitest systems have incorporated these traditional biochemical tests. Clumping factor, formerly referred to as cell-bound coagulase, causes agglutination in human, rabbit, or pig plasma. Clumping factor on the surface of the bacterial cells directly converts fibrinogen to fibrin, which precipitates onto the cell surface, causing agglutination, and this was performed on a glass slide using a heavy suspension of organism mixed with saline and a drop of plasma. A negative result was followed up by a tube coagulase test, which is described later. Because of the insensitivity of this slide test, only the tube coagulase or agglutination tests should be used. On Gram stain, gram-negativelooking cells show how older cells decolorize (×1000). B, Scanning electron micrograph showing the typical "clusters" of staphylococci (×20,000). Modified from Becker K, et al: Staphylococcus, Micrococcus, and other catalase-positive cocci. Laboratorians should look for clot formation after 4 hours of incubation at 37° C. If no clot appears, the tube should be left at room temperature and checked the next day.
Although a few reference laboratories perform mating tests with known tester strains antibiotics for face redness mectizan 12 mg lowest price, this procedure is not regularly performed in clinical laboratories. Most geophilic fungi produce large numbers of conidia and therefore are among the most readily identified species. Zoophilic dermatophytes are not commonly found living freely in soil or on dead organic substrates. They often cause infections in animals and can be spread as agents of disease in humans. Although the anthropophilic species are almost always encountered as agents of human disease, the infections are seldom inflammatory. Species identification may be difficult because most anthropophilic species produce few conidia. Not only are sites diverse on the host involved in infections, but certain species also cause distinctive lesions. Over time, involved portions of the trunk develop diagnostically distinctive concentric rings of scaling tissue. In some forms of ringworm, a persistent allergic reaction, dermatophytid, is manifested in the formation of sterile, itching lesions on body sites distant from the point of infection. Symptoms of dermatophyte infections range from slight to moderate and occasionally severe. Infections Involving Hair Different body sites manifest different symptoms of mycoses. Infections of the scalp, in which hair follicles are the initiation sites, can be among the most severe and disfiguring forms of mycoses. Tinea favosa, or favus, begins as an infection of the hair follicle by Trichophyton schoenleinii and progresses to a crusty lesion made up of dead epithelial cells and fungal mycelia. Two distinct forms of tinea capitis-gray patch ringworm and black dot ringworm-are caused by different species of dermatophytes. Gray patch ringworm is a common childhood disease that is easily spread among children. The fungus colonizes primarily Agents of Cutaneous Mycoses General Characteristics Three genera of fungi-Trichophyton, Microsporum, and Epidermophyton-are causative agents of dermatophytoses. The lesions are seldom inflamed, but luster and color of the hair shaft may be lost. Microsporum audouinii and Microsporum ferrugineum are causative agents of this disease. The hair follicle is the initial site of infection, and fungal growth continues within the hair shaft, causing it to weaken. The brittle, infected hair shafts break off at the scalp, leaving the black dot stubs. Tricho phyton tonsurans and Trichophyton violaceum are the most common fungi implicated in this form of dermatophytosis. Infections Involving Nails Onychomycosis, which is infection of the nails, is most often caused by dermatophytes but also may be the result of infection by other fungi. These nail and nail bed infections may be among the most difficult dermatomycoses to treat. Long-term, costly therapy with terbinafine or itraconazole has been considered the best treatment, but results are often unsatisfactory. There is a direct association between dermatophytic infections of the feet or hands and infections of the nails. It is unlikely that anyone suffering from tinea pedis will escape some extent of onychomycosis. The subungual form is the most common form of onychomycosis, described as lateral, distal, or proximal. Either end of the nail is first infected, with spread continuing to the nail plate. Infection arises from infected skin scales coming into contact with exposed skin via a carpet, shower floors, or other shared walking/ standing surfaces where shoes are not always worn. It is believed that individuals have a genetic predisposition to developing the disease because not everyone encountering infected skin scales becomes infected. Various sites on the foot may be involved, but tinea pedis usually affects the soles and toe webs. In more severe cases, the sole may develop extensive scaling, with fissuring and erythema. The disease may progress around the sides of the foot from the sole, giving rise to use of the term moccasin foot, descriptive of the appearance of the infected area. Infections of the glabrous skin range from mild, with only minimal scaling and erythema, to severely inflamed lesions. Systemic Dermatophyte Infections Immunocompromised persons may suffer systemic dermatophyte infections. In some patients, it manifests itself as granulomas, whereas in others, pea-sized to walnut-sized nodules can develop. Biopsy of these nodules reveals fungal elements that are easily recovered in culture. Epidermophyton floccosum Although Epidermophyton floccosum produces only one size of conidia, these conidia are described as macroconidia because of their size.
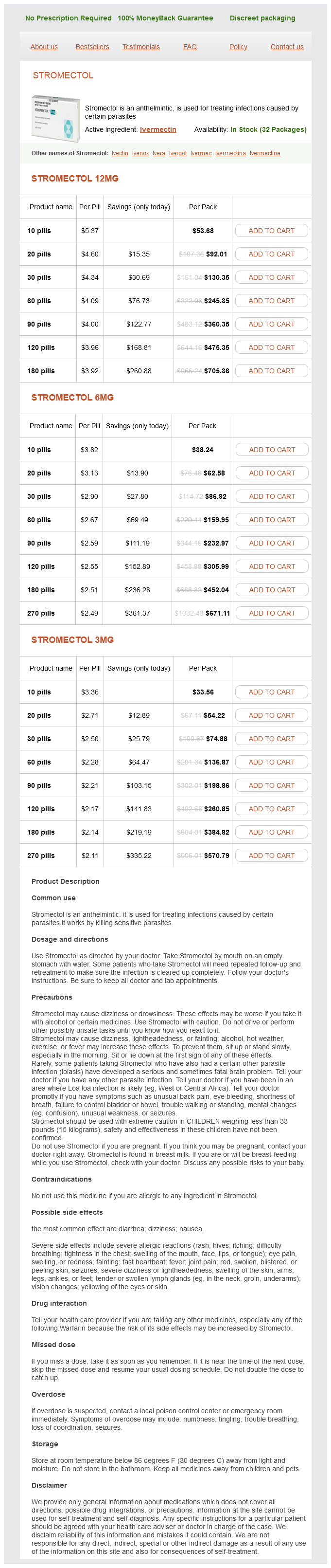
Mectizan Dosage and Price
Stromectol 12mg
- 10 pills - $53.68
- 20 pills - $92.01
- 30 pills - $130.35
- 60 pills - $245.35
- 90 pills - $360.35
- 120 pills - $475.35
- 180 pills - $705.36
Stromectol 6mg
- 10 pills - $38.24
- 20 pills - $62.58
- 30 pills - $86.92
- 60 pills - $159.95
- 90 pills - $232.97
- 120 pills - $305.99
- 180 pills - $452.04
- 270 pills - $671.11
Stromectol 3mg
- 10 pills - $33.56
- 20 pills - $54.22
- 30 pills - $74.88
- 60 pills - $136.87
- 90 pills - $198.86
- 120 pills - $260.85
- 180 pills - $384.82
- 270 pills - $570.79
Secretory antibody antimicrobial yeast buy mectizan mastercard, lactoferrin, and lysozyme are produced by the host as a way to protect against infection. To be successful in establishing infection, infectious agents must be able to avoid or overcome these local factors. Lactoferrin competes with bacteria for free iron, an essential trace element; Neisseria meningitidis can use lactoferrin as a source of iron and is therefore not inhibited by the presence of lactoferrin. The host produces antibodies against the "old" antigens, which are no longer effective because the organism now has "new" antigens that do not bind to antibodies made against the old antigens. In most situations when an organism is engulfed by macrophages, lysosomal contents are released into the phagocytic vacuoles and the organism is killed. However, if the engulfed organism is not exposed to intracellular killing and digestive processes, it is able to survive and multiply inside the macrophage. Bacterial species, such as Chlamydia, Mycobacterium, Brucella, and Listeria species, are easily engulfed by macrophages and phagocytes. With some organisms, the invasion is localized and involves only a few layers of cells. With others, it involves deep tissues; for example, the gonococcus organism is invasive and may infect the fallopian tubes. Other organisms, such as Corynebacterium diphtheriae, do not spread beyond their initial site of infection, yet the disease they produce is serious and often fatal because the exotoxins they produce are disseminated. Certain organisms that survive phagocytosis can be disseminated rapidly to many body sites, but the organisms themselves are not invasive. The phagocyte carries the organism to other body sites, but the bacterium itself is incapable of penetrating tissues. Once bacteria are attached to nonphagocytic cells, phagocytosis by white blood cells is less likely to occur. This damage may be from toxins, either exotoxins or endotoxins, or from inflammatory substances that cause hostdriven, immunologically mediated damage. The ability of organisms to produce exotoxins and extracellular enzymes is another major factor that contributes to the virulence and invasiveness of organisms. Toxins are poisonous substances produced by organisms that interact with host cells, disrupting normal metabolism and causing harm. Exotoxins are produced by both gram-negative and gram-positive bacteria and are secreted by the organism into the extracellular environment, or they are released on lysis of the organism. Exotoxins can mediate direct spread of the microorganisms through the matrix of connective tissues and can cause cell and tissue damage. Some organisms produce soluble substances, such as proteases and hyaluronidases that liquefy the hyaluronic acid of the connective tissue matrix, helping bacteria to spread in tissues, promoting the dissemination of infection. Endotoxins, in contrast to exotoxins, do not have enzyme activity, are secreted in only very small amounts, do not have specificity in their activity on host cells, are not very potent, and are not destroyed by heating. Most are composed of two subunits: one is nontoxic and binds the toxin to the host cells and the other is toxic. Diphtheria toxin inhibits protein synthesis and affects the heart, nerve tissue, and liver. Botulinum toxin is a neurotoxin that blocks nerve impulse transmission, causing flaccid paralysis, especially in infants. The cell wall of gramnegative microorganisms is composed of two layers-the inner peptidoglycan layer and an outer membrane. These are the chemical mediators that produce the effects of endotoxin that consist of dramatic changes in blood pressure, clotting, body temperature, circulating blood cells, metabolism, humoral immunity, cellular immunity, and resistance to infection. Endotoxin stimulates the fever centers in the hypothalamus, increasing body temperature within 1 hour after exposure. Endotoxin exposure also causes hypotension, producing severe hypotension within 30 minutes. In contrast to shock caused by fluid loss, such as shock seen in severe bleeding, septic shock is unaffected by fluid administration. The endotoxin also initiates coagulation, which can result in intravascular coagulation. This process depletes clotting factors and activates fibrinolysis so that fibrin-split products accumulate in the blood. Another feature of patients with endotoxic shock is severe neutropenia, which can occur within minutes after exposure. It results from sequestration of neutrophils in capillaries of the lung and other organs. Leukocytosis follows neutropenia because neutrophils are released from the bone marrow. It stimulates proliferation of B lymphocytes in some animal species, activates macrophages, activates complement, and has an adjuvant effect with protein antigens. Yersinia pestis a Cholera Enteritis Dysentery Plague Toxins that produce harmful effects of infectious disease. A severe infection with gram-negative bacteria can lead to serious and often life-threatening situations. Host Resistance Factors Physical Barriers Humans have evolved a complex system of defense mechanisms to prevent infectious agents from gaining access to and replicating in the body. The stratified and cornified epithelium presents a physical barrier to penetration by most microorganisms.